 |
A 55-year-old woman under management for primary open angle glaucoma for the past 15 years presented for a checkup. Her peak intraocular pressures (IOPs) were 31mm Hg OD and 26mm Hg OS. She had moderate glaucomatous damage to each optic disc.
For the majority of her care, her treated IOP was in the mid-teens with stability in her visual field, optic disc photography and optical coherence tomographic retinal nerve fiber layer. However, over the past two and a half years, her IOP slowly and consistently rose to the mid 20s, despite escalating her therapy to include latanoprost and dorzolamide-timolol FC (she was allergic to brimonidine). Selective laser trabeculoplasty (SLT) lowered her IOP to the upper teens for about a year before she rose again to the mid 20s in her right eye with her left remaining in the high teens.
In this case, medical therapy was maximized and trabeculoplasty already employed. Though apparently stable, the right eye maintaining mid-20s pressure was disconcerting. Repeat trabeculoplasty was not embraced and trabeculectomy and tube implantation were likewise discounted as excessively risky in an eye maintaining an elevated IOP but not yet showing signs of progression. In that she had a mildly symptomatic cataract in her right eye (with 20/30- acuity), it was felt that lens extraction with implantation of an iStent (Glaukos) would be her next best, safest route of pressure reduction. She successfully underwent combined cataract extraction with iStent implantation with a subsequent sustained, medicated IOP of 18mm Hg in that eye.
 |
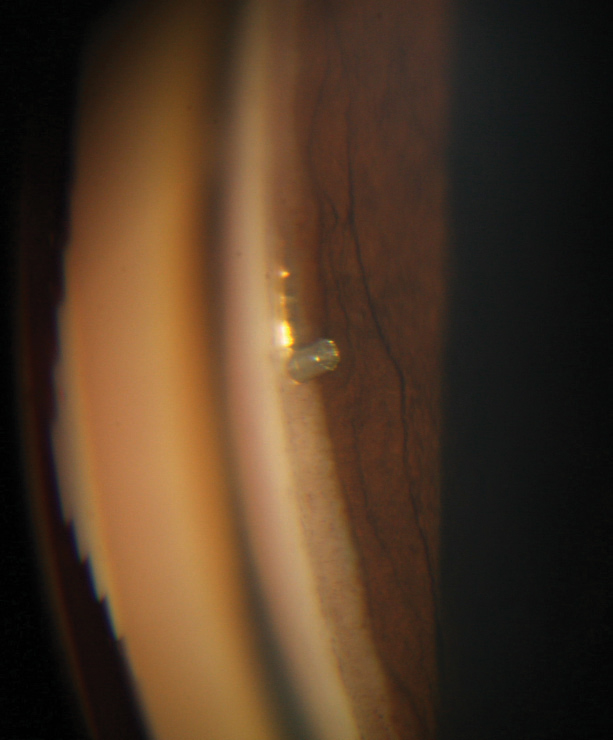
| Under magnification you can see an iStent being inserted through the trabecular meshwork during cataract surgery. Click image to enlarge. |
Two For One
Research shows that modern cataract surgery with phacoemulsification substantially reduces IOP and need for glaucoma medications in many patients.1-3 The exact mechanism of IOP reduction is unknown, though some have speculated that removal of a cataractous lens removes any possible phacomorphic component of IOP rise.
Minimally invasive glaucoma surgeries (MIGS) have gained popularity in cases of glaucoma and co-existent cataract due to its ease of implantation during cataract surgery, favorable safety profile and the possibility for effective and long-lasting IOP reduction. Additionally, patients may also experience a reduced need for IOP-lowering medications.4 This can be especially popular among patients who are non-adherent.
Most MIGS procedures are performed ab interno and microincisional through a clear cornea during cataract surgery. The procedures are minimally traumatic and can be performed coincident with lens extraction. The iStent, specifically, is implanted in conjunction with cataract surgery through the trabecular meshwork and into the Schlemm’s canal.5
Some researchers speculate that increased outflow facility following phacoemulsification solely accounted for the IOP reduction and that the MIGS devices added little in additional IOP reduction.6-8 Indeed, many early reports may have substantiated only a minimal extra IOP reduction through a MIGS procedure.7 However, since these procedures have a substantial learning curve, later results should be considered in judging efficacy.
In the Literature
A recent meta-analysis of 37 studies examining a combined 2,495 patients, iStent with phacoemulsification as compared with phacoemulsification alone, noted 4% IOP reduction from baseline following phacoemulsification alone compared with 9% reduction in IOP following an iStent implant with phacoemulsification.9 This IOP reduction rose to 27% following two iStent implants with phacoemulsification. Compared with cataract extraction alone, iStent with phacoemulsification resulted in significant reduction in the postoperative IOP and a significant decrease in the number of glaucoma medications needed postoperatively. The overall assessment was that iStent with phacoemulsification significantly outperforms phacoemulsification alone in terms of reduction in IOP and postoperative medications being used.9
Other non-comparative studies show positive outcomes, safety and decreased medication burden. A study involving a mainly a Hispanic population with predominantly moderate or severe glaucoma shows a substantial reduction of IOP and medication need and favorable safety for a year following stent implantation during cataract surgery. At one year, 94% of eyes in that study achieved their predefined treatment goal of reduced IOP and/or medications. Two eyes had filtering surgery; the remaining 95% avoided such treatment.10
Another prospective, open-label, non-randomized study evaluating long-term safety and efficacy of iStent trabecular microbypass stent implantation during cataract surgery in patients with primary open-angle, pseudoexfoliation glaucoma, ocular hypertension or secondary or post-traumatic glaucoma saw that the procedure was safe and effective, as measured by a sustained reduction in IOP and medication use and an excellent safety profile through three years after surgery.11
 |
| When implanted, as seen here, the iStent and other MIGS devices are designed to help lower IOP. New research shows how they’re fairing. |
Looking to the Future
While results have been improving as surgeons work through learning curves, future advancements in the iStent trabecular bypass are being developed. Glaukos is currently pursuing FDA approval for a second-generation product called iStent Inject, a new trabecular bypass system that implants two devices, rather than one as with the current iStent. Results of a prospective, randomized, multicenter clinical trial of the iStent Inject were presented at the 2018 American Society of Cataract and Refractive Surgery annual meeting. The device met the study’s primary and secondary effectiveness endpoints. At 24 months, 75.3% of the iStent Inject cohort achieved a 20% or greater reduction in unmedicated IOP, compared with 61.9% for the cataract-only cohort and a mean unmedicated IOP reduction of 6.9mm Hg for the iStent Inject cohort, compared with 5.4mm Hg for the cataract-only cohort.
MIGS procedures are statistically better at reducing medication load and IOP when combined with cataract surgery as opposed to the effects of cataract surgery alone. With surgical experience and advancements in the devices implanted, better IOP outcomes can be expected. Much the same way early glaucoma imaging devices improved diagnosis, but paled in comparison to current technology, we can likely expect that later generation MIGS procedures and devices will exceed those being used today.
Drs. Sowka and Kabat have no financial interest in any products mentioned. Dr. Sowka has previously served in an advisory manner for Glaukos.
1. Armstrong JJ, Wasiuta T, Kiatos E, et al. The effects of phacoemulsification on intraocular pressure and topical medication use in patients with glaucoma: a systematic review and meta-analysis of 3-year data. J Glaucoma. 2017;26(6):511-22. |

