 |
|
Patients with both photophobia and chronic ocular surface pain had higher levels of pain when presented with light stimuli than those with only the former condition. Photo: EyeBrain. Click image to enlarge. |
Central nervous system activity must be evaluated when dealing with patients with ocular pain with neuropathic features. A recent small study found that one imaging technique—functional magnetic resonance imaging (fMRI)—may be useful for assessing photophobia in patients with this condition. The research demonstrated that, in response to a light stimulus, there was greater activation within brain regions associated with pain processing in patients with both photophobia and chronic ocular surface pain vs. those with photophobia alone.
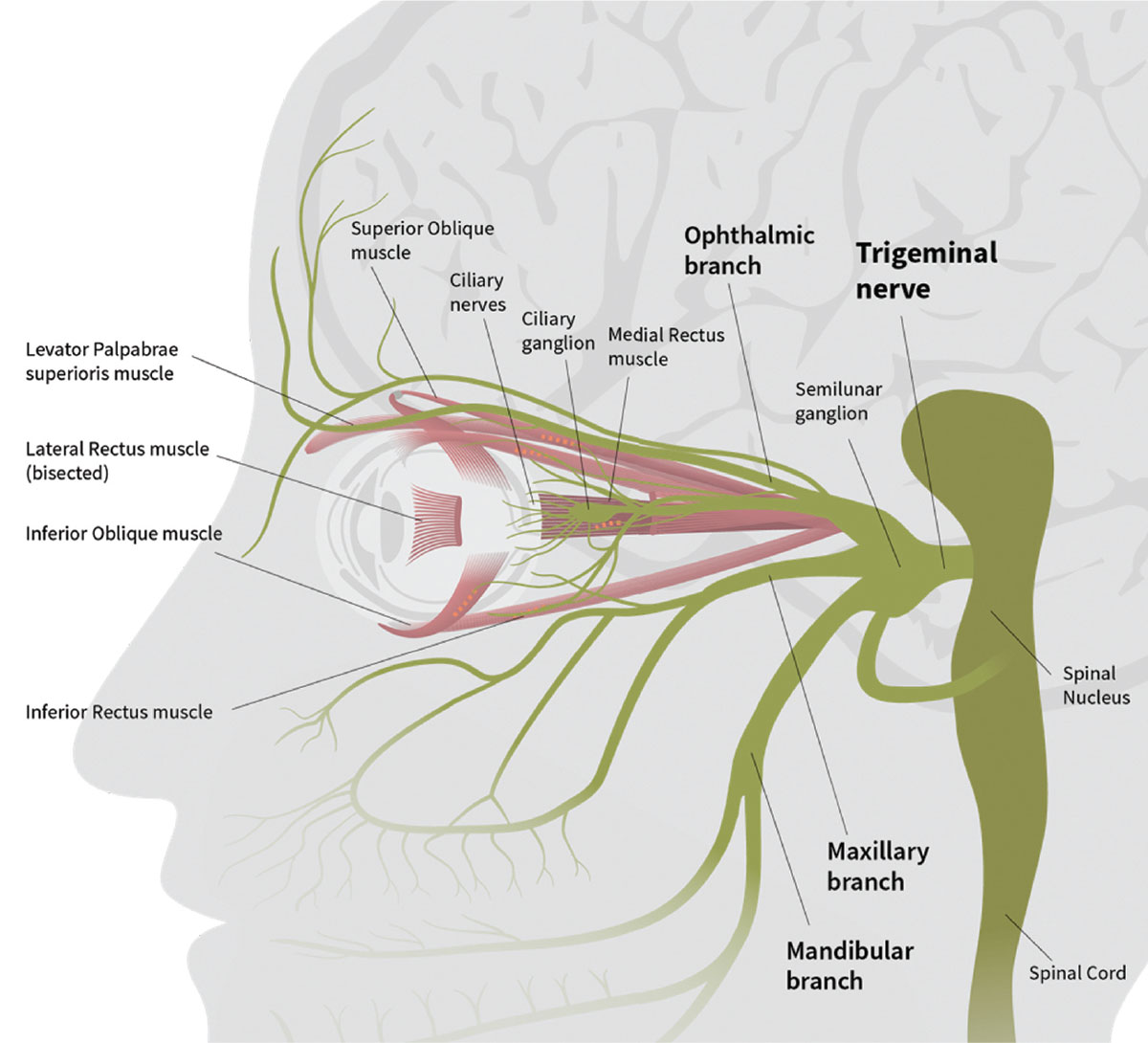
Another major finding of the study: applying anesthetic to the eye appeared to modulate the cortical structures in the trigeminal nociceptive pathway. The researchers noted in their paper, “These findings support the hypothesis that pathologic central sensitization within the trigemino-cortical nociceptive pathway contributes to photophobia in individuals with chronic ocular surface pain.”
The 16 study participants first completed a set of questionnaires to evaluate pain levels, ocular surface symptoms, dry eye and general health information including medical history. Each participant also underwent a thorough ocular surface evaluation. They were then divided into two groups:
Cases, made up of individuals who reported chronic (≥six months) ocular surface pain and light sensitivity at least most of the time over one week (n=8)
Controls, made up of those who had no chronic ocular surface pain and minimal or no light sensitivity (n=8)
All participants were shown two fMRI scans, one before and one after anesthetic drops were administered. The researchers explained, “During each scan, individuals were presented with two screen conditions: a resting black screen condition, which featured a white fixation cross on a black background (~0.5 lux), and a light stimulus white screen condition, which featured a black fixation cross on a white background (~65 lux).” The white screen was shown 16 times for periods of six seconds each. After the first scan, participants were each given a single eye drop of topical anesthetic 0.5% proparacaine, then the next scan was immediately performed.
After each scan, participants verbally rated their pain intensity when viewing either the black or white screen on a scale of zero (no pain) to 100 (“most intense pain imaginable”). The researchers observed, “Cases reported higher pain intensity ratings than controls in response to light stimuli during fMRI.” Average preanesthetic pain intensity ratings in these participants were also much higher when viewing the light stimulus (white screen: 49) vs. resting (black screen: 18.6). After anesthesia, pain ratings for cases were 38.6 for the light stimulus and 17.5 for rest.
Additionally, the study authors added, “Case ratings correlated more with light-evoked activation in pain-related areas within the trigeminal brainstem, primary somatosensory cortex (S1), anterior midcingulate cortex and insula than with controls.”
The anesthetic appeared to decrease light-evoked activation in the primary somatosensory cortex and anterior midcingulate cortex. The researchers noted, “Although subjective pain responses after anesthetic placement varied between case individuals, reduced cortical activation was observed when examined as a group.”
The researchers concluded that observing activity in the trigeminal nociceptive system may contribute to photophobia in patients with chronic ocular surface pain. Using fMRI to examine these pathways and their responses to medication such as anesthetic may help inform future research and therapeutic development. “Further understanding of modulatory interactions that govern ocular surface pain and photophobia is critical for developing effective, precision-based therapies,” they wrote.
Choudhury A, Reyes N, Galor A, et al. Clinical neuroimaging of photophobia in individuals with chronic ocular surface pain. Am J Ophthalmol. October 9, 2022. [Epub ahead of print]. |

