 |
|
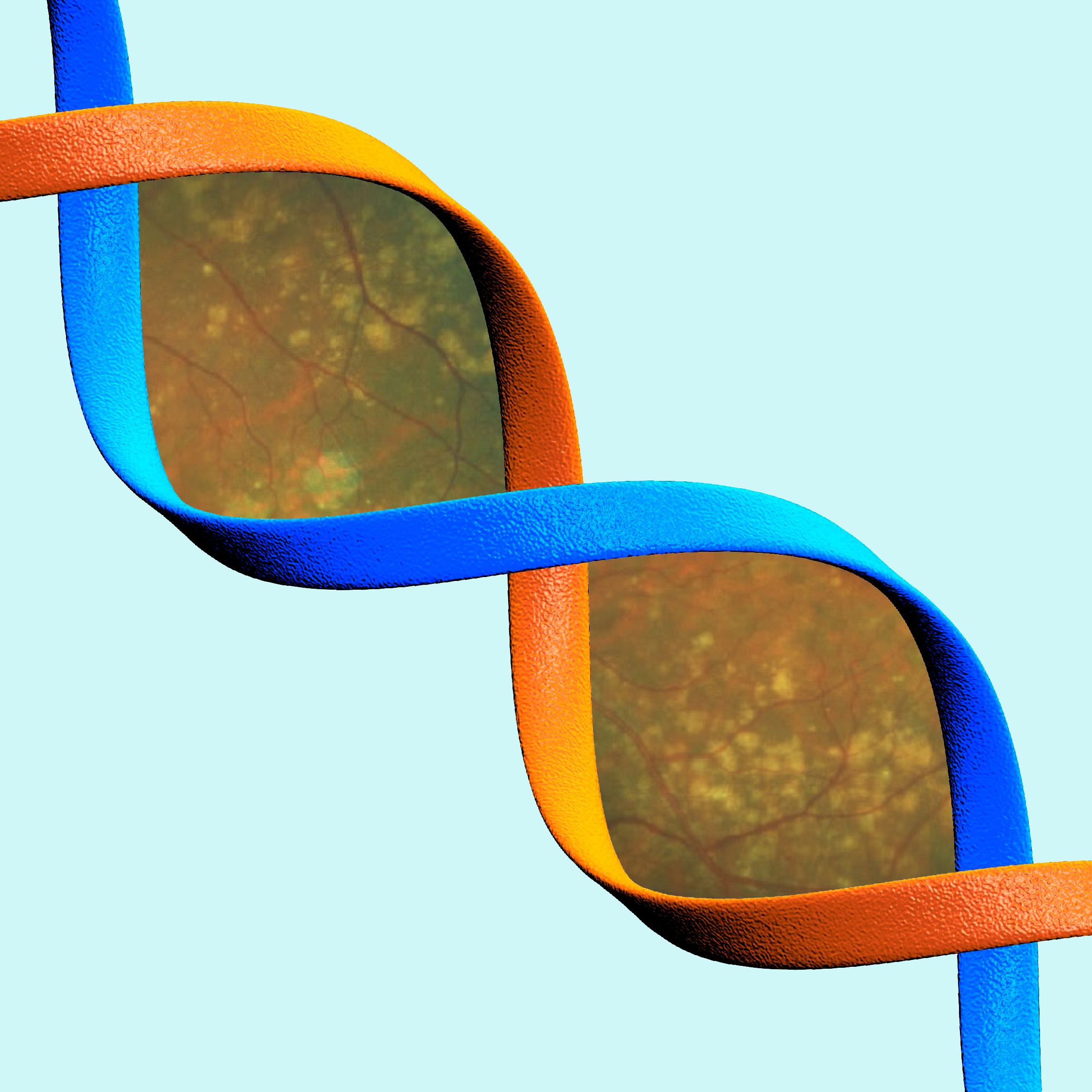
It’s likely that PRS performance for AMD will improve more in the future as the size of genome-wide association studies continue to grow. Photo:Getty Images; Anna Bedwell, OD. Click image to enlarge. |
It’s well-established that there’s a genetic component to AMD pathogenesis, but whether or not that means genetic screenings performed in office can be of diagnostic value has been a matter of debate for many years. Research appearing in Ophthalmology outlines how newly identified genetic risk variants affect the performance of an updated polygenic risk score (PRS2023) when compared with an older one (PRS2016).
An independent cohort of older individuals with retinal imaging data was used, comprising 4,175 total participants, all of European ancestry and aged 70 years or older with this genotype and retinal imaging data from the ASPirin in Reducing Events in the Elderly trial.
Of all the participants, 62.4% had no age-related macular degeneration (AMD), 20.4% had early AMD, 16.1% had intermediate and 1.1% had late-stage AMD. Intermediate or late-stage AMD was seen in more than 27% of participants with a high PRS2023 (top quartile). Comparatively, less than 15% in the middle two quartiles and less than 13% in the lowest quartile had intermediate or late-stage AMD.
Both PRS2023 and PRS2016 were significantly associated with AMD after adjusting for age, sex, smoking status and lipid levels, with increasing odds ratios for worsening AMD grades. With both demonstrating strong associations, this indicates a strong genetic component of the disease. However, the PRS2023 outperformed the older, likely because of a greater number of AMD-associated genetic variants and updated odds-ratios from a larger and more recent genome-wide association study.
The PRS2023 would explain 42.2% of disease liability, assuming a population prevalence of 10% for late-stage AMD. Area under the curve of a model containing conventional/non-genetic risk factors and the PRS2023 was 91% for predicting late-stage AMD, indicating good accuracy. This improved 12% over the baseline model without the PRS (from 79% to 91%). As such, the study authors argue this “demonstrates that an updated PRS for AMD leads to significantly improved prediction of risk and severity, providing strong evidence to support clinical implementation.”
Although area under curve improvement for all AMD was only 3% (from 60% to 63%), late-stage AMD only is when the addition of PRS2023 to the model improved 12%. As well, an increase in late-stage AMD prevalence from Q1 (0.1%) to Q2-3 (0.7%) was observed, then another increase to Q4 (3%). The researchers explain in their paper that, “therefore, our results suggest that the PRS2023 has an ability to predict and distinguish those at greatest risk of progressing to late, vision-threatening disease is a significant advantage of the new PRS when considering clinical utility, patient counseling and identification of high-risk individuals early to enroll into intervention studies.”
Overall, the authors believe “our findings have clinical implications for the improved risk stratification and prediction of AMD, especially for vision threatening late-stage AMD.”
Yu C, Robman L, He W, et al. Predictive performance of an updated polygenic risk score for age-related macular degeneration. Ophthalmology. January 31, 2024. [Epub ahead of print]. |

