Nearly 20% of the U.S. population (approximately 50 million Americans) suffer from some form of allergy, so its not surprising that research continues to focus on treatment options for these individuals.
Dry Eye Contributes To Allergic Response
Patients natural tear production can help eradicate the allergic response. Tears act as a barrier, improving the eyes first line of defense. They dilute and ultimately flush the allergens and mediators from the eye. New evidence shows that tears, or the lack of tears as seen in dry eye syndrome (DES), may contribute to the propagation of the allergic response.
Approximately 15% of people past age 65, and 10% of people past age 30, suffer from DES. And, the majority of patients with baseline chronic dry eye conditions are women. For these patients, symptoms are often exacerbated by attendant factors in the premenopausal and early menopausal stages of life.1
One study confirmed this association by outlining the cycle of tear production associated with corneal surface neural feedback.2 Researchers established that when the ocular surface is dry, a neuro-sensory mechanism activates signals. These signals, in turn, stimulate the lacrimal gland and accessory lacrimal systems to secrete tears.
Persistent ocular surface inflammation may disrupt this feedback loop. Factors that interfere with this feedback system may trigger a vicious cycle of progressive dryness and inflammation.
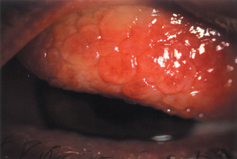
Treating patients in the early phase of allergic conjunctivitis will limit the chances of progression to vernal keratoconjunctivitis, seen here.
Artificial tears should be used in concert with any topical anti-allergy medication. In fact, treatment should be aimed at decreasing the concomitant factors associated with dry eye and SAC/PAC. Oral antihistamines can exacerbate this process, so we do not routinely prescribe these to treat symptoms of ocular allergy.3
A study to be presented at the Association for Research in Vision and Ophthalmology meeting in April challenged 78 allergic rhinoconjunctivitis sufferers with a conjunctival allergen at one visit and a nasal allergen at another. They found that by introducing an allergen to just the ocular surface, they induced all the signs and symptoms of allergic rhinitis and allergic conjunctivitis. This suggests that drainage of allergens and allergic mediators down the nasolacrimal duct spreads the allergic reaction to distal organs. These results highlight the importance of the eye in imitating and propagating the allergic reaction. So, it is appropriate to target the eye for systemic anti-allergy therapy.4
Blocking the Response
Because most allergic signs directly result from histamine release, medications aimed at blocking histamine receptors have also demonstrated effectiveness as a mode of treatment. Newer antihis-tamines such as Livostin (levocabastine, Novartis Ophthalmics) and Optivar (azelastine hydrochloride, ASTA Medica) are more potent and longer-acting compared with some previous formulations. Yet, these medications only serve to competitively and temporarily block the free-floating histamine from occupying the H1 receptor. They will reduce itching and, to some extent, redness. However, these medications will not decrease inflammation or reduce degranulation of the mast cell and subsequent release of more mediators.
Researchers are currently investigating a new FDA-approved antihistamine: Elestat (epinastine, Allergan). A twice-a-day dose was well tolerated, and demonstrated rapid delivery and long duration of efficacy.5 In another study, epinastine statistically was as effective as a bi-modal formulation such as Zaditor (ketotifen fumarate, Novartis Ophthalmics).6
Did You Know . . .
Simply relying on your patients subjective symptoms may not be enough. A 1995 study looked at patients who were diagnosed with rhinoconjunctivitis and found that while patients described their allergic symptoms as minimal, biopsy of the conjunctiva revealed a more vigorous inflammatory process.1313 So, the patients awareness of his or her allergic response may be muted.
Another treatment option is to block the degranulation of the mast cell and stabilize it. However, topical mast cell stabilizers require multiple dosing during the day. Also, patients can develop a tolerance to these drugs, making them less effective with time. Moreover, first-generation mast cell stabilizers, such as lodoxamide and cromolyn, potentially take up to several weeks to stabilize the granulating mast cells.
Second-generation mast cell stabilizers, such as Alocril (nedocromil sodium, Allergan) and Alomide (lodoxamide tromethamine, Alcon), have been shown to act much faster and at a lower dosing schedule. A recent study looked at 20 patients taking nedocromil bid for four days. Twelve hours after their last daily dose, researchers exposed those patients to cat dander in a room for one hour. Overall response to the allergen showed that nedocromil has a long duration of action when patients followed the assigned twice-a-day dosing regimen. At the end of one hour, more than 80% of patients had no symptoms of allergy, even while sitting in the cat-dander room.7 This study demonstrates that second-generation mast cell stabilizers may be appropriate for treating mild forms of allergic conjunctivitis.
The combination of a mast cell stabilizer and histamine blocker is the recommended treatment for severe allergic conjunctivitis. Dual therapy medications such as Zaditor and Patanol (olopatadine, Alcon) give immediate relief, with histamine antagonism. Consistent use of these medications can ameliorate future allergic events by preventing mast cell degranulation. For example, studies have demonstrated that olopatadine reduces the pro-inflammatory cytokine secretion of the mast cells by tenfold when compared with antazoline and Naphcon-A (naphazoline hydrochloride/pheniramine maleate, Alcon).8
The current dosage of olopatadine 0.1% is bid. A soon-to-be-released study will report the results of a single dose of olopatadine 0.2% for the treatment of allergic conjunctivitis. Using a double-masked, randomized, placebo-controlled study with 260 allergic patients, the authors conclude that olopatadine 0.2% is a safe, well-tolerated and effective treatment for the ocular symptoms of allergic conjunctivitis when dosed once.9
Inflammation
Prostaglandins (PGE2) are thought to potentiate degranulation of mast cells stimulated with IgE. In fact, one study found more prosta-glandins in tears of patients with ocular allergies than in tears of patients with post-surgical inflammation.10
This research demonstrates that anti-inflammatory medicationsboth steroids and NSAIDS, such as Alrex (loteprednol etabonate, Bausch & Lomb) and Acular (ketorolac tromethamine, Allergan)can be a useful adjunct in treating late-phase allergic response. One study found no statistical difference in response when researchers compared the efficacy of an NSAID with a mild steroid in combination with anti-allergy meds.11
Although the long-term use of steroids may initiate a rise in intraocular pressure, site-specific steroids such as loteprednol have been proven safe and show a decrease in the risks commonly seen with ketone-based steroids when used long-term.12
Research continues to try to find the most appropriate anti-allergy treatment, based on a variety of factors. Although prophylaxis is still the best treatment, be cognizant of the signs and stages of the allergic response of your patients. Ignoring these signs may lead to priming, a condition in which a lower amount of antigens is required to elicit a full-blown allergic response. Our goal should be to provide immediate relief coupled with long-term stabilization of the mast cell complex and an overall suppression of the immune response.
Dr. Bloomenstein frequently lectures on allergy and and practices at Barnet Dulaney Perkins Eye Center, Phoenix, Az.
1. Pflugfelder SC, Solomon A, Stern ME. The diagnosis and management of dry eye: a twenty-five year review. Cornea 2000 Sep;19(5):644-9.
2. Nelson JD, Helms H, Fiscella R, et al. A new look at dry eye disease and its treatment. Adv Ther 2000 Mar-Apr;17(2):84-93.
3. Welch D, Ousler GW 3rd, Nally LA, Abelson MB. Ocular drying associated with oral histamines (loratadine) in the normal population. Cornea 2000 Nov;19(6, Suppl 2): S135.
4. Gomes PJ, Krokhmal L, Abelson MB, Welch DL. Allergic rhinoconjunctivitis is mediated primarily through ocular exposure to allergen. ARVO Abstract #4849: April 29, 2004.
5. Friedlaender MH, Sharf L, Breshears D. Control of ocular allergy symptoms by epinastine HCL 0.005% in a conjunctival antigen challenge evaluation. ARVO Abstract #4841. April 29, 2004.
6. Bonini S, Whitcup SM, Barett J. Efficacy of epinastine HCL 0.05% ophthalmic solution in patients with acute allergic conjunctivitis compared with ketotifen. ARVO Abstract #4842. April 29, 2004.
7. Rothman JS, Raizman MB. Comparison of 2% nedocromil sodium eye drops with Patanol for the treatment of cat dander allergic conjunctivitis. Invest Ophthalmol Vis Sci 2000;41(4):S367(Abstract 1928).
8. Yanni JM, Weimer LK, Sharif NA, et al. Inhibition of histamine-induced human conjunctival epithelial cell responses by ocular allergy drugs. Arch Ophthalmol 1999 May;117(5):643-7.
9. Abelson MB, Gomes PJ, Welch DL, et al. Olopatadine 0.2% is effective for the once daily treatment of the ocular signs and symptoms associated with allergic conjunctivitis. ARVO Abstract #4824. April 29, 2004.
10. Takano Y, Igarashi A, Okada N, et al. PGE2 production from conjunctival and corneal cells in allergic conditions and the measurement of PGE2 concentrations in tears of patients with severe ocular allergies. ARVO Abstract #4826. April 29, 2004.
11. Fujishima H, Tanaka M, Fukagawa K, et al. Comparison of the efficacy of NSAID (bromfenac sodium) and steroid (fluorometholone) eye drops in the treatment of allergic conjunctivitis. ARVO Abstract #4832. April 29,2004.
12. Ilyas H, Slonim CB, Braswell GR, et al. Long-term safety of loteprednol etabonate 0.2% in the treatment of seasonal and perennial allergic conjunctivitis. Eye Contact Lens 2004 Jan;30(1):10-3.
13. Ciprandi G, Buscaglia S, Pesce G, et al. Minimal persistent inflammation is present at mucosal level in patients with asymptomatic rhinitis and mite allergy. J Allergy Clin Immunol 1995 Dec;96(6 Pt 1):971-9.

