 |
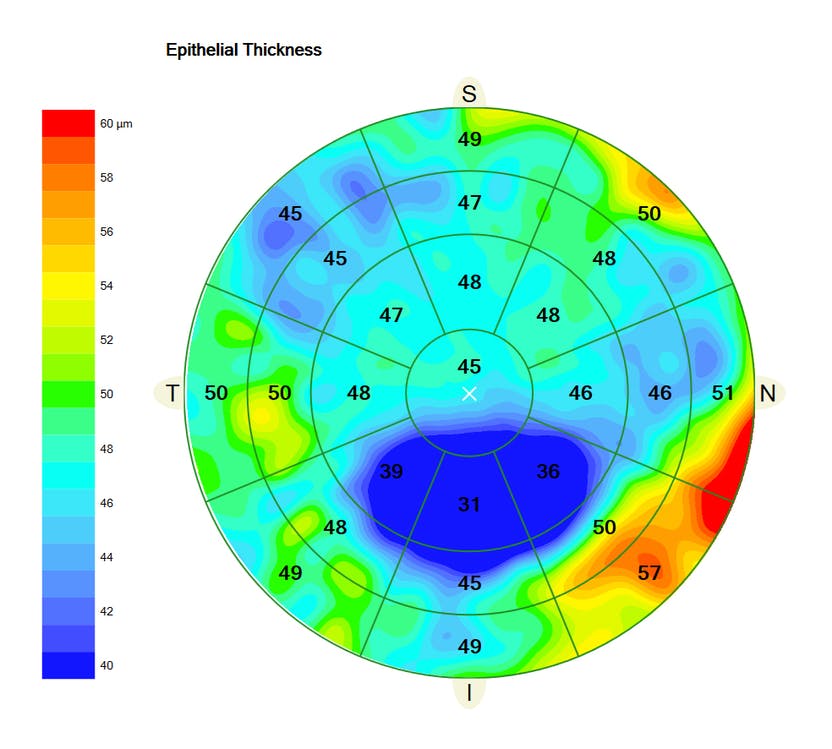
| Researchers found that corneal and epithelial thickness maps are an accurate way to detect and diagnose keratoconus. Photo: Carl Zeiss Meditec. Click image to enlarge. |
It is important to detect keratoconus as early as possible in life to begin efforts aimed at preventing disease progression and to be mindful of ectasia risk if the patient pursues corneal refractive surgery. Even in its early stages, keratoconus can be detected by typical patterns on OCT pachymetric and epithelial thickness maps as focal thinning at the same or contiguous location. A recent study determined the validity of this approach in a larger population by analyzing corneal and epithelial map parameters and patterns with spectral-domain OCT.
The researchers developed a two-step decision tree with a Zeiss Cirrus that was based on previous studies with another OCT device, the Optovue Avanti. In step one, the team measured corneal minimum, minimum-median and superonasal-inferotemporal pachymetry as well as epithelial superonasal-inferotemporal thickness. If at least one of these parameters exceeded the cutoff, the eye was then considered suspicious for keratoconus and subjected to step two. If none of the four parameters overran the cutoff, then the eye was accepted as healthy. Step two required a grader to inspect the corneal and epithelial thickness maps and search for characteristic keratoconic map patterns of coincident and concentric epithelial thinning.
The study included 172 manifest keratoconic eyes (108 patients), 21 subclinical keratoconic eyes (20 patients) and 172 normal eyes (90 age-matched participants). Step one captured 100% of manifest and subclinical keratoconic eyes. Step two ruled out all suspicious but normal cases and, falsely, two subclinical keratoconic eyes. The decision tree reached 100% specificity with 100% sensitivity in manifest keratoconus and 90.4% sensitivity in subclinical keratoconus. Epithelial superonasal-inferotemporal had the best sensitivity in both manifest and subclinical keratoconus (97% and 85.7%, respectively).
“This study showed that pachymetric and epithelial map parameters and patterns of the Zeiss Cirrus OCT can be used in the diagnosis of keratoconus, including subclinical cases,” the study authors concluded in their paper. “At present, using this decision tree with the cutoff values described here together with tomography and other examinations may reduce the margin of error in the diagnosis of keratoconus to a minimum.”
Yücekul B, Dick HB, Taneri S. Systematic detection of keratoconus in optical coherence tomography: corneal and epithelial thickness maps. J Cataract Refract Surg. June 13, 2022. [Epub ahead of print]. |

