Taking the Lead on GlaucomaJuly's issue is our 28th annual glaucoma report, where we explore the latest in treatments, technology, MIGS and diagnostic techniques to manage your patients with this aggressive disease. |
Glaucoma is one of the leading causes of blindness in the United States, affects more than three million Americans and accounts for more than 17 million office visits a year.1 With an aging and increasingly diverse population, optometrists will see more glaucoma in their offices and need to be prepared.
In terms of managing and diagnosing glaucoma, standard automated perimetry (SAP) has been the gold standard for decades. Whether the progressive loss of retinal ganglion cells in our glaucoma patients is from compressive forces, vascular ischemia or a combination of both pathophysiologies, axonal disruption is quantifiable using diagnostic perimetry and optical coherence tomography (OCT).
Newer technologies such as OCT allow measurement of retinal nerve fiber and ganglion cell layer thicknesses, thus visualizing structural changes from glaucoma that may present prior to functional loss, allowing for earlier detection. However, to evaluate functional change, SAP remains standard of care, making it a crucial tool for managing glaucoma.
Standard automated perimetry devices such as the Humphrey Field Analyzer (HFA; Zeiss) and Octopus (Haag-Streit) are cornerstones in most optometric offices. However, the instrument takes up office space, must be isolated to a dark room and is dependent on proper instructions and patient positioning. This makes testing difficult and time consuming for staff and patients. In addition, certain patients may be precluded from visual field testing (i.e., those who have limited mobility or are home-bound).
With recent technological advances, alternatives to SAP have become available. The increased presence of headset technology in eyecare could make it easier for healthcare providers to individualize management.2 These tools can be adapted to a patient instead of requiring the patients to conform to analog instruments.
Visual information analysis with headset-based visual fields is an exciting technology with numerous possibilities for improving optometric care.3
This device’s portability may contribute to increased efficiency in a typical practice; multiple test subjects can be assessed simultaneously using the same server in a single, well compartmentalized room, by a single technician. Doctor-patient interactions may also change from centralized to more individual settings, providing more options for providers to reach marginalized and underserved communities.
Several portable visual field testing options are described below. As independent data is scarce, bear in mind that much of what’s discussed comes from company sources. We also review independent research when possible.
 |
|
This VF headset and remote allows patients to not hunch forward, as in a traditional SAP device. They are free to move their head and neck, sit back in a chair and enjoy being more comfortable. Photos: James L. Fanelli, OD. Click image to enlarge. |
VisuAll (Olleyes)
This device is a portable virtual reality headset with a wireless, Bluetooth-enabled remote to record patient responses. It’s available in three models: VisuAll ETS and VisuAll S for office use and VisuAll H for home use.4
The test can be performed in any position or lighting condition. No trial lenses are needed as patients can wear their own glasses.4 The head-mounted display is split into two halves, one for each eye, eliminating the need for patching. Patient testing instructions are given in an easy-to-follow video.
Gaze tracking and fixation monitoring are built into the application. The patient will be prompted to return to central fixation and stimuli presentations are stopped until fixation is corrected.
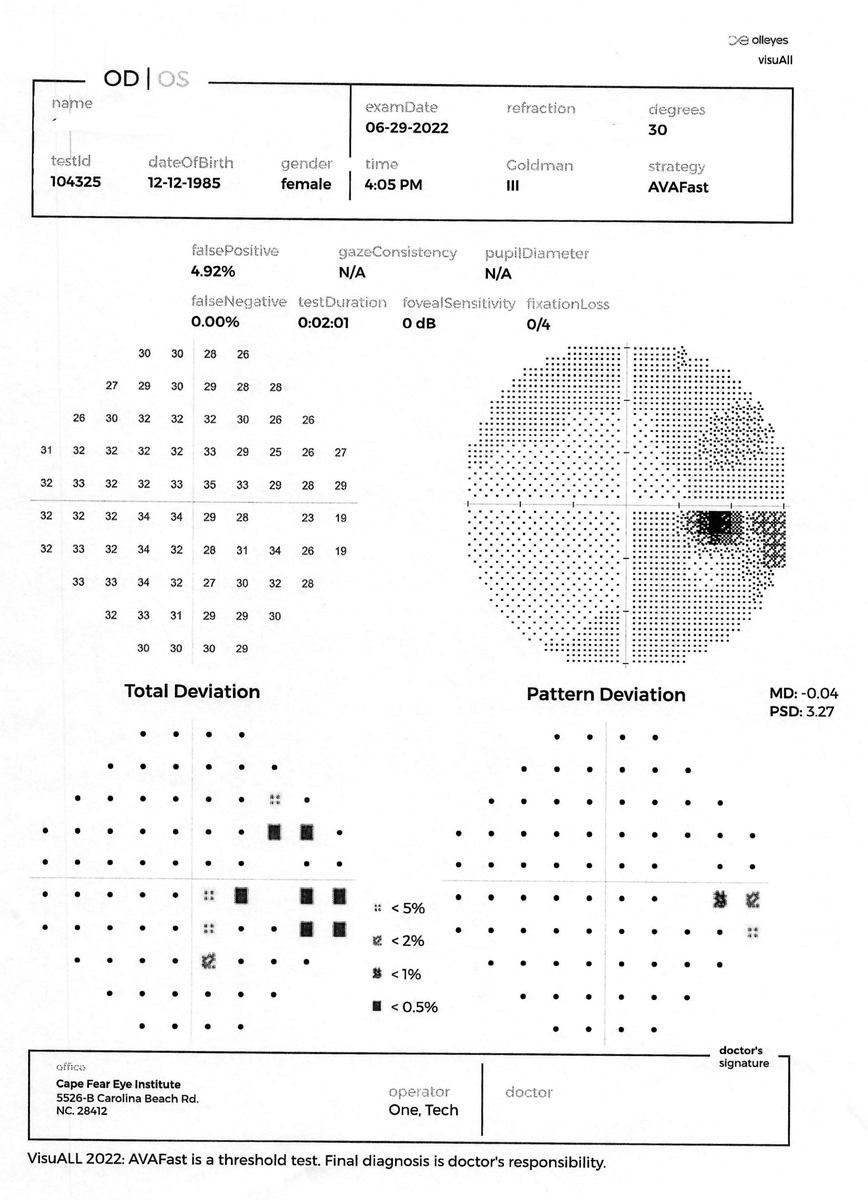
Results from the VisuAll are displayed through an application that can be downloaded onto a laptop, smartphone or tablet for the doctor’s interpretation. The test result layout is similar to the HFA, making interpretation familiar and straightforward.5
In addition to visual field testing, VisuAll offers color vision testing, visual acuity testing, contrast sensitivity, extraocular motility and pupillometry. The company says that visual field testing options range from the most common protocols (24-2, 30-2, 10-2) to screening tests. Testing time is about three minutes for threshold and 45 seconds for screenings.4
When comparing the 24-2 option of the VisuAll with our standard perimeters (i.e., Humphrey and Octopus), there are a lot of similarities. The background luminance of the VisuAll is 10cd/m2, which is the same as both the Humphrey and Octopus. White-on-white stimuli are presented at a duration of 200ms. This matches with the Humphrey but varies from the Octopus at 100ms.
The VisuAll presents 50 test locations, which is slightly less than the Humphrey at 54 and the Octopus at 59. Stimuli are presented in a 6º grid pattern across the horizontal and vertical midlines.2 This is identical to the Humphrey but varies from the Octopus, which presents stimuli in an unequal spacing pattern, more dense centrally and more spaced out peripherally.
Research review. As it stands, information from clinical trials regarding the VisuAll’s performance is positive in regards to its performance compared with traditional SAP. In a limited study out of the Wills Eye Institute, 25 healthy eyes vs. 26 controlled mild/moderate glaucoma eyes were evaluated with a 24-2 test with both the VisuAll and HFA. Testing time for the VisuAll was on average three minutes longer for both healthy and glaucomatous eyes than the HFA. VisuAll runs a full threshold, which takes more time than a SITA standard. The mean sensitivity of the whole visual field and the sensitivity of each individual quadrant in the two devices were compared with excellent correlation.5,6
Moreover, another study, done at Glaucoma Associates of Texas, was presented at the American Glaucoma Society (AGS) meeting in March 2022.7 It looked at early detection of retinal dysfunction in eyes with pre-perimetric glaucoma using a virtual reality platform. Over 1,700 patients were tested with the VisuAll; 128 were diagnosed with pre-perimetric open-angle glaucoma. The VisuAll was then compared with the HFA and with the corresponding ganglion cell complex areas on OCT to evaluate structure-function relationship of both instruments. Results showed that the VisuAll and HFA were similar in detecting decreased retinal sensitivity of the superior hemifield that correlated to the corresponding inferior ganglion cell complex thickness.7 Overall, VisuAll detected a greater number of visual field defects than the HFA in eyes with pre-perimetric glaucoma.7
re:Vive (Heru)
Heru is a company founded by physicians and researchers at Bascom Palmer Eye Institute. Two versions of this device currently exist: re:Vive 1.0 and the updated 2.0. The unit consists of a lightweight headset and wireless clicker to record patient responses. A software application can be downloaded onto a portable device such as a laptop or tablet for result viewing.8
The re:Vive continually tells the patient how to take the test through a function called Virtual Personality to educate the patient on test-taking instructions. It also has another function called Active Track that corrects for fixation and gaze tracking errors using cameras in the device. A stimulus is only presented if the patient is properly fixating. In addition, if a screening test is being run and the patient is struggling, the re:Vive will automatically convert the test into a full threshold.
No trial lenses are needed. The re:Vive presents the stimuli at optical infinity, thus presbyopic changes are of no consequence.
Current available visual field tests include: 24-2, 10-2, suprathreshold and foveal threshold. Stimuli are bright on a dark background with a luminance of 10cd/m2. The testing results layout is similar to the HFA, again making interpretation straightforward.
The re:Vive 2.0 model added additional modes, including color vision testing (screener Ishihara plates, extended Farnsworth D-15) and contrast sensitivity testing. Clinical trials testing this model are still in progess.
Research review. When compared with the HFA, threshold testing time for the re:Vive is 4.3 minutes as opposed to five minutes. One study noted its repeatability and that mean deviation has a strong correlation.9
To further confirm the accuracy of the Heru Threshold test strategy, a prospective study comparing the HFA 24-2 with re:Vive by Heru 24-2 was performed. The study included 47 eyes (21 healthy and 26 patients with glaucoma and neuro-ophthalmic diseases) and found strong correlations between the Heru visual field mean deviation (MD) and threshold values and those of HFA in normal eyes and eyes with glaucoma and other pathologies.10 That study also found excellent reproducibility on normal and pathologic eyes, respectively. The device’s re:Imagine Threshold strategy was statistically significantly faster than the HFA SITA Standard (4.3 vs. five minutes respectively).9,10
 |
|
The printout from the VisuAll unit is laid out exactly the same as an HFA printout to ease the transition to the new platform. Photo: James L. Fanelli, OD. Click image to enlarge. |
VF2000 (Micro Medical Devices)
This company launched the first virtual reality visual field headset in 2018—the VF2000 Visual Field Analyzer. MMD now offers three versions: VF2000 Focus, VF2000 G2 and VF2000 NEO. All units are composed of a lightweight headset and wireless patient response remote.11
The VF2000 Focus is equipped with a technology the company calls Focus Wheel that accounts for up to seven diopters of refractive error, reducing the need for trial lenses for a significant amount of patients.12
The VF2000 G2 adds 4K resolution and optional vision screening tests. Finally, the VF2000 NEO model offers the previously mentioned features plus eye tracking technology to reduce fixation errors.13,14
Interestingly, the Active Eye Tracking technology in the Neo model pauses the test if patients shut their eyes allowing for a break. Also, there is an option to use a patient’s blink to measure stimuli response. This is an advantage over other devices that may allow patients with disabilities or paralysis to complete visual field testing.14
Similar to other devices, the VF2000 series offers other functionalities, such as visual acuity testing, color vision testing and contrast sensitivity testing.11
Research review. A study out of Stanford University compared the VF2000 to the HFA. A total of 41 patients with known history of reliable visual field testing were selected, 28 of whom were known to have glaucoma and 13 were glaucoma suspects. MD and pattern standard deviation (PSD) were compared between both devices. Results found less than a 0.20dB difference between the VF2000 and HFA across all patients.15
Another study determined that the Palm Scan VF2000 was 100% sensitive and specific in detecting glaucoma. However, about 28% of moderate glaucoma cases were misclassified as mild and 17% were misclassified as severe by the visual field analyzer. Furthermore, 20% of severe cases were misclassified as moderate by this instrument.16
Advanced Vision Analyzer (AVA; Elisar Vision Technologies)
This organization, based in India, has presented a device that consists of a battery operated head-mounted device with a cable-attached patient response button. The results of the test can be displayed on a laptop or tablet.17
The AVA offers foveal threshold testing, 24-2, 30-2 as well as screening tests. A fixation monitoring, eye-tracking system is included. A cloud-based software allows doctors to wirelessly print or email reports.17
Research review. Little independent information is known about this device. One study demonstrated functional equivalence between the AVA and the HFA. However, its authors noted that further studies with larger numbers of patients and detailed clinical evaluation for the actual diagnostic accuracy of the AVA were required to allow for definite conclusions.18
Melbourne Rapid Fields (MRF; M&S Technologies)
M&S recently launched a virtual reality headset with similar features as the previously mentioned devices. But in addition to the VR headset, M&S offers two versions of their MRF that can be clinic-based or home-based.19 These options allow for more frequent progression analyses as well as patient convenience.
The clinic-based MRF is a portable, space saving design consisting of a tablet with responder and surround shroud. The shroud blocks reflections, ambient lighting and maintains 33cm distance.20
Tests offered include: 10-2, 24-2, 30-2 and screening. Testing time is three to four minutes per eye for a threshold 30-2. Patient instructions are given through an interactive system throughout the test. Upon completion, the results can be saved to a HIPAA-compliant cloud-based storage, saved as a PDF, printed or integrated into an EMR.
In a 2016 study, 90 eyes were tested using the MRF vs. SITA standard 24-2 HFA. Each test was run twice to establish repeatability. In the cohort, 12 eyes were healthy and 78 were glaucomatous ranging from mild to moderate stage. Results showed shorter test durations on the MRF vs. HFA (5.7 minutes vs 6.3). The MRF had a high correlation with HFA on MD and PSD. In addition, repeatability of MRF highly corresponded to the HFA. The overall conclusion was that there was a strong correlation between outcomes and repeatability between the two devices.21
With the web-based Melbourne Rapid Fields, the software application is emailed through a secure link. The patient opens the link from the comfort of their home on a computer or tablet to complete a visual field test. The patient follows the prompts given to fixate appropriately on the stimuli presented. The results are immediately transmitted to the doctor.22
In 2021, M&S Technologies announced its new device, the Smart System Virtuality Reality Headset. It will provide accurate 10-2, 24-2 and 30-2 visual field and contour stereo testing. The headset is purported to be adaptable to add many of the Smart System vision testing modules.23
Incorporating VR Visual Fields into a Busy OfficeBy James L. Fanelli, OD We are now a bit over six months into using virtual reality (VR) field testing in our office using the VisuAll Olleyes VR field unit. To say this has been a game changer is an understatement. My practice is heavily glaucoma- and neuro-ophthalmology-based, which in turn generates a very significant number of VF tests each day. Prior to the addition of the Olleyes unit, we were running two separate VF instruments, and those machines were kept pretty busy each day. With the addition of this VR field unit, several metrics have changed, for the better. From a logistics perspective, the VisuAll is mobile, portable and small. It can be used anywhere in your office and does not require a dedicated VF room. More often than not, the patient undergoes testing in the dilation/hold area in the patient care section of the office. It does not need to be completed in a pretest or exam room. That is very different from traditional field testing space requirements. From a patient experience perspective, the effect of adopting this technology has been huge, especially in the glaucoma population. These patients are used to having periodic VF tests, and I’d say that very few of them actually look forward to taking the test. While I’ve known for years many patients’ reticence to taking VFs, I always imagined it was because they thought the test was boring or simply difficult to take. To my surprise, the number of patients who’ve completed the Olleyes testing who have expressed subdued happiness has been huge. Every day, unsolicited positive responses come from patients having completed the testing. But what I found most interesting is the common theme of patient comfort; they don’t need to hunch forward and remain stationary in a traditional field device. The are free to move their head and neck, sit back in a comfortable chair and enjoy not being immobile. It makes perfect sense, and I didn’t realize that was the biggest hurdle my patients had with traditional field units. Testing time is also greatly reduced, as full threshold field testing is done binocularly using a novel method, further facilitating patient acceptance. From a reliability perspective, having a large number of patients in clinic with chronic disease processes and serial fields over many years, of utmost concern to me was the reliability and reproducibility of test results. Of course, when one moves from one VF platform to another, data conversion may not exist. Establishing a new baseline is rather easy with the VisuAll unit; after the field tests, baseline data can be generated. Certainly, the first one or two fields need to be manually compared with the previous field device you were using, but with greater patient acceptance of this technology, getting to that threshold of three tests is relatively painless. Fortunately, I’ve been very pleased with the reproducibility of field defects seen in both patients with advanced and mild disease, when comparing older technology to the newer tools. While the field printouts look similar to a standard HFA field printout, the devil is in the details. And conveniently, the raw data (e.g., decibel values, pattern deviation) match up pretty well, and this has been validated clinically.1 From a billing perspective, the VR technology carries the same criteria, and CPT coding as does standard field testing, depending on the strategy used (screening or threshold field studies). Furthermore, available tests include 30-2, 24-2, 10-2, neuro fields and ptosis fields. Those account for all of the strategies used in my clinic. CPT coding is the same as standard field testing, and reimbursement is the same. The learning curve for my techs to operate the instrument was very short, and the device has verbal instructions in several languages for patients, making patient learning time very short. Conveniently, the instrument also performs other tests, such as visual acuities, pupillometry and color vision, lending itself to a pretesting suite of tests that can be performed in the office before the physician sees the patient. In fact, we just acquired a second unit to begin using it in this regard; the tech sets the patient up with the headset and leaves to begin evaluating a second patient while the first undergoes the series of programmed tests, reducing one-on-one tech/patient time. I no longer feel that I am beating up patients every time I need another field to follow their glaucoma or neuro-ophthalmology problem. I don’t experience their sighs or exasperation with the thought of a subsequent test. They actually enjoy the new format, believe it or not. Just as important, I get reliable data I can use to effectively manage the patient precisely. Disclosure: Dr. Fanelli has consulted with VisuAll on this visual field unit. 1. Razeghinejad R, Gonzalez-Garcia A, Myers JS, Katz LJ. Preliminary report on a novel virtual reality perimeter compared with standard automated perimetry. J Glaucoma. 2021;30(1):17-23.5. |
On the Horizon
The objectiveField Analyzer (OFA) by Konan Medical is not currently commercially available. The company details that the device works by analyzing pupillary responses to multifocal stimuli using infrared cameras. Responses are measured using something the company calls “clustered volley,” a multifocal pupil objective perimetry method.24
Multifocal stimuli are arranged in a dartboard layout consisting of 44 test regions per eye. The OFA presents dichoptic multifocal stimuli to both eyes, measuring direct and consensual responses from each eye concurrently. The company asserts that the patient will find this comfortable and appreciate having the test completed quickly and without need for user input.25
The initial technical specifications state that a macular, 24º and 30º test are available. A 30º test that is equivalent to a 30-2 takes seven minutes to test each eye concurrently. Trial lenses are needed: -3.00D, +3.00D, -6.00D, +6.00D, -9.00D, +9.00D. Background luminance is 10cd/m2.
The objectiveField Analyzer is not a portable device. Thus, it retains the attendant disadvantages of traditional perimeters in that aspect. However, its clinical applications extend beyond perimetric evaluation.
Researchers in Australia have tested prototypes of this device. One study determined its ability to diagnose and monitor multiple sclerosis in early-stage disease.26 Another study determined that the OFA might be a useful tool for assessing retinal function, detecting altered sensitivity and delay even before detectable structural changes. Peripheral macular regional thickness was more correlated with the device’s sensitivity and delay than the central macula. Thus, peripheral macular health may have higher prognostic value than central retinal.27
Discussion
Virtual reality visual field devices offer much promise and some genuinely new ideas. The advantages over SAP are tremendous. These portable devices can be used anywhere in the office without staff supervision, freeing up office space and reducing staffing challenges. Moreover, the application’s simplicity may increase clinical efficiency, allowing practices to administer more field tests per patient, thus improving accuracy over time. The removal of patching and trial lenses make test administration much easier for the patient, and built-in gaze tracking and fixation monitoring enables better reliability.
In addition, these mobile technologies have the potential to help provide higher quality eye care to limited mobility patients, nursing home and homebound patients, medical missions and community-based healthcare centers.
As with any new technology, more clinical trials and studies are needed, particularly with larger sample sizes. The early data that is available now shows strong correlation and repeatability with standard automated perimeters. More compelling, however, would be independent studies that document the capabilities of these devices in detecting disease progression—something sorely lacking in the current literature.
Besides limited data, another potential disadvantage of the portable devices is lack of stimulus presentation options. For reduced visual acuity and moderate/severe glaucoma patients, a stimulus V is needed for better accuracy in following glaucoma progression. Stimulus III presentation is the most common option on most of the portable devices.
In addition, all the portable devices offer numerous other testing capabilities such as contrast sensitivity, color vision and visual acuities. Is it worth having an all-in-one device, but not have its merit verified for a long time? If all pre-existing office equipment were replaced with headset-based testers, what would happen if the device malfunctioned? Of course these are hypotheticals, but something to ponder.
Portable headsets have the potential to upgrade and improve a tedious aspect of eye care. However, at this time, I feel not enough independent data is available to comfortably start debulking our clinics of our standard perimeters.
This exciting technology has the ability to offer more advantages than disadvantages over traditional standard automated perimeters. As more research data emerges, our options for treating and managing glaucoma will continue to grow.
Dr. Anspaugh practices medical optometry at Eye Physicians and Surgeons of Arizona, an ophthalmology clinic specializing in glaucoma and cataracts. She is a Fellow of the American Academy of Optometry. She has no financial disclosures.
1. Centers for Disease Control and Prevention. Don’t let glaucoma steal your sight! Vision Health Institute. November 24, 2020. www.cdc.gov/visionhealth/resources/features/glaucoma-awareness.html. Accessed June 1, 2022. 2. Montelongo M, Gonzalez A, Morgenstern F, Donahue SP, Groth SL. A Virtual Reality-Based Automated Perimeter, Device, and Pilot Study. Transl Vis Sci Technol. 2021;10(3):20. 3. Soans RS, Renken RJ, John J, et al. Patients Prefer a virtual reality approach over a similarly performing screen-based approach for continuous oculomotor-based screening of glaucomatous and neuro-ophthalmological visual field defects. Front Neurosci. 2021;15:745355. 4. Olleyes. Olleyes virtual visual field products. olleyes.com. Accessed June 1, 2022. 5. Razeghinejad R, Shukla AG. In the field. The Ophthalmologist. August 25, 2020. theophthalmologist.com/subspecialties/in-the-field. Accessed June 1, 2022. 6. Razeghinejad R, Gonzalez-Garcia A, Myers JS, Katz LJ. Preliminary report on a novel virtual reality perimeter compared with standard automated perimetry. J Glaucoma. 2021;30(1):17-23. 7. Grover DS, Tolman A, Ali A, Fellman RL. Early detection of retinal dysfunction in eyes with pre-perimetric glaucoma using a virtual reality platform. Poster presented at American Glaucoma Society Annual Meeting. March 2022. olleyes.com/wp-content/uploads/2022/03/AGS-2022-GAT-poster.pdf. Accessed June 1, 2022. 8. Heru. Rethinking glaucoma management using wearable diagnostics from Heru reVive visual field. www.seeheru.com/rethinking-glaucoma-management-using-wearablediagnostics- from-heru-revive-visual-field. Accessed June 1, 2022. 9. Goldbach AH, Shousha MA, Duque C, et al. Visual field measurements using Heru Visual Field Multi-platform application downloaded on two different commercially available augmented reality device. ARVO Annual Meeting 2021. 10. Kashem R, Godlbach AH, Elsawy A, et al. Comparison of Heru Visual field as a cloud based artificial intelligence-powered software application downloadable on commercial augmented reality headset with Humphrey Field Analyzer SITA Standard. ARVO Annual Meeting 2021. 11. Micro Medical Devices. A virtual reality visual field headset for the modern practice. micromedinc.com/vr-visual-field-test-headset. Accessed June 1, 2022. 12. Micro Medical Devices. Visual field analyzer —VF2000 Focus. micromedinc.com/vf2000-visual-field-analyzer. Accessed June 1, 2022. 13. Micro Medical Devices. The next evolution of the visual test machine—G2. micromedinc.com/VF2000-g2. Accessed June 1, 2022. 14. Micro Medical Devices. The premium virtual reality visual field device—Neo. micromedinc.com/VF2000-neo. Accessed June 1, 2022. 15. Tran E, Wan L, Yan W, et al. Comparison of virtual reality (PalmScan VF2000) visual fields analyzer with Humphrey visual field in glaucoma patients. Invest Ophthalmol Vis Sci. 2020;61:3893. 16. Shetty V, Sankhe P, Haldipurkar SS, et al. Diagnostic performance of the PalmScan VF2000 Virtual Reality Visual Field Analyzer for identification and classification of glaucoma. J Ophthalmic Vis Res. 2022;17(1):33-41. 17. Elisar Vision Technology. AVA Advanced Vision Analyzer. www.elisar.com/products. Accessed June 1, 2022. 18. Narang P, Agarwal A, Srinivasan M, Agarwal A. Advanced Vision Analyzer–virtual reality perimeter: device validation, functional correlation and comparison with Humphrey Field Analyzer. Ophthalmol Sci. 2021;1(2):100035. 19. M&S Technologies. Melbourne Rapid Fields (MRF). www.mstech-eyes.com/products/category/melbourne-rapid-fields. Accessed June 1, 2022. 20. M&S Technologies. In-clinic visual field testing. www.mstech-eyes.com/products/detail/melbourne-rapid-fields. Accessed June 1, 2022. 21. Kong YX, He M, Crowston JG, Vingrys AJ. A comparison of perimetric results from a tablet perimeter and Humphrey Field Analyzer in glaucoma patients. Transl Vis Sci Technol. 2016;5(6):2. 22. M&S Technologies. Web-based visual field testing. www.mstech-eyes.com/products/detail/mrf-web-based. Accessed June 1, 2022. 23. M&S Technologies. M&S Technologies launches the Smart System virtual reality headset including Critical Eye Tracking. www.mstech-eyes.com/news/story/ms-technologies-launches-the-smart-system-virtual-reality-headset-including. August 2, 2021. Accessed June 6, 2022. 24. Konan Medical. ObjectiveField frequently asked questions & specifications. www.konanmedical.com/ofa-specs-faq. Accessed June 6, 2022. 25. Konan Medical. ObjectiveField objective field analyzer (OFA). www.konanmedical.com/objectivefield. Accessed June 6, 2022. 26. Carle C, Maddess T, Baird-Gunning J, et al. Diagnostic power of rapid objective visual testing of multiple sclerosis patients. Invest. Ophthalmol Vis Sci. 2021;62(8):2420. 27. Rai BB, Maddess T, Carle CF, et al. Comparing Objective perimetry, matrix perimetry and regional retinal thickness in mild diabetic macular edema. Transl Vis Sci Technol. 2021;10(13):32. |

