 |
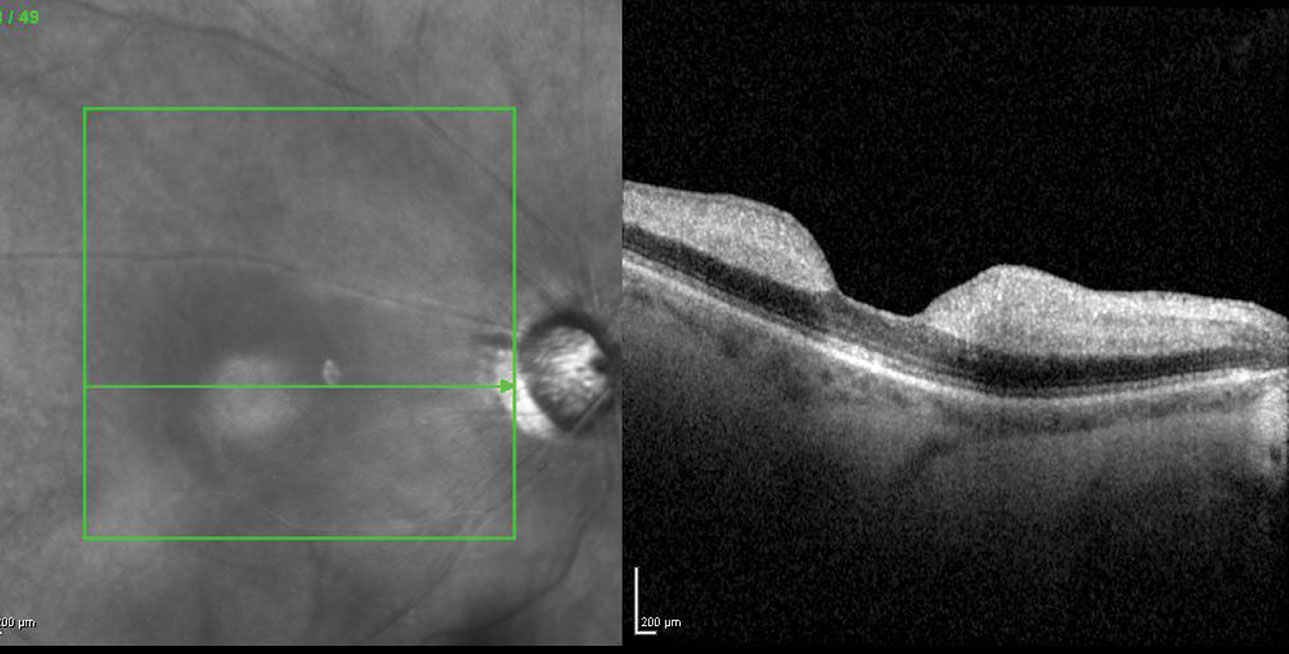
| CRAO is one condition that ODs can help in proper referral of to alleviate the burden of ophthalmologists and neuro-ophthalmologists, ultimately resulting in better patient outcomes. Photo: Diana Shechtman, OD. Click image to enlarge. |
Consistent with projections of an overall decline in the ophthalmology workforce, estimates at the level of individual subspecialties reveal insights into that profession’s current readiness (or lack thereof) to meet demand. A new study on neuro-ophthalmology in the US paints a dispiriting picture.
Previous research has indicated the need for neuro-ophthalmologists in the US to be approximately one such expert per 1.2 million individuals. A recent survey has estimated the current ratio level to be about 1.7 million individuals per neuro-ophthalmologist; only eight states reported numbers below the estimated threshold of 1.2 million.
In one new study in Ophthalmology, the current demographic characteristics and geographic distribution of neuro-ophthalmologists was recorded as of April 2023. According to this new research, their mean was about 1.9 neuro-ophthalmologists per million people in the US, but the range varied based on geographic location.1
Of the total 635 neuro-ophthalmologists identified, 68.7% were male and a strong majority (94.3%) graduated from an allopathic medical school; of the 85 physicians with a secondary graduate degree, 63.5% had a PhD. Interestingly, 25% of all neuro-ophthalmologists did a residency in neurology and 7.4% did a residency in ophthalmology and neurology, compared with the three-quarters that completed an ophthalmology residency. Almost one-third (30%) were trained in more than one fellowship, most commonly oculoplastics (12.3%) and pediatric (8.3%) ophthalmology.
Alarmingly, most of the current workforce is estimated to be in their late careers, with 60% in practice for 20 years or more. Comparatively low percentages were made up of mid-career neuro-ophthalmologists (18.9%, 10 to 19 years) and early career ones (21.1%, <10 years). Just as alarming, three states (Maine, South Dakota and Wyoming) had no neuro-ophthalmologists. Counties without a neuro-ophthalmologist displayed a lower median income, less vehicle access and lower health insurance rates.
Based on these rates, a projected 180 additional practicing neuro-ophthalmologists are needed to meet US population demand of care. This is especially limited by geography, as most currently practicing were located in metropolitan coastal areas and around academic institutions; Of the top 30 counties with the greatest neuro-ophthalmologist numbers, 14 were not accounted for in the top 30 populous counties.
The low number of neuro-ophthalmologists, especially in more remote areas, also reflects recent research that determined mean time from referral to consultation to be 34 days, peaking at one week for urgent care and 13 for routine. Without urgent access, this pushes patients to seek put emergency department (ED) visits, where expertise may be limited and unnecessary tests may take place.
Although the number of ophthalmology residents who are seeking subspecialty training has been increasing, this is not the case for neuro-ophthalmology, and the almost one-third seen in this study to train in an additional fellowship may further exacerbate the shortage, as some did not list neuro-ophthalmology as their subspecialty on institutional home pages. However, an increase was observed in neurology-trained clinicians among early-career neuro-ophthalmologists, potentially alleviating some of the burden.
The authors of this study propose an immediate call-to-action to boost interest in neuro-ophthalmology as a subspecialty: “Potential strategies to incentivize residents to pursue neuro-ophthalmology could include modifying ophthalmology fellowships to offer extensive training in strabismus, orbital and cataract surgery, as well as temporal biopsy or Botox injection that could help generate more revenue,” they wrote in their paper. “Another strategy to target this problem is to have the neuro-ophthalmology clinical rotation as a required area for neurology residents, especially early in their training. This can boost the number of neurology-trained neuro-ophthalmologists and help alleviate the shortage in this subspecialty.”1
Optometric Role in CRAO
Another recent study, this one in Journal of Neuro-Ophthalmology, highlights just how optometrists can play an increasingly pivotal role in eye care in the wake of a dwindling neuro-ophthalmologist population. The study researchers surveyed the US optometric community to determine current practice patterns in managing central retinal artery occlusion (CRAO), since they are often the first providers to evaluate patients with acute vision loss and diagnose a CRAO.
A total of 1,926 optometrists responded to the survey, of which 98% had diagnosed less than five CRAOs in the prior year and 52% had not diagnosed a CRAO in the prior year. Of those who did diagnose at least one occurrence in the prior year, 71.7% evaluated patients more than four hours after initial vision loss, while only 13.6% evaluated patients within four hours. Those who diagnosed a CRAO primarily referred patients to an ED affiliated with a certified stroke center (44%), outpatient ophthalmology clinics (39.9%), an ED without a stroke center (13%), outpatient neurology clinics (1%) or other, mostly primary care physicians (56.4%).
The 56% of optometrists who responded that did not specify they would refer an acute CRAO patient to an ED with a stroke center emphasizes the need for education in the optometric community. The 40% who would refer them to outpatient ophthalmology clinics sheds light onto the already burdened specialty, especially the subspecialty of neuro-ophthalmology. This is demonstrated by the authors highlighting in their paper that, “given the need to perform an urgent stroke evaluation in acute CRAO patients and the narrow thrombolysis treatment window, it is imperative that optometrists and ophthalmologists are educated to view acute retinal arterial ischemia as a stroke equivalent and establish appropriate networks to immediately refer patients with an acute CRAO to an ED affiliated with a stroke center, instead of referring these patients to outpatient clinics.”2
The authors do suggest some solutions: “Education of optometrists on this topic should be pursued through established and new forums such as continued medical education courses, editorials and stroke awareness campaign advertisements in optometric journals and peer-to-peer education by academic optometric leaders to ‘follow the guidelines.’”2 But for neuro-ophthalmologists, who are greatly overburdened by the current US population, ODs will need to step up and properly manage these patients, referring them to the right type of care. To do so, perhaps optometrists would benefit from neuro-ophthalmologist educational outreach, describing proper protocol for certain conditions seen.
1. Pakravan P, Lai J, Cavuoto KM. Demographics, practice analysis and geographic distribution of neuro-opththalmologists in the US in 2023. Ophthalmology. September 20, 2023. [Epub ahead of print]. 2. Mileski KM, Biousse V, Newman NJ, et al. Optometric practice patterns for acute central and branch retinal artery occlusion. J Neuro-Ophthalmol. September 21, 2023. [Epub ahead of print]. |

