 |
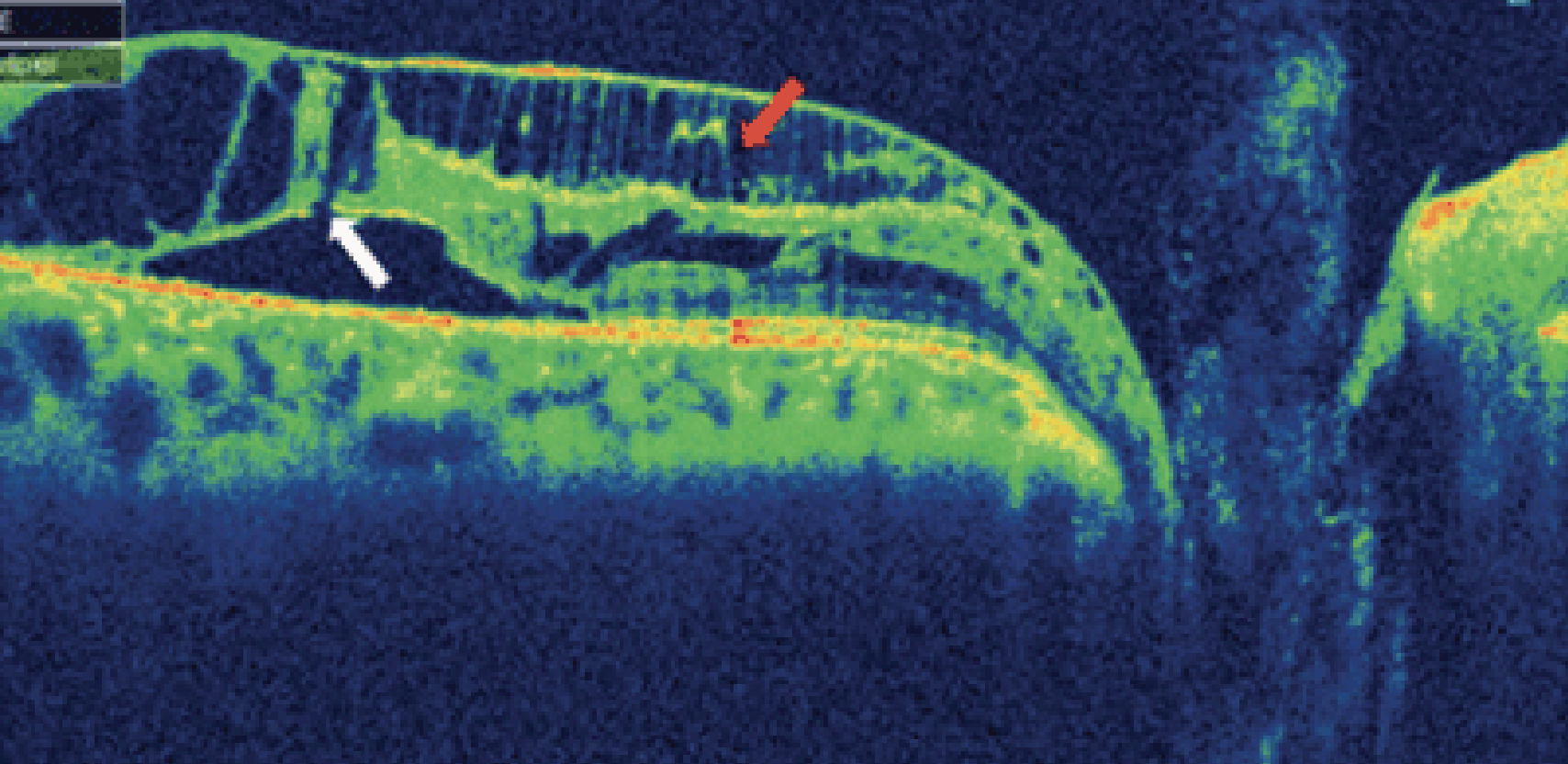
| Multiple retinal splits can be seen in this patient with an optic pit is typical of a macula retinoschisis. Photo: Jerome Sherman. Click image to enlarge. |
Recent research confirmed that peripapillary and macular retinoschisis can develop in eyes without a visible optic pit or advanced glaucomatous cupping. As far as treatment goes, the investigators noted that eyes without foveal involvement and those with foveal involvement but only a mild decrease in vision can be observed for spontaneous resolution. If there is persistent foveal involvement with vision loss, surgery can improve vision by resolving the macular retinoschisis. Surgery for fovea-involved macular retinoschisis without a visible optic pit resulted in faster anatomic resolution and better vision recovery, the team found.
This retrospective, multi-center case series included 11 eyes of 11 patients with macular retinoschisis without a visible optic pit, advanced optic nerve head cupping or macular leakage on fluorescein angiography. Visual acuity (VA), retinoschisis resolution, months to resolution and recurrence of retinoschisis were evaluated in the cohort.
Seven subjects were treated for glaucoma, and nine had nerve fiber layer defects on OCT. All eyes had retinoschisis in the outer nuclear layer in the nasal macula extending to the edge of the optic disc, and eight had fovea-involved retinoschisis. Three non-foveal and four fovea-involved eyes were observed, and four fovea-involved eyes with vision loss had surgery. Surgery involved preoperative juxtapapillary laser followed by vitrectomy, membrane and internal limiting membrane peeling with intraocular gas and face down positioning.
The mean baseline VA was significantly worse in the surgery group than the observation group. Retinoschisis resolved, and vision improved in all surgical cases. The mean resolution time for the surgery group was 2.75±0.96 months, which was shorter than the observation group (28.0±21.2 months). No eye developed recurrence of the retinoschisis after surgery.
“These findings are important as the fluorescein angiogram does not show subretinal or retinal leakage, indicating that the fluid does not arise from the retinal vasculature or subretinal sources in the macula,” the researchers concluded in their paper. “This finding emphasizes that macular edema can occur from the disc even in eyes without a visible optic pit or advanced cupping. If this entity is not recognized, unnecessary procedures including anti-VEGF injections and photodynamic therapy may be performed.”
Fujimoto S, Kokame GT, Ryan EH, et al. Macular retinoschisis from optic disc without a visible optic pit or advanced glaucomatous cupping (no optic pit retinoschisis [NOPIR]). Ophthalmology. June 5, 2023. [Epub ahead of print]. |

