 |
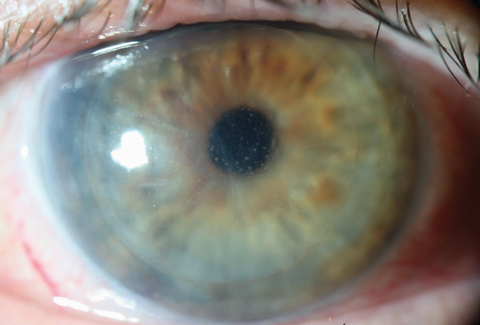
| Corneal transplant patients who receive the COVID-19 mRNA vaccination may be more subject to rejection. Photo: Christopher Kuc, OD. Click image to enlarge. |
Four cases of corneal transplant rejection were reported following COVID-19 mRNA vaccination (Table 1). Researchers suggested general inflammation following rapid antibody development in response to the vaccine may be a possible mechanism.
The authors noted in their recent paper that reports documenting corneal transplant rejection after vaccination are few and limited to small case series. They cited a 2006 report of three corneal transplant rejection cases following influenza vaccination, a single report of bilateral corneal transplant rejection after influenza vaccination a few years prior and a 1998 report of corneal transplant rejection cases associated with hepatitis B, tetanus booster and influenza vaccinations. “A limited understanding of the potential immunologic link between vaccination and corneal graft rejection has rendered true causation difficult to ascertain,” they explained.
All four cases (two men, two women; three white, one African American; age range 61 to 77) had clinically evident immune rejection of their corneal transplants one to two weeks after COVID-19 vaccination. All patients received the mRNA-1273 Moderna vaccine. “Importantly,” the authors wrote, “all had undergone respective keratoplasties dating from at least six months to several years previously, and all had regained corneal graft clarity without previous rejection events. No patient had known infection or exposure to COVID-19.”
“In particular, case one represents a patient who would predictably be at low risk for allograft rejection: a first-graft DMEK recipient who was maintained on daily topical steroids,” they noted. “Although two cases of keratoplasty rejection have been reported in conjunction with COVID-19 infection previously, to the best of our knowledge, these cases represent the initial observations of corneal transplant rejection immediately after COVID-19 vaccination.” All patients received frequent topical corticosteroids in response to rejection.
The authors proposed that vaccination-induced rejection may result from “the disruption in the immunoregulatory state of the eye that normally covers immune privilege.” They said that a nonspecific proinflammatory state post-injection may boost the body’s immune response to foreign, implanted corneal tissue. “Animal and human studies show that both of these mRNA vaccines induce CD4 type-1 helper T-cell activation involved in humoral immunity,” they explained. “Early research demonstrates that low titers of SARS-CoV-2 Immunoglobulin G antibodies can be detected within nine to 12 days after the first vaccine dose in seronegative individuals. Those individuals with existing antibodies from a previous COVID-19 infection can rapidly develop 10 to 20 times the antibody level after a single vaccine dose compared with SARS-CoV-2 naïve individuals.”
In the four cases, individuals experienced ocular symptom onset seven to 17 days following the inciting vaccine dose. Though the patients all denied previous exposure to the virus, they may have had asymptomatic exposure, promoting an inflammatory state. “[It] should also be considered that graft rejection might represent a specific immune reaction of COVID-19 antibodies to SARS-CoV-2 antigens harbored in the cornea,” the researchers wrote. They noted that “asymptomatic viral infiltration through the corneal stroma to reach the endothelium seems unlikely,” however.
“One recent case report of corneal endothelial graft rejection in a patient positive for COVID-19 furthers the idea that transmission of virus across the blood-ocular barrier into the aqueous humor could expose the posterior cornea to SARS-CoV-2,” they continued. “Finally, other local factors and their possible contribution to graft rejection must be considered. For example, in case one, the presence of CME preceding vaccination might indicate increased permeability of the uveal tract, thereby increasing vulnerability to an immune response through uveal antigen-presenting cells.”
They concluded that while there’s no consensus yet among corneal transplant surgeons on treatment, a recent survey suggests a course of action may be to initiate or increase topical steroids in the peri-vaccination period for post-keratoplasty patients receiving any type of vaccine. “As steroid responsiveness with clinical improvement occurred in all of our patients, we recommend such prophylactic initiatives at least until the true assessment of the risk and mechanism of rejection can be ascertained,” they wrote. “Given the massive global vaccination initiatives for COVID-19, we predict and hope that such answers will soon be forthcoming to facilitate more secure evidence-based strategies for corneal transplant protection.”
Table 1. Summary of the Four Cases of Corneal Transplant Rejection Following COVID-19 Vaccination
Transplant Type | Time to Presentation | Outcomes after Steroid Initiation | |
Case 1 | DMEK (6 months ago) | 3 weeks post-1st dose | endothelial rejection line appeared fainter with improvement in visual acuity and corneal edema 5 weeks after diagnosis |
Case 2 | PK (9 years ago) | 9 days post-2nd dose | complete resolution of corneal stromal edema and rejection line |
Case 3 | DSAEK | 2 weeks post-2nd dose | initial improvement with steroid treatment, resolution of anterior chamber cells and improvement in stromal edema |
Case 4 | PK | 2 weeks post-2nd dose | initial improvement with steroid treatment, reduced keratic precipitates and complete resolution of corneal edema, anterior chamber cells and flare |
Shah AP, Dzhaber D, Kenyon KR, et al. Acute corneal transplant rejection after COVID-19 vaccination. Cornea. 2022;41:121-124. |

