 |
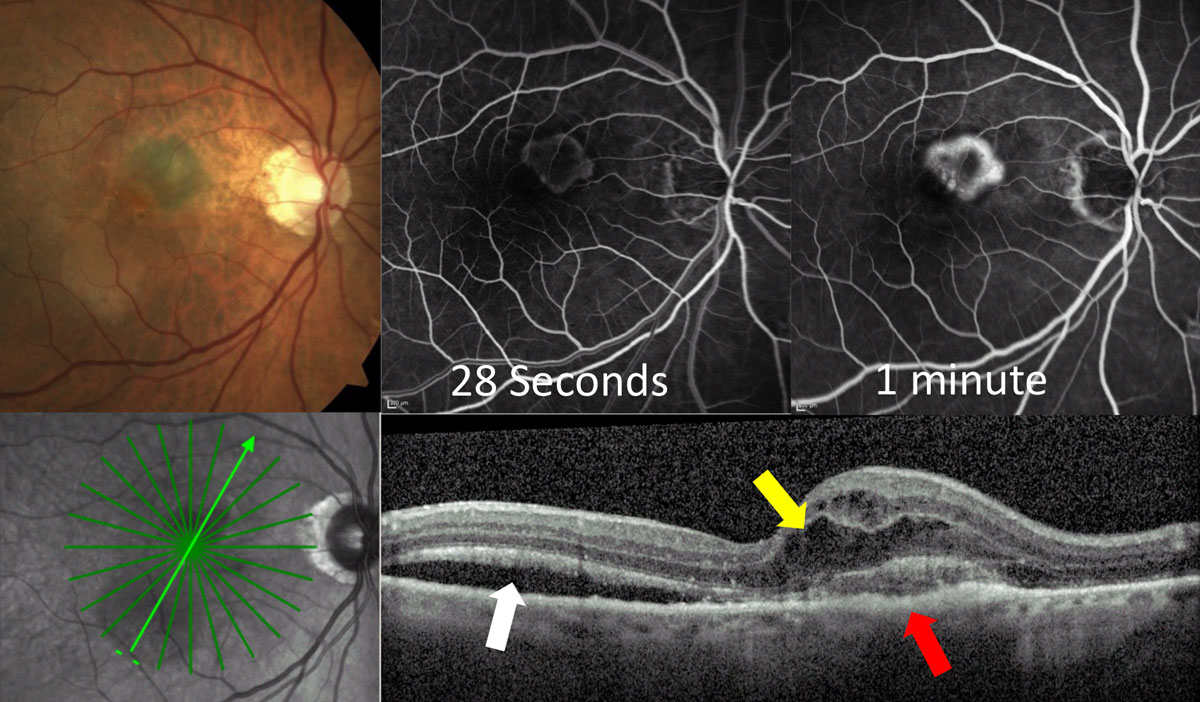
The connection between kidney function and AMD may be attributed to shared risk and genetic factors and pathogenic mechanisms. Notably, only late AMD (and not early AMD) showed an association with compromised kidney function in this study. Photo: Jessica Haynes, OD. Click image to enlarge. |
As chronic kidney disease (CKD) and age-related macular degeneration (AMD) share some of the same risk factors, pathogenic mechanisms and genetic polymorphisms, researchers have speculated that there may be a correlation between renal function and AMD. To further investigate this possibility, a team in Asia conducted a large cross-sectional study that revealed an association between CKD and late AMD, but none between kidney disease and early AMD.
Participant data (n=51,253) was gathered from 10 population-based Asian studies. Definitions for early AMD combined criteria in three different grading scales but generally included soft drusen and RPE changes. Late AMD was defined by the presence of either geographic atrophy or neovascularization and CKD was defined as estimated glomerular filtration rate (eGFR) below 60mL/min/1.73m².
The researchers performed a pooled analysis to examine the associations between CKD and eGFR with AMD (early and late), adjusting for confounders including age, sex, hypertension, diabetes, body mass index, smoking status, total cholesterol and study groups.
The mean age of participants was 54.1 years. The percentage of the cohort with CKD, early AMD and late AMD was 9.9%, 9.0% and 0.71%, respectively. After confounder adjustment, the researchers found that CKD was associated with higher odds of late AMD (odds ratio, OR: 1.46). Poorer kidney function was also associated with late AMD (OR: 1.12). Neither CKD nor eGFR were significantly associated with early AMD.
The lack of an association between renal function and AMD in its early stage suggests “a nuanced relationship between kidney function and different stages of AMD, warranting deeper exploration,” the researchers wrote in their paper on the study, published recently in Ophthalmology. “Importantly,” they added, “our current findings warrant further evaluation of kidney function as a predictor for the progression of AMD from early to late stages.”
This study is certainly not the first to draw a parallel between CKD and late-stage AMD; for example, one from 2011 found a significant association between a higher prevalence of CKD and late AMD but not early AMD. More recently in 2017, a study based in Taiwan reported an association between mild to moderate CKD and AMD, which was most prominent in late AMD, and another from that same year found that reduced eGFR was significantly associated with the presence of geographic atrophy.
Causal links between reduced kidney function and increased AMD must still be elucidated, but current research shows that the connection “may be attributed to shared influencing factors including common susceptibility genes like complement factor H and apolipoprotein E, as well as overlapping pathogenetic mechanisms such as the upregulation of the renin-angiotensin aldosterone system.” Furthermore, “CKD may lead to increased oxidative stress due to reduced glomerular filtration of free radical-generating nitrogenous waste products. The heightened oxidative stress can accelerate lipid deposition within Bruch’s membrane, which can further contribute to the degeneration and calcification of elastin and collagen,” the study authors wrote.
The researchers concluded that the observed association between compromised kidney function and late AMD further underscores the importance of ocular examinations in individuals with kidney disease.
Xue CC, Sim R, Chee ML, et al. Is kidney function associated with age-related macular degeneration? Findings from the Asian Eye Epidemiology Consortium. Ophthalmology. December 29, 2023. [Epub ahead of print]. |

