Herpes simplex virus (HSV) is a major health concern. This is evidenced by the epidemic of genital herpes and the enhanced acquisition of human immunodeficiency virus (HIV) associated with HSV.1 Its prevalence in the ocular world is just as strong, with HSV keratitis (HSVK) standing as the leading infectious cause of corneal blindness among developed nations, primarily because of its recurrent nature.2 Here, you’ll find a review of HSVK, including proper differential diagnosis and contemporary antiviral medical management.
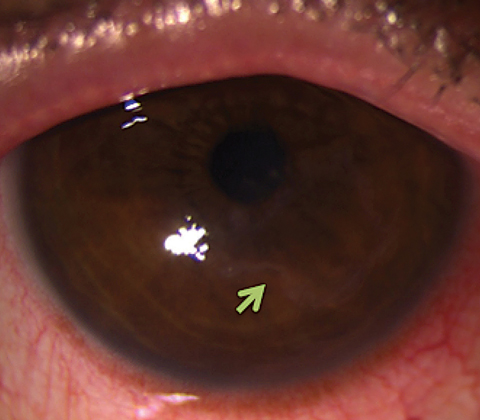 |
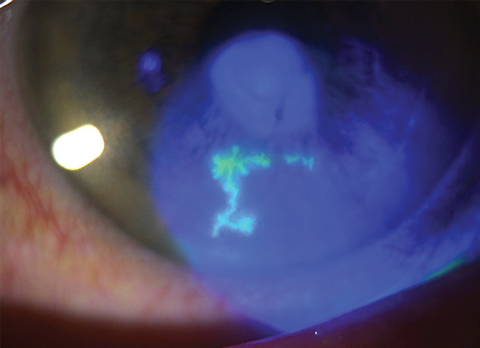
| Advanced dendritic lesions during HSV epithelial keratitis can result in geographic ulcers (green arrow). These defects are more diffuse in appearance, but still maintain branched features along their borders. Photo: Lisa Martén, MD |
Assessing the Eye
Humans are the only known natural reservoir for HSV. Along with the nose and mouth, the eyes are a main access point (Table 1).3 Systemic viral infections from other areas of the body may also manifest in the ocular tissues, resulting in potentially sight-threatening complications.
HSV-related ocular disease is classified as either primary or recurrent. It is also classified as blepharitis, conjunctivitis, HSVK, iridocyclitis or retinitis based on the specific ocular tissues affected.
HSVK is classified by the location of the principal site of corneal involvement. This includes HSVK of the epithelium (HSV epithelial keratitis), HSVK of the stroma (HSV stromal keratitis with or without ulceration) and HSVK of the endothelium (HSV endothelial keratitis).4
Ocular complications of HSV include lid, conjunctival and corneal involvement, as well as intraocular infections and retinitis.2,5 Approximately 72% of ocular HSV disease involves the corneal epithelium; 41% involves the lid or conjunctiva; 12% affects the corneal stroma; and 9% involves the iris and associated uveal tract.
Primary ocular HSV infections typically involve rapidly spreading corneal dendrites or geographic ulcers in the epithelium, as there is no antibody in the tear film to act against the virus. In these cases, there is no associated immune reaction to cloud the stroma or deeper ocular tissues.6,7
Those undergoing chemotherapy, recipients of bone marrow or organ transplants and people with HIV infection can develop multiple and extensive lesions. In some cases, visceral spread may occur.2,3,5
Table 1. Major Viruses of Ophthalmic Significance3 | |
| DNA | |
| Family | Ophthalmic Involvement |
| Adenoviridae |
|
| Herpesviridae |
|
| Papoviridae |
|
| Poxviridae |
|
| RNA | |
| Togaviridae |
|
| Retroviridae |
|
HSV-1 or HSV-2?
An estimated 3.7 billion people under age 50 worldwide have HSV-1 infection.8 HSV-1 is transmitted primarily through direct contact with infected secretions (i.e., saliva or tears) or lesions. Complications of HSV-1 infection occur mainly in the orofacial and ocular areas, but they can also include genital herpes.5,8,9
HSV-2 is less prevalent, with an estimated 417 million people ages 15 to 49 affected worldwide.8 It is sexually transmitted and causes genital herpes. The decreasing prevalence of HSV-1 before puberty in affluent and developed countries, and the increase in orogenital sexual practice, have led to a change in the epidemiology of HSV-1 and HSV-2. HSV-1 is now causing disease in a territory formerly inhabited exclusively by HSV-2 and vice-versa.9
Recurrences of HSV may be triggered by fever, hormonal changes, ultraviolet exposure, psychological stress, ocular surgery, ocular trauma and trigeminal nerve manipulation.5,8 Although pregnant women do not fit the traditional definition of immunosuppressed, the changes in immune response due to the pregnancy increase the risk of both primary and recurrent HSV infections.10 HSV-1 tends to recur in the orofacial area but not in the genital area after primary infection; conversely, HSV-2 tends to recur in the genital area but not in the orofacial area after primary infection.9
Both HSV-1 and HSV-2 infections are lifelong. Vaccines have been ineffective to date, but researchers continue to study the possibilites.8
 |
 |
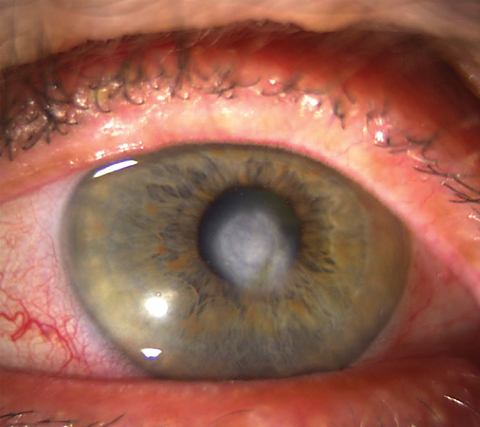
| On top, significant scarring from deep corneal inflammation, which is one of the most common causes of vision loss in HSVK. Below, keratic precipitates with anterior chamber reaction and stromal haze, which are hallmarks of HSV endothelial keratitis. Click images to enlarge. Photos: Lisa Martén, MD |
Making the Diagnosis
HSVK is often diagnosed without the need for laboratory testing, so an understanding of the clinical signs and symptoms is critical. Proper diagnosis begins with a detailed history. Optometrists should elicit the exact clinical course of the patient’s symptoms. Some history items to probe include HSV recurrence, contact lens wear, medical and systemic history, nasal and oral cold sore history, recent topical or systemic steroid treatment and recent fever or ultraviolet light exposure.4,11 The clinician should ask also about recent ocular surgery or trauma, previous corneal abrasions and recurrent erosions. This will help to narrow down the list of differential diagnoses.
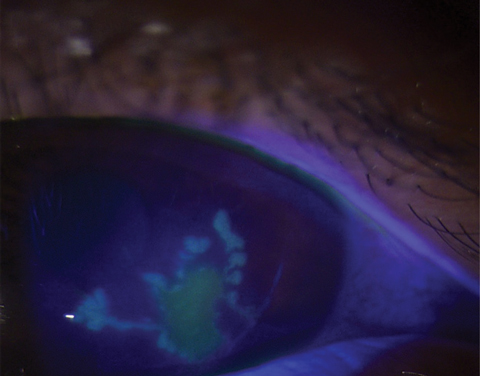
During the clinical examination, if the patient presents with skin vesicles, note their distribution. For example, vesicles on the forehead, scalp and nose that respect the vertical midline are more suggestive of varicella-zoster (VZV) than HSV.11 The slit lamp examination should include a detailed evaluation of the cornea. Vital dye staining with fluorescein and either rose bengal or lissamine green should also be performed. The typical epithelial lesion in HSVK presents as a true dendritic ulcer with terminal endbulbs.12 This is different from the presentation of VZV keratitis (VZVK), which usually presents as a pseudodendrite without terminal bulb staining. In differentiating HSVK from VZVK, remember that ulceration is frequently present in an HSV dendrite. Conversely, there is frequently minimal or no ulceration or epithelial defect in a VZVK pseudodendrite.
It is also prudent to evaluate corneal sensitivity bilaterally.9 Unlike other microbial infections and corneal abrasions, where corneal sensitivity is heightened, patients with HSVK often present with decreased sensitivity in the involved eye relative to the fellow eye.11 To test this, gently apply a cotton swab to the patient’s cornea and evaluate the blink reflex. You should test the uninvolved eye first so the patient can use it as a basis for comparison. A higher or lower sensitivity in one eye may manifest as a subjective increase or decrease of feeling, touch or sensitivity.
HSV has the ability to establish a latent infection. This allows it to live in the host without inducing pathology. As a result, it is difficult to detect. While laboratory testing is generally not needed to establish a diagnosis of HSVK, it can help to provide confirmation in the rare complicated case where the diagnosis is in doubt. The standard in diagnosis of HSVK is viral isolation in a culture.13 Due to potentially lengthy turnaround time, standard HSV culture is not useful for rapid clinical diagnosis.
Additional tests that can be conducted include Giemsa stains of the cornea and skin scrapings, enzyme-linked immunosorbent assay testing, HSV antibody titers and polymerase chain reaction assays.4,11,13 Serology is of limited use because there is a high prevalence of antibodies in the normal population. These tests are only positive when a live virus is present (as seen in HSV epithelial keratitis) and cannot be used to diagnose, or exclude, active disease caused by immunologic reactions against HSV triggered by prior infections, which is typically the case for HSV stromal keratitis.
 |
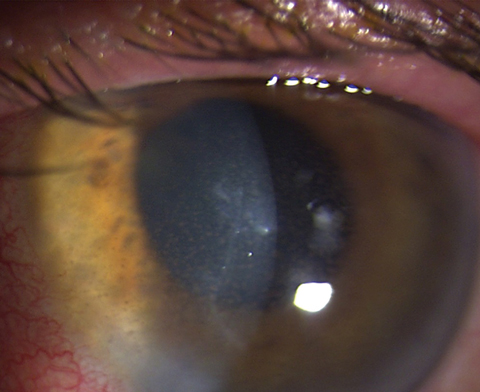
| HSV epithelial keratitis doesn’t always present with the classic corneal dendrite. Sometimes, the epithelial defect will be more coalesced in appearance. Photo: Lisa Martén, MD |
HSVK or a Masquerader?
The initial presentation of ocular HSV may or may not represent primary infection by the virus. In one study of 108 adult patients with primary ocular HSV, 84% of patients had moderate to severe conjunctivitis, 38% had moderate to severe blepharitis, 35% had a concomitant upper respiratory infection and 31% had generalized symptoms. Only 15% of patients had dendritic ulcers, while 2% had HSV endothelial keratitis and 19% had bilateral disease.14
Because of its variable presentation and ability to affect all corneal layers, HSVK has several masqueraders and differential diagnoses. For example, any keratitis that creates a dendriform lesion could be mistaken for HSV epithelial keratitis. Infectious masqueraders include Acanthamoeba keratitis, VZVK, adenovirus epithelial keratitis, Epstein-Barr epithelial keratitis, chlamydial keratitis and other varying microbial keratitis.4,12 Non-infectious differentials include Thygeson’s superficial punctate keratopathy, exposure keratopathy, epithelial defects from topical medications (i.e., antivirals and beta-blockers), epithelial defects due to contact lens wear, epithelial regeneration lines, epithelial basement membrane disease and recurrent corneal erosions.4,12 Appropriate patient history, demographics and a comprehensive workup will help you sift through masqueraders.
There are several differential diagnoses for both HSV stromal keratitis and HSV endothelial keratitis. Differentials for HSV stromal keratitis include an exhaustive list of interstitial and microbial keratitides. In diagnosing HSV stromal keratitis without ulceration, consider other interstitial keratitides such as that caused by syphilis, Cogan’s syndrome, Lyme disease, leprosy, lymphoma, tuberculosis and sarcoidosis.4,12 When diagnosing HSV stromal keratitis with ulceration, consider all forms of microbial keratitis as well as exposure and neurotropic keratopathy.4,12
Of the different types of HSVK, endothelial is the least common. The presence of stromal and epithelial edema with inflammation at the level of the endothelium, signified by keratic precipitates in the absence of significant anterior uveitis, is classified as endothelial keratitis. The list of differential diagnoses for HSV endothelial keratitis is the same as that for stromal keratitis, in addition to any form of keratouveitis, Posner-Schlossman syndrome, cytomegalovirus endothelial keratitis and corneal graft rejection.4,12 These differential diagnoses frequently present with raised intraocular pressure (IOP). Herpetic eye disease should be considered the cause of acute-onset, unilateral corneal edema unless proven otherwise.
The wide variety of conditions that can masquerade as HSVK makes the history and work-up vital to a correct diagnosis. In any case of epithelial, stromal or endothelial keratitis, if the patient’s story does not fit the clinical findings, then HSVK should be at the top of your differentials.
 |
| Here is an example of the classic HSVK epithelial dendrite with terminal bulbs. Photo: Lisa Martén, MD |
Treatment
Once a diagnosis has been made, focus should shift to treatment.
HSV epithelial keratitis is thought to account for 50% to 80% of all ocular herpes infections.13 HSV epithelial keratitis is the result of the virus’ destruction of corneal epithelial cells secondary to viral replication.13 Patients often present with the classic symptoms of HSV ocular infection such as redness, tearing, foreign body sensation, pain, photophobia and blurred vision.11,12,15
The cornea generally shows diffuse punctate areas that eventually coalesce into a distinct dendritic lesion with terminal bulbs.12 If the ulcer is more advanced, a more diffuse epithelial lesion, known as a geographic ulcer, will be present.
The Herpetic Eye Disease Study (HEDS) I showed no benefit in combining both oral and topical antivirals, so choose one course of treatment.15 One exception to this may be prescribing for immunocompromised patients with HSV epithelial keratitis, as the prevalence of acyclovir-resistant (ACVR) HSV-1 isolates is much higher (4.3% to 14%) than that in immunocompetent patients (0.1% to 0.6%).16 This difference is likely due to longer mucosal persistence of ACVR HSV variants. Therefore, it may be prudent to treat immunocompromised patients with HSVK both systemically and topically.
HSV epithelial keratitis is usually treated with antiviral medication, which may be topically applied or systemically administered. The two most common topical antiviral agents include Viroptic (trifluridine 1%, Pfizer) and Zirgan (ganciclovir 0.15%, Bausch + Lomb). Both of these agents are FDA approved for treating HSVK. Viroptic is generally dosed one drop nine times daily in the affected eye until the ulcer is resolved, whereas Zirgan is dosed one drop five times daily until the ulcer is resolved, then three times daily for seven additional days. Viroptic is effective, but also known for its toxicity, which can delay corneal healing. As a result, Zirgan is often the topical treatment of choice.
Unlike topical antivirals, oral antiviral medications should be used with caution in patients with kidney or liver disease due to the internal processing (i.e., metabolism, excretion) of these agents. Available oral formulations include Zovirax (acyclovir, GlaxoSmithKline), Valtrex (valacyclovir, GlaxoSmithKline) and Famvir (famciclovir, Novartis).
Oral antivirals tend to be the treatment of choice for HSV epithelial keratitis because they are often less expensive than topical agents, and the dosing schedule is more adaptable to daily use (Table 2).
In addition to prescribing antiviral therapy, clinicians should stabilize the ocular surface by prescribing preservative-free tear supplements. Topical immunomodulatory medications may be added for increased tear production and anti-inflammatory support. Lacrimal plugs and bandage contact lenses may be implemented in long-term ocular surface management.
Table 2. Oral Antiviral Therapy Dosing4 | |
| Dendritic Epithelial Keratitis (Seven to 10 days) | |
| Antiviral | Dosage |
| Acyclovir | 400mg five times daily |
| Valacyclovir | 500mg three times daily |
| Famciclovir | 250mg two or three times daily |
| Geographic Epithelial Keratitis (14 to 21 days) | |
| Acyclovir | 800mg five times daily |
| Valacyclovir | 1g three times daily |
| Famciclovir | 500mg three times daily |
| Stromal Keratitis Without Ulceration* (At least 10 weeks) | |
| Acyclovir | 400mg two times daily |
| Valacyclovir | 500mg once daily |
| Famciclovir | 250mg two times daily |
| Stromal Keratitis With Ulceration** (Seven to 10 days) | |
| Acyclovir | 800mg three to five times daily |
| Valacyclovir | 1g three times daily |
| Famciclovir | 500mg two times daily |
| Endothelial Keratitis*** (Variable) | |
| Acyclovir | 400mg three to five times daily |
| Valacyclovir | 500mg two times daily |
| Famciclovir | 250mg two times daily |
| Prophylaxis of Recurrent HSVK (At least one year) | |
| Acyclovir | 400mg two times daily |
| Valacyclovir | 500mg once daily |
| Famciclovir | 250mg two times daily |
| *Antiviral treatment is prophylactic since patients are also treated with a therapeutic dose of topical steroid. **Limited dose of topical steroid plus therapeutic dose of antiviral. ***Therapeutic dose of topical steroid and therapeutic dose of antiviral. Oral antiviral agent is reduced to prophylactic dose after seven to 10 days and maintained as long as steroid is in use. | |
HSV stromal keratitis without epithelial ulceration is the more common of the two HSV stromal infections. As its name implies, stromal keratitis without ulceration is thought to occur due to viral proteins that remain in the cornea even after the infection has resolved.17 In response to these remaining proteins, the body produces an inflammatory response, which results in a stromal keratitis without necrosis. Patients will generally present with symptoms of blurry vision, photophobia and halos around lights brought on by edema of the stroma.15
Clinical signs include stromal edema, anterior chamber reaction, stromal opacity and neovascularization.13 This significant inflammatory response, in combination with recurrent disease, often makes stromal keratitis the instigator of irreversible damage and significant scarring. Stromal keratitis without ulceration requires the use of a topical corticosteroid along with an oral antiviral.
HSV stromal keratitis with ulceration is, fortunately, less common than stromal keratitis without ulceration. Stromal keratitis with ulceration is also an immune-mediated response to the proteins left behind in the stroma.12 However, instead of producing inflammation, the cells signal tissue necrosis, resulting in ulceration and, ultimately, stromal bed destruction.
Clinical symptoms are similar between the two types of stromal keratitis. Patients with HSV stromal keratitis with ulceration present with necrosis of the stromal tissue. This results in an opacification of the stroma, which can lead to thinning of the tissue and increased risk of corneal perforation.12
The treatment of stromal keratitis with ulceration is still commonly debated. A limited number of studies exist regarding treatment; thus, a well-established protocol does not exist. It is thought, however, that similar to stromal keratitis without ulceration, a combination of topical corticosteroids and oral antivirals is best suited to treat stromal keratitis with ulceration.4
HSV endothelial keratitis stems from inflammation due to viral proteins within the corneal endothelium.13 Patients with HSV endothelial keratitis present with symptoms similar to other forms of HSVK, including pain, redness, photophobia and blurry vision. HSV endothelial keratitis is also marked by a deep stromal opacification with anterior chamber reaction, keratic precipitates and, occasionally, elevated IOP.12 The elevation of IOP is a common sign of endotheliitis and should never be overlooked. Much like its stromal counterpart, HSV endothelial keratitis is thought to respond well to a combination of oral antivirals and topical corticosteroids. Because Zirgan and Viroptic do not penetrate the cornea deeply, oral antivirals are the preferred method of treating HSV endothelial keratitis.4
Post-HSVK eyes should be carefully monitored for IOP rise secondary to trabeculitis.17 In some cases, long-term use of topical steroids is needed to prevent future flare-ups and scarring. Whenever corticosteroids are used with a patient with previous history of HSV ocular infection, antivirals are needed to prevent recurrence.
For patients with significant corneal scarring from recurrent HSVK episodes, consider use of an amniotic membrane to boost corneal repair. Although not considered a first-line treatment for HSVK, amniotic membranes can help decrease inflammation and provide the building blocks to heal corneal tissue. Even when scarring appears to be beyond repair, these devices may be able to improve the corneal appearance and give the ocular surface a second chance.
Surgical intervention is seldom necessary in the management of HSVK. Progressive stromal thinning with impending or actual perforation may occur, although it is rare. Conservative surgical intervention with application of cyanoacrylate glue is usually sufficient, although tectonic keratoplasty may be required to preserve the integrity of the globe. Adjunctive temporary or permanent tarsorrhaphy is recommended in such cases.
When Acute Becomes Chronic
A maintenance dose of systemic antiviral therapy may help some patients with HSVK. In the HEDS II study, a maintenance dose of either 400mg of acyclovir BID or 500mg valacyclovir QD for 12 months after resolution of the initial episode significantly decreased the probability of recurrence.18 Patients who have had more than one episode of HSVK and those with HSV stromal keratitis are prime candidates for a maintenance course of antiviral medication, which can often spare patients significant scarring and loss of vision.
HSVK is the most frequent cause of corneal blindness in the United States and the most common source of infectious blindness in the Western world.2 A detailed, targeted history and meticulous clinical work-up are essential to proper diagnosis, effective treatment and preservation of visual function. With timely, aggressive treatment, the prognosis in HSVK is generally favorable.
Dr. Leon is an optometrist at the South Texas Eye Institute. She is a graduate of the Rosenberg School of Optometry at the University of the Incarnate Word, where she completed a residency in primary care optometry.
Dr. Pizzimenti is a full-time faculty member at the University of the Incarnate Word in San Antonio, Texas, where he coordinates the Primary Care Residency Program. He is also a contributing editor for Review of Optometry.
| 1. Freeman EE, Weiss HA, Glynn JR, et al. Herpes simplex virus 2 infection increases HIV acquisition in men and women: systematic review and meta-analysis of longitudinal studies. Aids. 2006;20(1):73-83. 2. Farooq AV, Shukla D. Herpes simplex epithelial and stromal keratitis: an epidemiologic update. Surv Ophthalmol. 2012;57(5):448–62. 3. Harding SP. Viral infections of the eye. Reviews in Medical Virology. 1993:161-71. 4. White ML, Chodosh J. Herpes simplex virus keratitis: a treatment guideline. The American Academy of Ophthalmology Clinical Guidelines. June 2014. 5. Kaye S, Choudhary A. Herpes simplex keratitis. Prog Retin Eye Res. 2006;2(4):355-80. 6. Pavan-Langston D. Part one: the research perspective. Advances in the management of ocular herpetic disease. Candeo Clin Sci Comm. 2011;1-9. 7. Toma HS, Murina AT, Areaux RG Jr, et al. Ocular HSV-1 latency, reactivation and recurrent disease. Semin Ophthalmol. 2008;23(4):249-73. 8. World Health Organization fact sheet on herpes simplex virus. www.who.int/mediacentre/factsheets/fs400/en/. January 2017. Accessed June 15, 2017. 9. Azher TN, Yin XT, Tajfirouz D, et al. Herpes simplex keratitis: challenges in diagnosis and clinical management. Clin Ophthalmol. 2017;11:185-191. 10. Langford KS. Infectious disease and pregnancy. Obsestrics, Gynaecology and Reproductive Medicine. 2002;12(3):125-30. 11. Rabinowitz MP. Herpes simplex virus. Wills Eye Manual Office and Emergency Room Diagnosis and Treatment of Eye Disease. 6th ed. Philadelphia: Lippincott Williams & Wilkins; 2012. 12. Hill GM, Ku ES, Dwarakanathan S. Herpes simplex keratitis. Disease-a-Month. 2014;60(6):239-46. 13. Zhu L, Zhu H. Ocular herpes: the pathophysiology, management and treatment of herpetic eye diseases. Virologica Sinica. 2014;29(6):327-42. 14. Liesegang, TJ. Herpes simplex virus epidemiology and ocular importance. Cornea. 2001;20(1):1-13. 15. Murphy C, Shahnazaryan D. Managing herpes simplex keratitis. Iris Medical Times. 2011;45(16):35. 16. Duan R, de Vries RD, Osterhaus ADME, et al. Acyclovir-resistant corneal HSV-1 isolates from patients with herpetic keratitis. J Infect Dis. 2008;198(5):659-63. 17. Adams MJ, Carstens EB. Ratification vote on taxonomic proposals to the International Committee on Taxonomy of Viruses. Arch Virol. 2012;157(7):1411–22. 18. Wilhelmus KR, Beck RW, Moke PS, et al. Acyclovir for the prevention of recurrent herpes simplex virus eye disease. N Engl J Med. 1998;339:300-6. |

