 |
History
A 27-year-old black female was referred to the office by another local practitioner in the hopes that we would investigate an unusual, brown corneal ulcer in her right eye, with specific instructions to rule out fungal infection.
Her history uncovered that she had felt something in that eye since last week after working in the garden. She explained that her eye had been red and painful for the last four days, but that her vision was intact. She went to her own eye doctor the day before.
Her systemic history was noncontributory.
Diagnostic Data
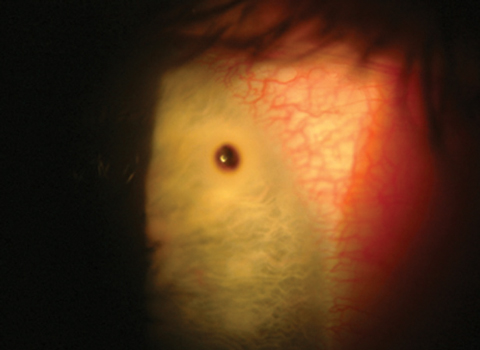
Her best corrected entering visual acuities were 20/20 OD and 20/20 OS at distance and near. Her external examination was normal with no evidence of afferent pupil defect. The biomicroscopic examination of the anterior segment shows the lesion (Figure). Goldmann applanation tonometry measured 15mm Hg OU.
Dilated examination uncovered normal posterior poles with no peripheral pathologies OU.
Your Diagnosis
Does the case presented require any additional tests, history or information? What steps would you take to manage this patient? Based on the information provided, what would be your diagnosis? What do you believe is the patient’s most likely prognosis?
 |
| This 27-year-old patient has suffered from a red painful eye for approximately four days. Could an incident in her garden be related to this ocular finding? |
Diagnosis
Additional studies included sodium fluorescein staining of the lesion, the Seidel test, corneal sensitivity and eye-lid eversion.
The diagnosis in this issue is metallic intracorneal foreign body with rust deposition. Most of the time, corneal foreign body injuries present as an emergency following acute injury, making them a common urgent clinical entity of ophthalmic practice.1-12 Patients with corneal foreign body present with acute pain, photophobia, pain upon extraocular muscle movement, lacrimation, blepharospasm, foreign body sensation, variably blurry vision depending upon the location of the particle and a history of having something “go in their eye.”1-9 Light biomicroscopy of the injured area often reveals diffuse corneal edema and epithelial disruption. In severe cases, when edema is excessive, folds in Descemet’s membrane may be visible. Circumlimbal injection with a greater density of conjunctival erythema adjacent to the site of injury is common if the missile created enough damage to induce iritis. Iridocyclitis is marked by the observation of cells and proteinaceous flare in the anterior chamber.1-9 Cobalt blue light inspection, with the instillation of sodium fluorescein dye, will illuminate the damaged cornea and indirect lighting using the sclerotic scatter technique will back-light it.8 Research shows no gender predilection specifically, however, the majority of affected individuals are typically younger than age 20, and male.12-15 Inorganic foreign bodies (plastic, glass) tend to be better tolerated than organic (wood).9
Workshop and construction tools and motorized lawn equipment are notable sources of ocular injury among males.12,14,16,17
The cornea has five distinct layers:
- The corneal epithelium,
- Bowman’s membrane (a whirling structure designed to prevent penetrating injuries),
- The organized 250 lamellar sheet stroma
- Descemet’s membrane
- The metabolic endothelium.19-24
Corneal foreign bodies injuries are divided into two categories; superficial, not involving Bowman’s membrane and deep, penetrating Bowman’s membrane, but not rupturing Descemet’s membrane. Corneal foreign bodies typically enter the epithelium but are prevented from penetrating deep into the tissue by the whirling and stiff Bowman’s membrane.23 Foreign bodies coming to rest below the Bowman’s membrane will disrupt layers of the cornea that have no mechanism for recreating the specific architecture that permitted them to be transparent. This means foreign bodies piercing the Bowman’s membrane will leave a permanent scar.15,16
The cornea has remarkable healing properties. The epithelium adjacent to any insult expands in size to fill in the defect, usually within 24 to 48 hours.18 Below the epithelium, no mechanism for cellular replacement exists. Here, cells enlarge (polymegathism), change shape (pleomorphism) or move over.24 Lesions that are purely epithelial often heal quickly and completely without scarring. Unfortunately, if there is any colatteral destruction of limbal stem cells, superficial corneal injuries may develop into recurrent epithelial ulcerations, chronic stromal ulcers, develop deep stromal vascularization or develop conjunctival overlap.25-27 Corneal avascularity is moderated by anti-angiogenic factors.26,27 These factors counterbalance pro-angiogenic/lymphangiogenic factors that are constantly available, becoming upregulated during wound healing.27 Angiogenic proteins (vascular endothelial growth factor-VEGF and basic fibroblast growth factor-bFGF) and angiogenesis regulatory proteins along with matrix metalloproteinases and lymphangiogenic regulatory proteins all play vital roles during corneal wound healing.27
All corneal injuries induce an inflammatory reaction which exerts trophic influences in the corneal epithelium, damaging sensory nerves.28 Alterations in normal healing disrupts the integrity and function of the tissue with undesirable consequences, ranging from inability to wet with resultant loss of transparency to infectious ulceration and perforation.28
Treatment for corneal foreign body begins with a brief, problem oriented history. Since patients with these injuries are often in distress, the process should be streamlined and succinct. The time, place and activity surrounding the injury should be recorded for both medical understanding and legal purposes. Visual acuity (VA) should be recorded, if possible, before any procedures or drops are given. If the blepharospasm is sufficiently intense, precluding acuity measurement, one drop of topical anesthetic can be administered with the VA measured immediately after. The eye examination should begin with an evaluation of the pupils and an external evaluation of the adnexa and then proceed to biomicroscopy. The eyelids should be everted and fornicies scrutinized to rule out the presence of scattered foreign material. Fluorescein dye (preferably without anesthetic) should be instilled to assist in identifying corneal defects and locating potential debris. The Seidel test (painting of the wound with fluorescein dye observing for aqueous leakage) should be performed if a full thickness cornea/globe perforation is suspected. Any injury should be documented for size, shape, location and depth. Corneal abrasions or lacerations should be cleaned and scrutinized for foreign matter. The anterior chamber should be observed for any evidence of uveitis. A dilated examination should be completed (either at time of initial evaluation or at follow-up) to rule out any posterior effects from the trauma and rule out penetrating foreign body.
Corneal foreign bodies can be removed using stream lavage, forceps, a cotton-tipped applicator, a spud or a loop, however, among the most popular instruments is the needle mounted on a syringe.29-33 The needle technique affords several advantages: reach, control over the size of the probe (23g to 30g, typically), sharpness for mild excavation, availability, inexpensive and easy of use. Generally, the procedure is accomplished following the administration of one or two drops of a topical anesthetic such as proparaciane, bupivacaine, alcane or teteracaine.32,33 If the patient is unable to maintain eye lid opening a lid speculum may be required. The patient should be instructed to maintain a gaze that affords the clinician the best lateral approach to the entrapped particle. The patient should be reminded that anesthesia has been applied and there will be no pain so as to create the best working environment for both parties. With the biomicroscope focused and locked on the foreign body illuminated with a direct or indirect light beam, the needle should be inserted between the patient and the slit lamp so it interrupts the light beam. As the examiner moves into position behind the oculars to view the area of regard, the needle will be in the way and out of focus. The needle can then be safely pushed back to the region locked in focus without risk of an accidental corneal breech. The object can then be safely dislodged and removed with a dry or anesthetic-moistened swab. If the corneal foreign body is a “corneal splinter” the best approach may be with a forceps, however, the technique for reaching the foreign body is still safe and sound.
In the event the foreign body is metallic and has produced a rust ring, the ring should be removed at the time the foreign body is removed so long as it determined to be safe from enlarging the potential scar zone. Some clinicians prefer the use of a motorized bur to lift superficial rust rings, however, often they inadvertently enlarge the region of corneal abrasion around the residual crater. In the event the risk-to-benefit ratio for rust removal is large, the rust can be left to dissipate or percolate to the surface during the healing process where it can be removed later.34 Rust ring infiltrate does not serve as an indicator of corneal inoculation or infection.35
The treatment for the residual superficial corneal injury is universal. Pain can be mitigated using adequate cycloplegia (determined on a case by case basis; atropine 1% QD-TID, for the worst and homatropine 5%, in the office, for the mildest), topical non-steroidal anti-inflammatory medication BID-QID and infection can be prevented using topical antibiotics.36-40 Bed rest, inactivity, cold compresses, artificial tear drops and over-the-counter analgesics (acetaminophen or ibuprofen) can be used to relieve acute pain. In cases where pain is severe, a thin, low-water-content bandage contact lens can be prescribed.38-43 Pressure patching is not contraindicated, however, it is no longer considered standard-of-care.38-43 Patients should be reevaluated every 24 hours until the injury demonstrates a restored epithelium.37-39 Topical lubricants and antibiotic ointment at bedtime can provide analgesia and cushioning to the lesion during the reparative process. Topical steroidal preparations can be added after the initial healing has taken place to prevent subepitheilial infiltration and to mitigate inflammation.
Some final pointers worth mentioning:
- Ointment should not be placed on the applicator used to lift foreign bodies from the cornea or conjunctiva. Contrary to myth, it doesn’t help the foreign body adhere to the applicator and the ointment reduces the visibility in the field,
- A peaked pupil, an eddy through the aqueous, a full thickness corneal scar, a full thickness lenticular opacity or disproportionate inflammatory response or plaque is indicative of a penetrating event or potential fungal seeding,
- High speed particles that are hot have the potential to enter the cornea and produce self-sealing wounds. Here, particles may enter the interior areas of the eye without producing a Seidel sign,
- To promote healing, prevent recurrent erosion and reduce corneal edema, a hypertonic solution or ointment may be prescribed along with the other medications or after reepithelialization has occurred,
- In cases where excess epithelium (a flap) impairs regrowth, a cotton-tipped applicator saturated with anesthetic may be used to debride the loose or excessive tissue.
- When a significant uveitis is present or if subepitheial infiltration occurs during the reparative process, topical steroids may be required. They must be used judiciously as they can retard corneal healing and raise intraocular pressure,
- Rapid aggressive subepithelial infiltration, increased pain and increased injection in the setting of an epithelial break may be a sign of infection. Lesions such as these should be considered vision threatening, warranting immediate treatment with a fourth generation fluoroquinolone antibiotic drops (if one is not already employed) and consideration for culture to determine the presence of an underlying microbial organism,
- All of the above mandate rapid follow up; patients may not have the ability to interpret whether the initial therapy is working, therefore it must be re-evaluated within 24 hours to 48 hours of the beginning of intervention.
| 1. Kumar NL, Black D, McClellan K. Daytime presentations to a metropolitan ophthalmic emergency department. Clin Experiment Ophthalmol. 2005;33(6):586-92. |

