 |
|
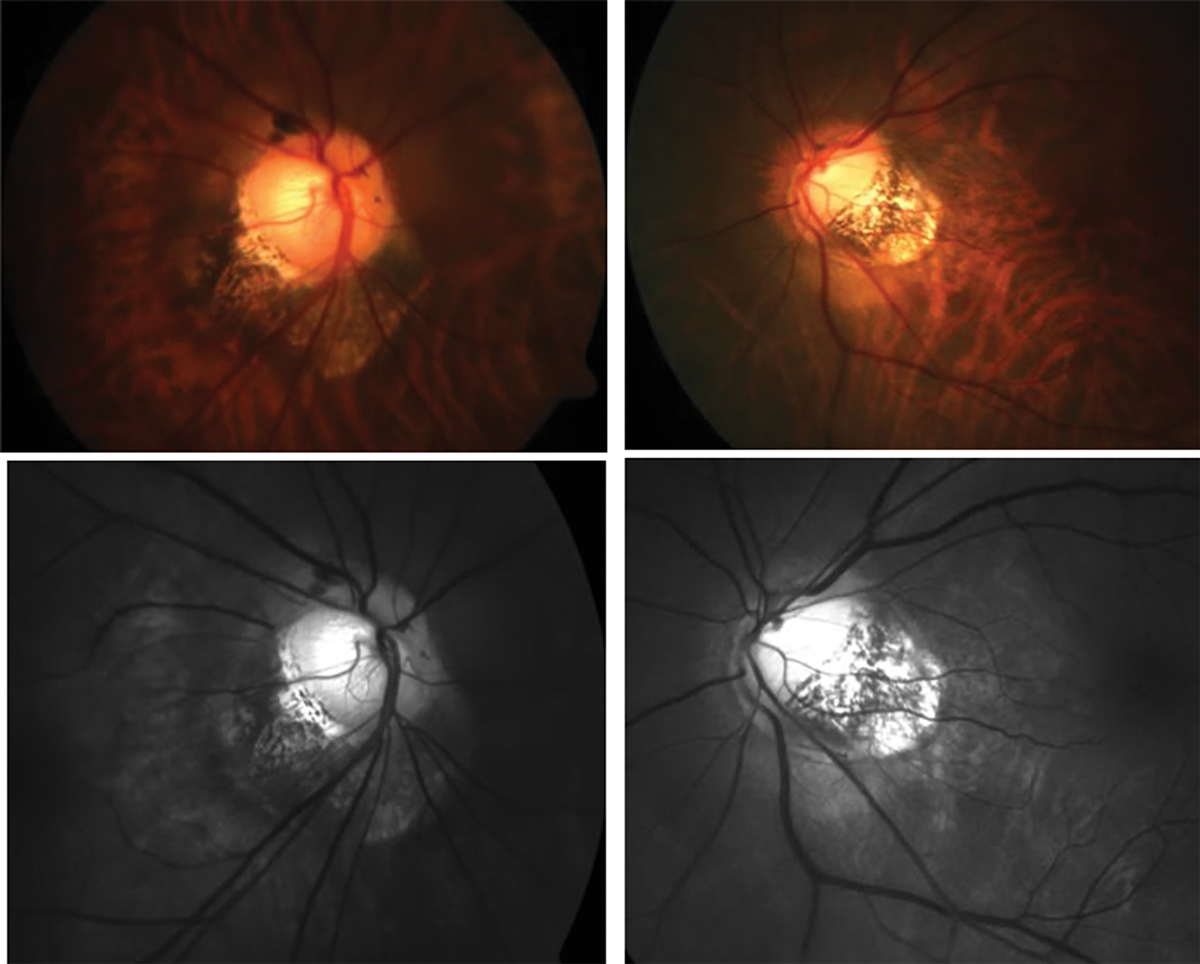
Assessing glaucoma progression on OCT can be unreliable in high myopes due to irregularities in the peripapillary region; however, assessing fundus photos chronologically may shine a light on which disease the observed changes are attributed to. Photo: Andrew Rouse, OD. Click image to enlarge. |
In patients with concurrent high myopia and glaucoma, identifying which structural changes are attributed to which disease can be challenging, yet doing so is critical to assess and manage disease progression properly. To complicate matters, OCT can be unreliable due to irregularities in the peripapillary region often found in high myopes. To catch and accurately interpret changes over time, it’s essential to routinely photograph these patients. A team of ophthalmologists recently demonstrated the benefit of this practice using the case of a highly myopic patient who was being treated only for glaucoma for several decades before the doctor discovered longitudinal structural changes pointing to high myopia after viewing the fundus photos chronologically.
The patient had first been diagnosed with pigmentary glaucoma in 1960 when she was 22 years old. She was treated off and on for several years, then consistently beginning in 1993 based on progressive optic nerve head (ONH) changes that were observed over the last seven years since routine black-and-white photography had begun. The patient developed slow long-term progression detected in the ONH, optic disc hemorrhages in both eyes and nuclear and posterior pole cataracts, which were operated on in 2003.
|
To learn more about similarities and differences between glaucoma and myopia, see this feature. |
The case report authors noted in their paper for Acta Ophthalmologica that “when comparing digital ONH photographs to the first paper prints taken in 1986 in Oulu, they looked dramatically so different and therefore raised a doubt about whether the photographs had been taken from the same patient. However,” they continued, “organizing the pictures in chronological order revealed uncommon longitudinal ONH and peripapillary changes in both eyes during the 36-year follow-up.”
They further explained that changes in the photos of both eyes taken from 1986 to 2000 “had been interpreted as glaucomatous progression in the upper and lower parts of the ONH, as indicated by the increased bending of the vessels towards the clinical disc margin. However, the subsequent images reveal that these changes actually continued further into profound progressive peripapillary scleral bowings; that is, bending of vessels along the cupping outside the disc margins in both eyes,” which none of the patients’ charts had previously reported. The authors speculate that previous ophthalmologists may have missed the progressive changes “jumping” outside the disc margins by only comparing the latest adjacent pictures with each other.
This case demonstrates several lessons on the importance of routine fundus photo documentation, as well as the long-term diagnostic and treatment challenges that may arise when managing glaucoma and/or highly myopic patients, the researchers argue. They can be summarized as follows:
1. A patient's diagnosis may change, and/or the patient may receive several diagnoses as time goes on, which may make it difficult to determine which of the structural and functional findings are related to each diagnosis. In this case, these included Krukenberg spindle, IOP that increased up to 30mm Hg on treatment, optic disc hemorrhages and myopia with tilted disc.
2. The clinicians were able to properly diagnose this patient only after observing routine one- to two-year fundus photos, which revealed longitudinal changes that were previously missed. “Compared to written interpretations by different clinicians, photographs are superior enabling retrospective re-evaluation of what has happened in the structures over the years and offer an opportunity to develop new diagnostic interpretations,” the authors wrote. “Without the series of photographs, we could not have learned that the progressive changes interpreted as being ‘typically glaucomatous' appeared later on to be related to myopia.”
3. It’s important to always evaluate progression by comparing the latest picture to the very first one. Obtaining and organizing patients’ records from previous eyecare providers is essential and easier now thanks to automated data recording tools.
4. Learning to detect whether certain clinical changes are related to glaucoma, myopia and/or aging requires the detailed examination of similar cases, the case report authors advise.
They concluded by asserting, “This essay demonstrates that routine photographic documentation of the fundus stands the test of time and promotes the continuous development of both clinical skills and deep learning algorithms.”
Tuulonen A, Kim TW, Chauhan BC, et al. The usefulness of routine photography in a myopic patient treated for glaucoma: 36-year follow-up. Acta Ophthalmologica. January 19, 2024. [Epub ahead of print]. |

