A 26-year-old black male presented complaining of redness and pain in his eyes that had persisted for three days. He said the pain felt as though a needle was poking his eyes. On a scale of one to five, with five representing the greatest discomfort, he described his level of itching as a three to five, with variability. He also had a watery discharge that was worse in the morning.
The patients ocular and medical history were unremarkable. He had tried contact lenses eight years earlier, but discontinued use shortly afterward. Family history showed that his grandfather had type II diabetes. The patient was not taking any medication and had no known drug allergies.
The patient did not have his medical record with him. He was a third-class petty officer in the Navy.
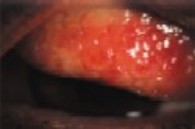 |
| Giant papillae on the upper tarsal conjunctiva are the hallmark clinical sign of vernal conjunctivitis. |
Diagnostic Data
Best-corrected visual acuity was 20/20-1 O.D. and 20/25-1 O.S, with a spectacle prescription of -4.50 -0.75 x 72 O.D. and -4.50 -1.50 x 93 O.S.
Slit lamp examination revealed giant papillae on lid eversion in the upper tarsal conjunctiva O.U. The bulbar conjunctiva in each eye was 1+ injected. Five limbal papillae were present in each eye. The cor-nea was clear, with no opacities or Trantas dots noted. The anterior chamber was deep and quiet. All other findings were unremarkable.
Diagnosis
I diagnosed vernal conjunctivitis vs. atopic conjunctivitis O.U.
Treatment and Follow-Up
I prescribed Patanol (olopatadine hydrochloride) bid for one week in both eyes and instructed the patient to return for a one-week follow-up.
The patient returned to the clinic four weeks later and re-ported no relief of symptoms. He had discontinued the Patanol after seven days with no improvement. The patient had been on sea patrol for two weeks, but returned to the clinic as soon as he could.
At this visit, best-corrected visual acuity was 20/20 O.D. and 20/25 O.S. IOP had risen slightly from 9 and 8mm Hg at his previous visit to 10mm Hg O.U. All other entrance testing was unchanged since his last visit.
Review of the patients past medical record validated my assessment. Upon further questioning, the pa-tient said that he had experienced exacerbations of the same signs and symptoms for the last three years and had suspected an infection.
I diagnosed the patient with vernal conjunctivitis O.U. I prescribed Pred Forte (prednisolone acetate) every four hours in both eyes and advised the patient to return for follow-up, including an IOP check, in one week, at which time he could begin tapering the drug to a maintenance dose for one month.
I advised the patient to discard the Patanol. I explained that he did not have an infection, but an aller-gy. I cautioned him that using topical steroids incorrectly could carry an increased risk for steroid-induced glaucoma, corneal damage secondary to abuse and possible cataracts. I also stressed the critical need for him to return for his follow-up exam when scheduled.
The patient returned for follow-up one week later and said he was feeling better. He had been using the Pred Forte as directed.
All entrance findings were consistent with the previous two examinations. IOP measured 10mm Hg O.D. and 13mm Hg O.S. Slit lamp examination showed some resolution of the previous findings. The bulbar conjunctiva revealed trace amounts of injection in both eyes. The giant papillae had shrunk to 2+ levels upon lid eversion, and the limbal papillae had resolved.
I determined that the patient had a re-solving vernal conjunctivitis O.U. The plan was to taper the Pred Forte as follows: qid for four days, tid for three days, bid for two days and once daily for three weeks. I told the patient to return to the clinic if the condition flared up or as needed.
| Treatment Options for VKC |
| Vernal conjunctivitis often responds to topical medications, but can sometimes be difficult to treat. Options for treating vernal conjunctivitis include: Mast cell stabilizers: Drugs like Crolom (cromolyn sodium), Alocril (nedocromil sodium) and Alamast (pemirolsat potassium) can be used concomitantly with corticosteroids. Mast cell stabilizer with antihistamine: Patanol and Zaditor (ketotifen fumarate) relieve itching associated with VKC. These require fewer instillations per day than other common treatments. Non-steroidal anti-inflammatory agents: Voltaren (diclofenac sodium) and Acular (ketorolac trometha-mine) are also indicated to relieve itching, though transient stinging is a common side effect. Topical corticosteroids: These include Pred Mild and Pred Forte. Know the risks of prolonged use or abuse of steroids, which include increased intraocular pressure, cataracts and a predisposition to infection.1 Educate the patient carefully. Immunosuppressant: Topical sandimmune (cyclo-sporine)4 is not approved for treatment of VKC, but has off-label indication for VKC resistant to general therapy. Oral antihistamines: Allegra (fexofenadine), Claritin (loratadine) and Zyrtec (cetirizine) may be indicated. Nitric oxide inhibitors: A recent study has shown NO inhibitors to be successful in treating severe allergic conjunctivitis.5 Chemotherapeutic: A recent trial showed Mutamy-cin (mitomycin C) to be effective in treatment of VKC.2 Other non-pharmaceutical options include debridement in the case of corneal plaques, laser phototherapuetic keratectomy or simple excision to prevent scarring and visual loss. A.A. |
Discussion
Vernal conjunctivitis, commonly referred to as VKC when the cornea is involved, is a chronic allergic conjunctivitis. It is almost twice as common in men in their teens and early 20s vs. women.1-3 Seasonal peak incidence tends to be in the warm months.2-4 However, it has been found year-round in some patients.2 Researchers estimate that vernal conjunctivitis comprises 0.5 percent of allergic eye disease.3
The precise immunopathologic mechanism is unknown, but the cause of VKC is thought to be more complex than a simple type I hypersensitivity reaction.3 We do know that mast cells, eosinophils and cytokines play pivotal roles in the pathogenesis of VKC, and that a cascade of chemical mediators and reactions are involved.1 Some be-lieve that genetics may play a role because vernal conjunctivitis has been associated with a familial history of atopy.1,4 Some atopic conditions include vernal conjunctivitis and atopic dermatitis. One study reported that the course of VKC might last 5-10 years, then resolve.4
Patients with vernal conjunctivitis exhibit intense itching, ropy discharge, redness, irritation, photo- phobia and foreign-body sensation.1-4 The hallmark sign is giant papillae on the upper tarsal conjunctiva.1-4 You may observe limbal papillae or edema along with cor-neal involvement in the form of superficial punctate keratitis and/or a shield-like ulcer.1-4 Such ulcers cause corneal plaques to form, which may lead to scarring and visual loss.
Bulbar edema may exist. This may lead to obstruction of the ductules of the lacrimal glands, causing dry eye syndrome.1 Lastly, you may note Trantas dots, a collection of eosinophils at the limbus.2,4
Differential Diagnosis
When itching is the chief complaint, an allergy is highly suspect. It is important to distinguish vernal conjunctivitis from other allergic conditions such as seasonal allergic conjunctivitis and atopic keratoconjunctivitis. Seasonal allergic conjunctivitis (SAC) is a self-limiting condition that usually exhibits small tarsal papillae.3 Atopic keratoconjunctivitis has prolonged symptoms and can have sight-threatening consequences.3
Your workup should begin with a thorough case history. VKC pa-tients may present with a past history of seasonal flare-ups, so ask them about exacerbations and re-missions. Perform a thorough slit lamp exam and evert the lids to look for giant papillae on the upper tarsal conjunctiva. If you suspect vernal conjunctivitis, pay particular attention to the limbus to note any SPK, shield ulcers, Trantas dots or limbal papillae. A quantitative tear test such as Schirmers would help determine if dry eye exists.
You may also wish to perform a conjunctival scraping and complete a differential quick stain to look for mast cells and eosinophils.4 An in-creased number of mast cells in the conjunctival epithelium is typical in patients with vernal conjunctivitis.1
As primary eye care providers, we must know how to diagnose vernal conjunctivitis and give our patients the relief from the intense symptoms that they experience. It is also our responsibility to properly educate patients about the cause and treatments of this condition.
Dr. Achilla is a U.S. Naval Officer (Lt.) at the Naval Medical Center in San Diego.
1. Tabbara KF. Ocular complications of vernal keratoconjunctivitis. Can J Ophthalmol 1999 Apr;34(2):88-92.
2. Akpek EK, Hasiripi H, Christen WG, Kalayci D. A randomized trial of low-dose, topical mitomycin-C in the treatment of severe vernal keratoconjunctivitis. Ophthalmology 2000 Feb;107(2):263-9.
3. McGill JI, Holgate ST, Church MK, Anderson DF, Bacon A. Allergic eye disease mechanisms. Br J Ophthalmol 1998 Oct;82(10):1203-14.
4. Friedman NJ, Pineda R, Kaiser PK. The Massachusetts Eye and Ear Infirmary Illustrated Manual of Ophthalmology. Philadelphia: W.B. Saunders Co., 1998:100.
5. Ko SM, Kim MK, Kim JC. The role of nitric oxide in experimental allergic conjunctivitis. Cornea. 2000 Jan;19(1):84-91.

