 |
| This study found that MNV lesion types may predict response to anti-VEGF treatment. Photo: Qiang W, et al. Front Neurosci 26 Aug 2021. Click image to enlarge. |
Anti-VEGF drugs are the mainstay treatment for neovascular age-related macular degeneration (nAMD) eyes, but the heterogeneity present among lesion types also can influence response to treatment. As such, identifying different baseline patient profiles could help practitioners individualize treatment approaches in order to achieve the best long-term results. In a new study published in Ophthalmology Retina, researchers evaluated the influence of macular neovascularization (MNV) lesion type on 12-month clinical outcomes in treatment-naïve eyes with nAMD eyes treated with anti-VEGF drugs and found many type-specific differences in baseline VA, improvement in acuity and change in lesion activity.
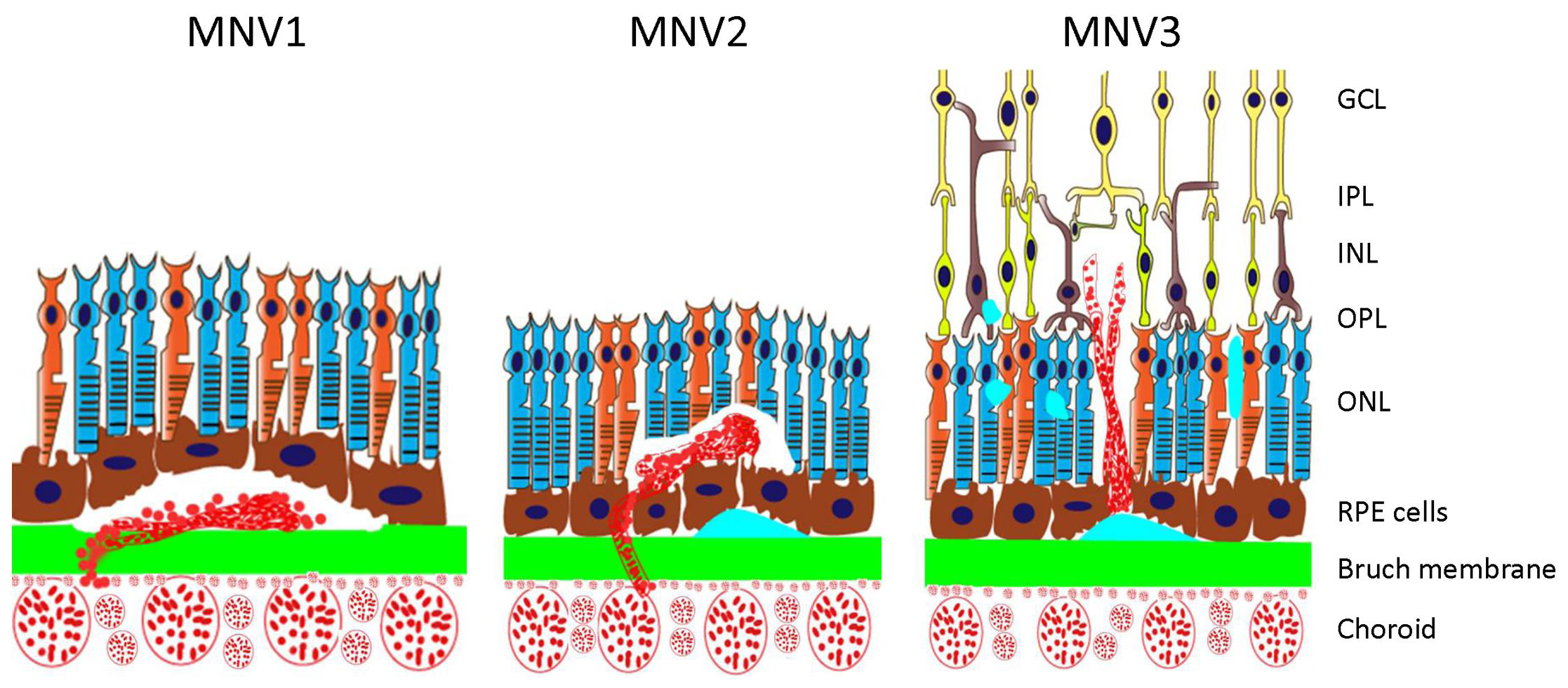
For review, MNV lesions are categorized as follows:
- type 1: sub-RPE “occult” choroidal neovascular membrane
- type 2: “classic” subretinal membrane above the RPE
- type 3: retinal angiomatous proliferation
A total of 1,606 nAMD eyes (1,330 patients) who received seven injections over 12 months were included.
Significant clinically relevant differences between MNV lesion types were found. Type 1 was the most prevalent neovascular lesion, accounting for nearly half of the study subjects (45.3%). This is in line with previous randomized clinical trials, which reported that occult lesions represented between 37.6% and 54.5% of their study cohorts and other real-world cohorts.
With regards to the visual outcomes, type 2 lesion patients had lower baseline and final VA at 12 months than the other MNV lesion types. “These lesions grow into the subretinal space, are frequently associated with exudation of subretinal hyperreflective material and ultimately lead to fibrotic changes that affect the integrity of the outer retinal layers, the ellipsoid layer and the RPE, leading to loss of vision,” the authors explained in their paper. “Similar results have been presented in a recent meta-analysis, which suggested that these lesions should undergo early intensive treatment to reduce the risk of progressive vision loss.”
Type 3 lesions had the highest baseline VA at diagnosis, the quickest time to lesion inactivation and the lowest percentage of active visits over 12 months. According to the authors, this suggests that these lesions are detected early and commonly respond well to anti-VEGF therapies, consistent with previous reports.
Such lesions “showed numerically the greatest VA gain, probably related to a relatively lower baseline VA compared to other lesion types, which is less constrained by the ‘ceiling’ than lesions with better VA, an effect that is frequently seen in nAMD studies that is associated with a greater potential for VA gain,” the authors wrote. This difference was not observed in other MNV lesion types, as other previous reports found before us.
A relevant finding of this study that the authors say deserves further investigation is the variation in the treatment choice observed in aneurysmal type 1 lesions, which were predominantly treated with aflibercept compared to other drugs. Several previous studies have suggested that these lesions respond better to aflibercept than to other drugs, “often in studies conducted in the Asia-Pacific region where this type of lesion is more prevalent,” the authors explained. “Our results suggest that the MNV lesion type could be used as a prognostic marker of visual gain.”
The authors suggest that the finding of this study may be applied in daily practice and can potentially support a personalized clinical decision making in these patients. “The baseline characteristics, visual outcomes, number of injections and visits reported in this study provide an accurate picture on how each type of NV membrane is managed in our setting nationwide and benchmark our results to other real-world international cohorts,” the authors concluded.
Izquierdo-Serra J, Martin-Pinardel R, Moll-Udina A, et al. Macular neovascularization type influence on anti-VEGF intravitreal therapy outcomes on age-related macular degeneration. Ophthalmology Retina. October 27, 2023. [Epub ahead of print.] |

