 A 13-year-old white male, accompanied by his parents, presented following a BB wound to his left eye two days earlier. The patient was accidentally shot through the lower eyelid while he and his friend were playing with a BB gun. He immediately went to the emergency room for evaluation. A computed tomography (CT) scan showed that the BB was located in the inferior orbit and was lodged against the eye wall.
A 13-year-old white male, accompanied by his parents, presented following a BB wound to his left eye two days earlier. The patient was accidentally shot through the lower eyelid while he and his friend were playing with a BB gun. He immediately went to the emergency room for evaluation. A computed tomography (CT) scan showed that the BB was located in the inferior orbit and was lodged against the eye wall.
The BB was surgically removed, and the lid was repaired. Two days later, the boy visited the eye hospital complaining of blurred vision in the traumatized eye.
Best-corrected visual acuity was 20/20 O.D. and 20/400 O.S. There was no significant refractive error in either eye. Confrontation fields were full to careful finger counting O.U. The pupils were both equally round and reactive, and there was a trace afferent pupillary defect in the left eye.
The anterior segment exam was normal in the right eye. Examination of the left eye showed significant swelling and ecchymosis of the lids and conjunctiva. The cornea was clear, and the anterior chamber was 3+ deep, without cell or flare. The iris was flat, without mass or rubeosis, and the lens was clear. Intraocular pressure measured 16mm Hg O.U.
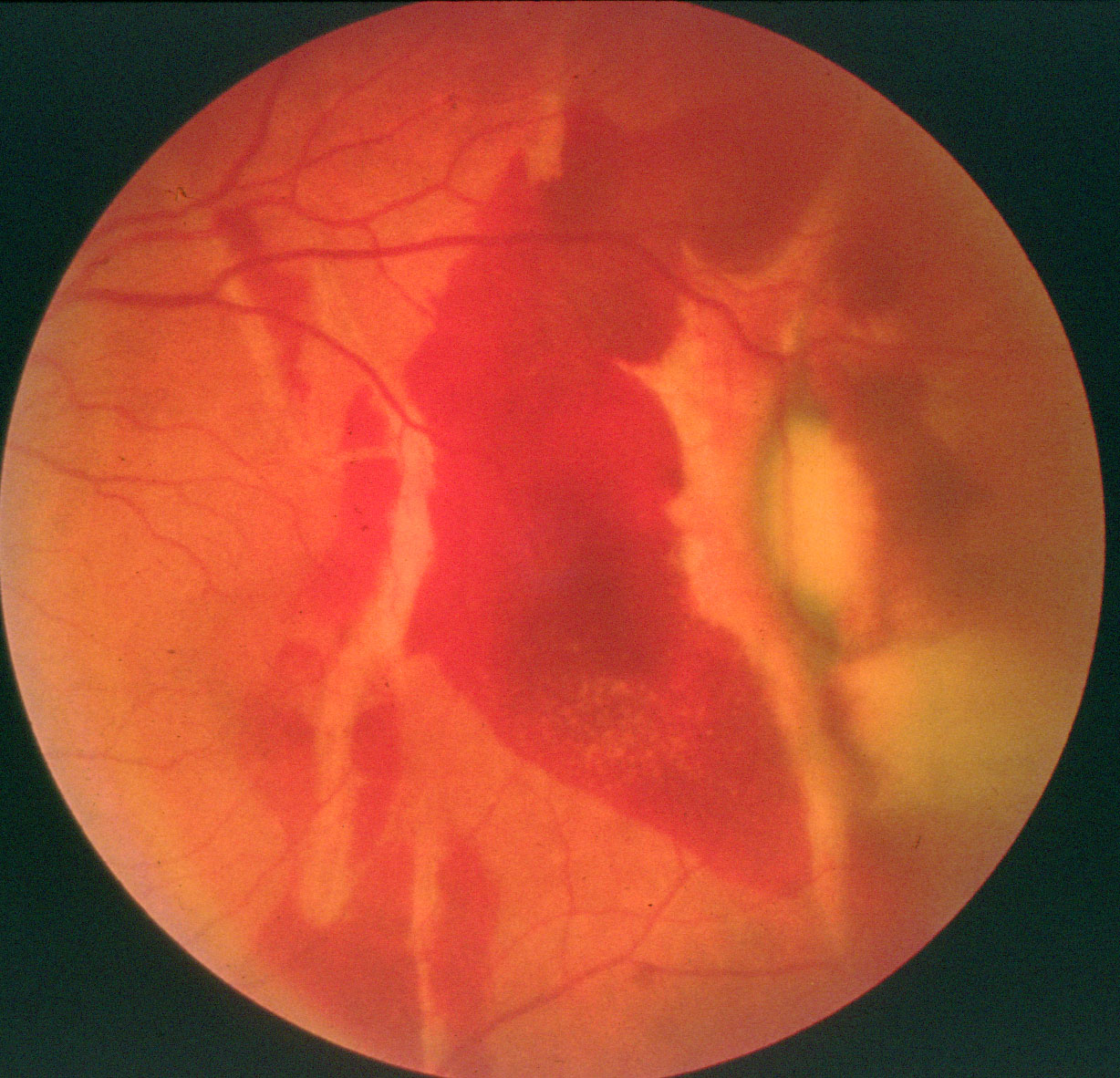
Dilated fundus exam of the right eye was completely normal. The left eye showed a small cup with good rim coloration and perfusion. The other changes are illustrated in figures 1 and 2.
2. A more peripheral view of the temporal retina. What does the oval white lesion represent?
Take the Retina Quiz
1. Which of the following conditions is responsible for the poor vision in the patients left eye?
a. Traumatic macular hole.
b. Choroidal rupture.
c.
d. Retinal detachment.
2. What is the lightly colored, linear lesion seen in the fundus photographs?
a. Open globe.
b. Lacquer cracks.
c. Choroidal rupture.
d. Nonspecific change in the retinal pigment epithelium (RPE).
3. What does the more peripheral view of the depigmented lesion indicate?
a. Open globe, perforating injury.
b. Commotio retinae.
c. Choroidal rupture.
d. Sclopetaria.
4. What is the appropriate treatment for this patient?
a. Observation.
b. Repair of the full-thickness macular hole.
c. Laser.
d. Enucleation.
For answers, see below.
Discussion
This patient suffered extensive retinal damage as a result of the BB injury to the left eye. Although the BB did not penetrate the globe, the eye sustained a significant contusion injury. This is most likely the result of the BB hitting the eye wall at such a high velocity.
He had extensive subretinal hemorrhage throughout the retina; this was denser superiorly. The patient developed a traumatic full-thickness macular hole, which accounts for the reduced visual acuity in his left eye.
He also sustained three choroidal ruptures. The largest rupture started superiorly, by the arcade, and extended inferiorly. Fortunately, it narrowly missed the center of the fovea. Two smaller ruptures can be seen, both superiorly and inferiorly, as light linear lines.
The changes described are a common result of severe ocular trauma. Traumatic macular holes were initially discovered in the late 1860s.1 It was once believed that all macular holes were the result of trauma; however, we now know that trauma accounts for merely 10% of all full-thickness macular holes.1 These injuries typically occur in younger patients.
At this juncture, the exact cause of macular holes remains unclear. Tractional forces from the vitreous seem to play a key role. However, experts disagree as to whether the traction is tangential, oblique or even anterior-posterior. Axial forces may also be possible. Hydration is another proposed explanation.
During trauma, it is believed that a breach develops in the internal retinal layers, which disrupts homeostasis. This, in turn, causes intraretinal swelling, and triggers the formation of a macular hole. In most cases, both the posterior hyaloid and the rigid internal limiting membrane remain intact.1,2
Choroidal ruptures result from mechanical compression of the globe followed by sudden hyperextension caused by blunt trauma. Bruchs membrane does not have enough elasticity to withstand the compressive force generated by blunt trauma, so it typically ruptures. These ruptures often are radial and occur temporal to the macula. There is a high propensity for choroidal neovascular membranes to grow through these breaks in Bruchs membrane.
The oval-shaped, depigmented lesion superior temporal is of particular interest. This represents a full-thickness break that affects the retina; RPE and choroid, but the sclera is not affected. This likely represents an area of sclopetaria. Sclopetaria results from a closed-globe injury, in which a missile-like object tangentially bumps, but does not penetrate, the eye wall. The contusion injury causes a rupture of the choroid, Bruchs membrane and retina, yet leaves the sclera intact.3 Severe scarring develops around the area where the rupture occurred.
In this patient, the subretinal hemorrhage will naturally resolve, and more scarring will develop in the area of the sclopetaria. Studies have shown that the risk for developing a retinal detachment in the area of the sclopetaria is relatively low.3
Vitrectomy to repair the macular hole is one treatment option. However, there are several reports of spontaneous closure of traumatic macular holes. One study showed that eight of 18 eyes with traumatic macular holes experienced spontaneous hole closure, yielding improved visual acuity.4
For now, we elected to carefully observe this patient. If the hole does not spontaneously close, we will seriously consider vitrectomy.
Retina Quiz Answers: 1) a; 2) c; 3) d; 4) a.
1. Smiddy WE, Flynn HW Jr. Pathogenesis of macular holes and therapeutic implications. Am J Ophthalmol 2004 Mar;137(3):525-37.
2. Oehrens AM, Stalmans P. Optical coherence tomographic documentation of the formation of a traumatic macular hole, Am J Ophthalmol 2006 Nov;142(5):866-9.
3. Dubovy SR, Guyton DL, Green WR. Clinicopathologic correlation of chorioretinitis sclopetaria, Retina 1997;17(6):510-20.
4. Recchia FM, Aaberg Jr T, Sternberg Jr P. Trauma: Principle and Technique of Treatment. In: Ryan SJ (ed.) Retina, Vol. IIIMedical Retina. 4th ed.

