 |
The June 2017 installment of this column, “Putting Pen to Paper,” included a cheiroscopic tracing to show size perception differences in how a patient with aniseikonia saw the world. Cheiroscopic tracings are not a routine part of optometric practice, but they come in handy as a problem-solver in some of the more difficult cases. In this month’s column, we will reacquaint you with the procedure and, more importantly, help you understand which types of cases it is best suited for.
 |
|
Fig. 1. The Wolff Standup Cheiroscope (Bernell). Click image to enlarge. |
The Process
A typical example of a stereoscope can be seen in Figure 1. The optics can vary, but most have +5.00 sphere lenses, which set the working distance at 20.00cm, simulating distance demand for accommodation. Additionally, they have base-out prism in front of each eye, allowing the two pictures to be separated in space, even though they appear to be overlapping to the viewer with little vergence demand. In one form or another, each also has a septum, which prevents the right eye from seeing the left target and the left eye from seeing the right target.
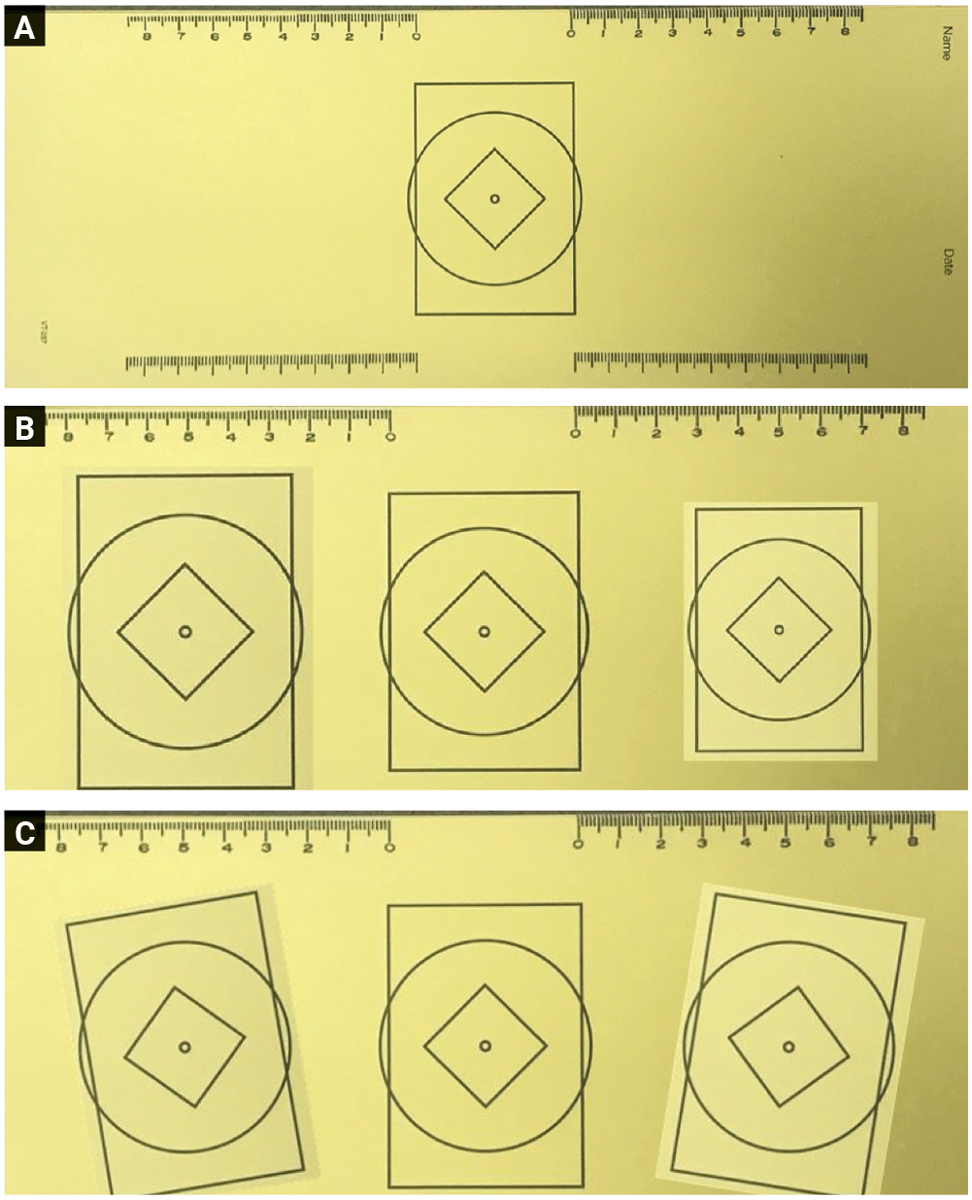
We now have the two channels isolated, but the sense is that they are unified. Figure 2 shows a patient completing a tracing. The standard paper used is 11.50in wide by 4.25in tall with the reference figure printed in the center (Figure 3a).
When performing the test, first the printed target is placed before one eye in the stereoscope. Then, the patient is given a pencil and asked to trace the figure. When the figure is in front of the left eye, the right hand performs the tracing, and vice versa. This gives us two ways to see the variations between the spatial percepts as formed through each eye. This helps with size differences (aniseikonia), cyclodeviations (where one eye relative to the other sees an altered scene) and vertical deviations (where one tracing is above the reference picture and the other is below).
There is a misconception that aniseikonia is nearly always present when different refractive powers exist between the right and left eyes. However, this is not always the case. We have seen cases with large differences in refraction between the right and left eyes with no size perception differences and cases where it is present.
We have also seen our fair share of cases with nearly equal refractive powers on each side, in which a clinically significant size perception difference existed. Without testing for it, we would be searching in the dark for something that is rather easy to identify and if present, is rather easy to prescribe for. As the late Robert A. Kraskin, OD, used to say, “It’s not what a lens does to a person, but what a person does with a lens” that really matters.
 |
|
Fig. 2. A modified Brewster Stereoscope (Keystone). This version is affixed to the wall and can be adjusted to meet the needs of most people. Click image to enlarge. |
More Than Meets the Eye
Figure 3b shows a size perception difference between a pair of eyes of about 10%. When the reference figure is in front of the right eye, the left hand traces a larger figure than is referenced. While tracing, the point of the pencil looks like it follows the outline of the reference figure, and when done, the two figures look as if they are one solid figure—both appearing to be the same size. The spatial transformation is the result of optics plus perception and is not secondary to only the optics.
When the reference figure is in front of the left eye, the right hand traces a smaller figure by the same amount on the right side of the paper, which, again, appears to be the same size as the target. It is important to have both representations to compare the size differences between the two figures. The more similar the size transformations are, the higher the likelihood those measures are clinically significant.
Figure 3c shows a similar set of tracings where no size difference is present but the perception of what is vertical and horizontal is clearly off with respect to how the world is viewed through each eye. In this instance, we can see 10° of outward cyclorotation. We always label the direction of the rotation relative to the top and whether it is shifted inwards toward the nose or outwards toward the ear.
 |
|
Fig. 3. On top (A) is the blank form used to perform the tracings. The middle image (B) shows a roughly 10% size difference. Note that each side must show a similar amount of size difference, but in the opposite direction. On the bottom (C) is a clinically significant cyclorotation. Click image to enlarge. |
The Case
An older male patient was referred due to sudden-onset diplopia. In a person aged 65+, this is always a red flag. His history included acute sinus infections, which required medical treatment but no surgery.
Cover testing in primary gaze at distance revealed a 10 prism-diopter exophoria with a 2 prism-diopter vertical deviation. At near, the amount of exo increased, but the patient did not show a tropia until we did some eye movements.
When looking in any direction 20° to 25° away from straight ahead, he saw double vision with a horizontal and vertical component. However, he also mentioned that every time his vision doubled, one image was twisted, or, as he said, “vertical wasn’t vertical in one of the images.”
We performed a double Maddox rod test and measured 10° of cyclodeviation in primary gaze. This same cyclo was seen on a cheiroscopic tracing, similar to Figure 3c.
Because the patient was not seeing double in primary gaze and showed normal global stereo acuity and no other signs of eye, vision or systemic health issues, we decided to take no further action and simply see him four to six weeks later. We expected him to continue recovering and explained our hypothesis that the episode of double vision was secondary to his sinus issues, which may have interfered with innervation to the extraocular motor system.
At the follow-up visit, the cyclo was fully resolved, though the patient still showed a mild exophoria at both distance and near. The slight vertical deviation had also resolved. He was able to move his eyes out to 50° in all directions at distance and near without diplopia interfering or any break in fusion occurring. A repeat of the cheiroscopic tracing showed equal-sized images and no evidence of the prior cyclorotation.
Imaging was not ordered because it seemed like he was already well along on the road to recovery by the time we saw him.
Takeaways
There are times when our standard chair and analytic tests don’t give us the whole picture. Adding some insights from our optometric heritage, which in this case included cheiroscopic tracing and the double Maddox rod for confirmation, helped us understand how best to approach the care of our patient. Having these adjunct tests available when needed can save chair time as well as reduce patient anxiety, which might be triggered by additional testing.
Dr. Taub is a professor, chief of the Vision Therapy and Rehabilitation service and co-supervisor of the Vision Therapy and Pediatrics residency at Southern College of Optometry (SCO) in Memphis. He specializes in vision therapy, pediatrics and brain injury. Dr. Harris is also a professor at SCO. Previously, he was in private practice in Baltimore for 30 years. His interests are in behavioral vision care, vision therapy, pediatrics, brain injury and electrodiagnostics. They have no financial interests to disclose.

