 |
A 74-year-old Hispanic male was referred for evaluation of a “black spot” OS. He denied any pain, redness, photophobia, photopsias or floaters. His medical history included diabetes mellitus, arthritis, kidney disease and heart arrhythmias, all of which were being treated medically. His ocular history included bilateral cataract surgery.
Entering VA was 20/40 OD and 20/60 OS with no pinhole improvement. IOPs were 12mm Hg OU. Pupils were equally round and reactive without a relative afferent pupillary defect, and confrontation visual fields were full OU. Anterior segment exam showed pseudophakia OU with mild posterior capsular opacification OD and an open posterior capsule OS; there was no evidence of anterior segment neovascularization.
Take the Retina Quiz
1. Which of the following is false regarding Figures 1 and 2?
a. B-scan shows a hyperechoic and mildly elevated optic nerve head lesion.
b. B-scan shows low internal reflectivity.
c. OCT shows superficial hyperreflective opacities within the optic nerve head.
d. There is a darkly and evenly pigmented lesion partially obscuring the optic nerve.
2. What is the most likely diagnosis for the pigmented lesion of the left eye?
a. Choroidal nevus.
b. Juxtapapillary choroidal melanoma.
c. Optic nerve melanocytoma.
d. Primary optic nerve melanoma.
3. How would you describe the B-scan (Figure 2)?
a. Hyperechoic, mildly elevated optic nerve head lesion with high internal reflectivity.
b. Hypoechoic, mildly elevated optic nerve head lesion with high internal reflectivity.
c. Hyperechoic, mildly elevated optic nerve head lesion with low internal reflectivity.
d. Hypoechoic, mildly elevated optic nerve head lesion with low internal reflectivity.
4. What is the general prognosis for this condition?
a. Excellent, no potential for malignant transformation.
b. Good, however 1% to 2% chance for malignant transformation.
c. Guarded, 50% chance for malignant transformation.
d. Poor, malignant lesion with high risk of metastasis.
5. What is the appropriate management?
a. Urgent referral for fine needle aspiration biopsy of lesion.
b. Genetic testing to rule out an inherited retinal dystrophy.
c. Observation with annual fundus exams and serial fundus photography.
d. All of the above are necessary.
 |
Fig. 1. Optos fundus photograph of the left eye. Click image to enlarge. |
Diagnosis
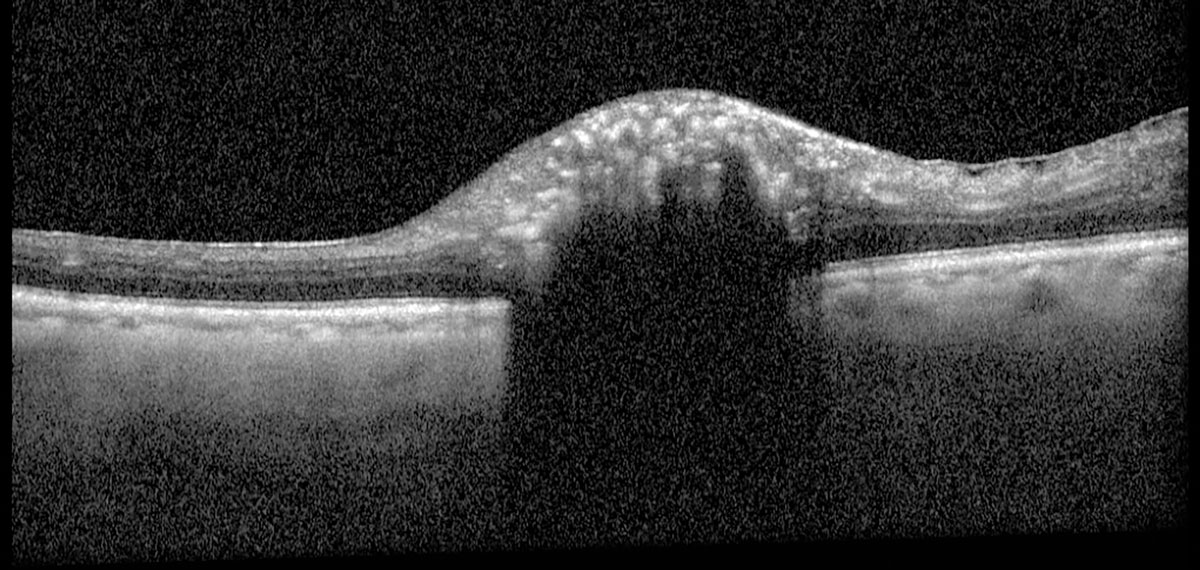
Fundus exam revealed a posterior vitreous detachment OU, diabetic retinopathy OU and a hyperpigmented melanocytic lesion contiguous with the inferior optic nerve head OS (Figure 1). B-scan ultrasound showed this was an elevated, hyperechoic lesion of the optic nerve head OS that was measured to have an apical thickness of 1.05mm and greatest basal diameter of 2.85mm (Figure 2). OCT through the lesion showed a shallow dome-shaped mass with superficial hyperreflective opacities and underlying shadowing with temporal epiretinal membrane (Figure 3). A clinical diagnosis of optic nerve melanocytoma was based on these findings.
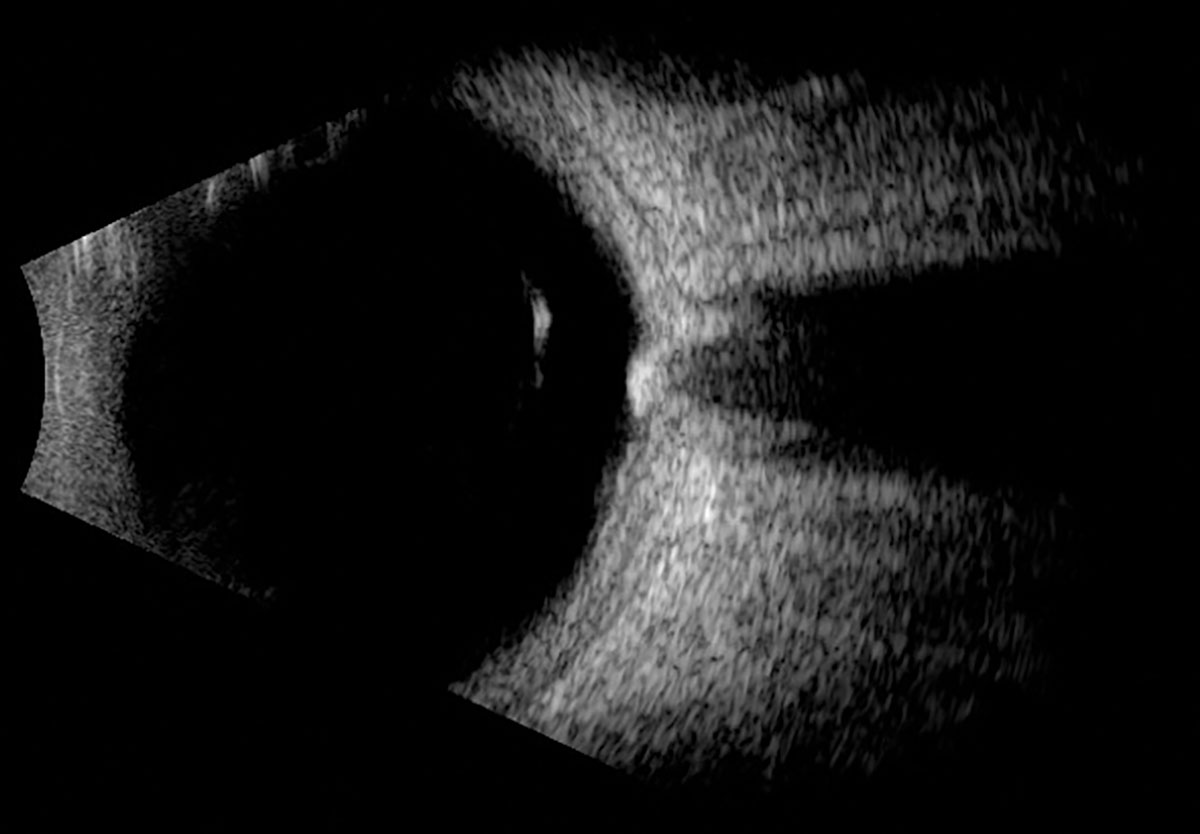 |
Fig. 2. Horizontal axial B-scan of the left globe. Click image to enlarge. |
Optic nerve melanocytoma is a benign neoplasm of the optic nerve head that was first described in 1933.1 The term melanocytoma was later coined in 1965 based upon histopathologic similarities to the melanocytic lesions found in ocular melanocytosis.1 Melanocytoma is actually a broad term to describe any lesion comprised of melanocytes; a more accurate descriptor would have been hyperpigmented magnocellular nevus of the optic disc, though this never gained enough traction to supplant the simpler term melanocytoma.1
Melanocytomas appear to have a slight female predilection (63%) with no clear racial predilection and average age of 50 years at time of initial diagnosis.1,2 Exact pathophysiology is unknown, and it was once thought to be a congenital lesion; however, it is interesting to note that melanocytomas are rarely seen in children and there are numerous reports of acquired lesions in patients with documented fundus photography before and after the occurrence.1 This has led to speculation that melanocytomas may initially arise as amelanotic lesions that later acquire pigment, though further studies are needed to better understand this process.1,2
The differential diagnosis for melanocytoma includes choroidal nevus, juxtapapillary uveal melanoma, hyperplastic retinal pigment epithelium (RPE), combined hamartoma of the retina and RPE and, more rarely, primary optic nerve melanoma or metastatic melanoma to the optic nerve.1,3 Melanocytoma is a largely clinical diagnosis based on the characteristic presentation of a unilateral intensely pigmented lesion involving all or part of the optic nerve head.1 Furthermore, lesions may be isolated to the optic nerve head or extend into the adjacent choroid or neurosensory retina.1 That being said, melanocytomas can be indistinguishable from melanoma in certain clinical contexts and a high clinical suspicion must be maintained.1,3,4
Ancillary testing such as fundus photography can be useful to monitor evolution of the lesion over time.1,3 Ultrasonography is of little diagnostic value, but notably depicts mildly elevated (28%) or dome-shaped (62%) lesions with medium-high internal reflectivity (85%) and are largely avascular (89%).3 These features are contrasted with melanomas, which often depict lower echogenicity and greater vascularity.3,5 Fluorescein angiography can delineate tumor borders (hypofluorescence) when difficult to discern clinically.1,5 While there are no pathognomonic features of melanocytoma on OCT, the lesions tend to have a hyperreflective superficial border, superficial hyperreflective opacities and dense shadowing.1,5,6 Despite its limitations, OCT can still be a useful tool to monitor for exudation and peripapillary extension.1, 5-7
 |
|
Fig. 3. Heidelberg Spectralis OCT of the left optic nerve head. Click image to enlarge. |
Prognosis
Fortunately, the prognosis is generally excellent, as many (93%) retain undisturbed VA of better than 20/40 with low risk of malignant transformation.1,4 Furthermore, the presence of a relative afferent pupillary defect has been seen in 7% to 30% of patients and seems to be associated with VA worse than 20/50.1,8 The majority of patients have some degree of visual field deficit, most commonly manifesting as enlargement of the blind spot.1,2
Despite the benign nature of these presentations, serial fundus photography has shown subtle enlargement in 10% to 15% of melanocytomas when observed over the course of years.1,5,8 In a review of 116 eyes, tumor enlargement was demonstrated in 11% to 14% of patients at five years, 32% at 10 years and 38% at 20 years; an initial thickness of >1.5mm at diagnosis is a predictive risk factor for growth.1,2,8 Although growth often represents the benign natural history of the lesion, it can alternatively represent tumor necrosis, which may produce a secondary optic neuropathy with severe vision loss.1
In conclusion, optic nerve melanocytomas are benign lesions that typically have no visual consequences. Occasionally, these lesions exhibit growth, produce retinal vein occlusions and rarely can progress to malignancy. Therefore, careful monitoring with annual fundus exam and serial photography are indicated monitor for transformation.
Retina Quiz Answers
1: b, 2: c, 3: a, 4: b, 5: c
Dr. Aboumourad currently practices at Bascom Palmer Eye Institute in Miami. He has no financial disclosures.
Dr. Campbell graduated from the University of Houston College of Optometry and is completing an ocular disease residency at Bascom Palmer Eye Institute.
1. Shields JA, Demirci H, Mashayekhi A, et al. Melanocytoma of the optic disc: a review. Indian J Ophthalmol. 2019;67(12):1949-58. 2. Shields JA, Demirci H, Mashayekhi A, Shields CL. Melanocytoma of optic disc in 115 cases: the 2004 Samuel Johnson Memorial Lecture, part 1. Ophthalmology. 2004;111(9):1739-46. 3. Gologorsky D, Schefler AC, Ehlies FJ, et al. Clinical imaging and high-resolution ultrasonography in melanocytoma management. Clin Ophthalmol. 2010;4:855-9. 4. Mohmad Z, Kah TA, Yong KC, et al. Melanocytoma of the optic nerve head - a diagnostic dilemma. Clin Pract. 2011;1(3):e60. 5. Zhang P, Hui YN, Xu WQ, et al. Infrared autofluorescence, short-wave autofluorescence and spectral-domain OCT of optic disk melanocytomas. Int J Ophthalmol. 2016;9(5):713-6. 6. Raval V, Reddy R, Kaliki S, et al. Optic nerve head melanocytoma: Optical coherence tomography/angiography features. Indian J Ophthalmol. 2021;69(2):332-6. 7. Lee E, Sanjay S. Optic disc melanocytoma report of five patients from Singapore with a review of the literature. Asia Pac J Ophthalmol (Phila). 2015;4(5):273-8. 8. Lee CS, Bae JH, Jeon IH, et al. Melanocytoma of the optic disc in the Korean population. Retina. 2010;30(10):1714-20. |

