 |
Q:
A 68-year-old retinitis pigmentosa patient was seen for the one week post-op visit following cataract surgery in the right eye. Visual acuity was unaided 20/20, but he stated that something was wrong with his vision in that eye. I dilated the patient and observed a large superior detachment that, in the course of the next hour, dropped the vision to 20/80 and then hand motion by the time I got him to the retinal specialist two hours later. What is the risk of RD after surgery, and did the RP predispose him to it?
A:
“It has been well established that rhegmatogenous retinal detachment (RD) is a potential complication following phacoemulsification,” says Mohammad Rafieetary, OD, of Charles Retina Institute in Germantown, TN.1-3 Although advances in cataract surgery have reduced the relative risk, “by one estimate the risk still looms at 1% compared with a 0.005% risk of retinal detachment in normal eyes,” he says.4 In RP patients, Dr. Rafieetary explains, no evidence currently supports that they are at higher risk for RD following cataract surgery.
“The relative risk for retinal detachment after cataract surgery is higher for younger patients, males and those with long axial lengths.2 But, within the context of the RP patient, the risk of post-op complications doesn’t differ from the general population,” Dr. Rafieetary says.5 He notes that macular edema (Figure 1) is a complication of RP, so pay special attention pre- and post-op and start patients on prophylactic NSAID drops.5
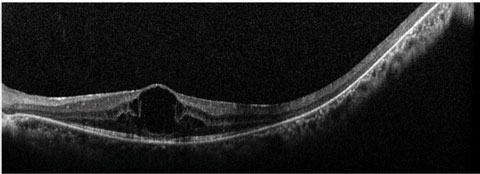 |
| Fig. 1. Macular edema, seen here on OCT, is a complication of RP. |
When managing patients with cataract, Dr. Rafieetary explains that the AOA recommends careful dilated retinal examination. “Due to the limitations of imaging devices, including widefield imaging, eye care providers should not substitute fundus photography with a dilated exam of the retina,” Dr. Rafieetary suggests.
However, outside of one’s standard postoperative protocols, sometimes OCT and visual fields (VF) are imperative, he says. “When unusual subjective symptoms are not explained by changes in the anterior segment, a dilated fundus exam and ancillary imaging such as OCT and automated VF must be used to properly diagnose the etiology,” he says.
Is There Anything New in RP Research?
“RP is an inherited disorder with over 100 genes implicated with its etiology and multiple subtypes,” says Dr. Rafieetary. “This can explain the complexities and challenges associated with finding a single effective treatment.”6
Dr. Rafieetary explains that you can easily follow the progress of RP research online. “The most comprehensive resource to follow the majority of RP clinical and scientific trials is clinicaltrials.gov, which has 117 RP studies listed on the site, in various stages.
Hope on the Horizon
While treatments for RP remain limited, the most promising therapies lie in the realm of regenerative medicine, explains Dr. Rafieetary. “Induced pluripotent stem cells are one of the most promising treatment modalities for RP and other retinal degenerative diseases, such as Leber’s congenital amaurosis and Best vitelliform macular dystrophy. These cells can be generated directly from adult cells.”7-9
The last decade has been a promising era for many posterior segment diseases that previously resulted in devastating visual outcomes, Dr. Rafieetary says, but even greater success could be on the horizon. “Over the next decade, we look forward to new advances for treatment of patients suffering from blinding retinal vascular and degenerative diseases such as RP, diabetic retinopathy and AMD.”
|
1. Olsen T, Jeppeen P. The incidence of retinal detachment after cataract surgery. Open Ophthalmol J. 2012;6:79-82. 2. Clark A, Morlet N, Ng J, et al. Risk for retinal detachment after phacoemulsification: a whole-population study of cataract surgery outcomes. Arch Opththalmol. 2012;130(7):882-8. 3. Erie JC, Raecker ME, Baratz KH, et al. Risk of retinal detachment after cataract extraction: 1980-2004: A population-based study. Trans Am Ophthalmol Soc. 2006 Dec;104:167-75. 4. Ivanisevi M, Boji L, Eterovi D. Epidemiological study of nontraumatic phakic rhegmatogenous retinal detachment. Ophthalmic Res. 2000 Sep-Oct;32(5):237-9. 5. Jackson H, Garway-Heath D, Rosen P. Outcome of cataract surgery in patients with retinitis pigmentosa. Br J Ophthalmol. 2001 Aug;85(8):936-8. 6. Hartong DT, Berson EL, Thaddeus PD. Retinitis pigmentosa. The Lancet. 2006;368(9549):1795-1809. 7. Yvon C, Ramsden CM, Lane A, et al. Using stem cells to model disease of the outer retina. Comput Struct Biotechnol J. 2015;13:382-9. 8. Tucker BA, Mullins RF, Streb LM, et. al. Patient-specific iPSC-derived photoreceptors precursor cells as means to investigate retinitis pigmentosa. eLife. 2013;2:e00824. 9. Yang J, Cai B, Glencer P. Induced pluripotent stem cells and outer retinal disease. Stem Cell Internat. 2016;2016. 2850873. |

