 |  |
Most of us likely have at least one patient on a daily basis complain about floaters, such as black spots, bugs, spider webs and strings. These are frustrating symptoms that can be detrimental to a patient’s quality of life. The last thing they want to hear is, “Your brain will get used to them.”
Through the years, there has been more emphasis on treatment for this nuisance. While vitrectomy and vitreolysis are commonly used, there is another treatment available known as 1-Step limited vitreous removal (Vista Ophthalmics).
Candidates
At this time, 1-Step is only approved in patients that are pseudophakic. While it is possible to perform in those with retinal pathology, it is best to avoid in patients with lattice degeneration, a history of retinal breaks, tears or holes or with an epiretinal membrane. Patients should be symptomatic for at least four months. Those with a new-onset posterior vitreous detachment should wait at least four to six months to prevent further traction on the retina. Make sure to perform a dilated eye exam to rule out any pathology.
Procedure
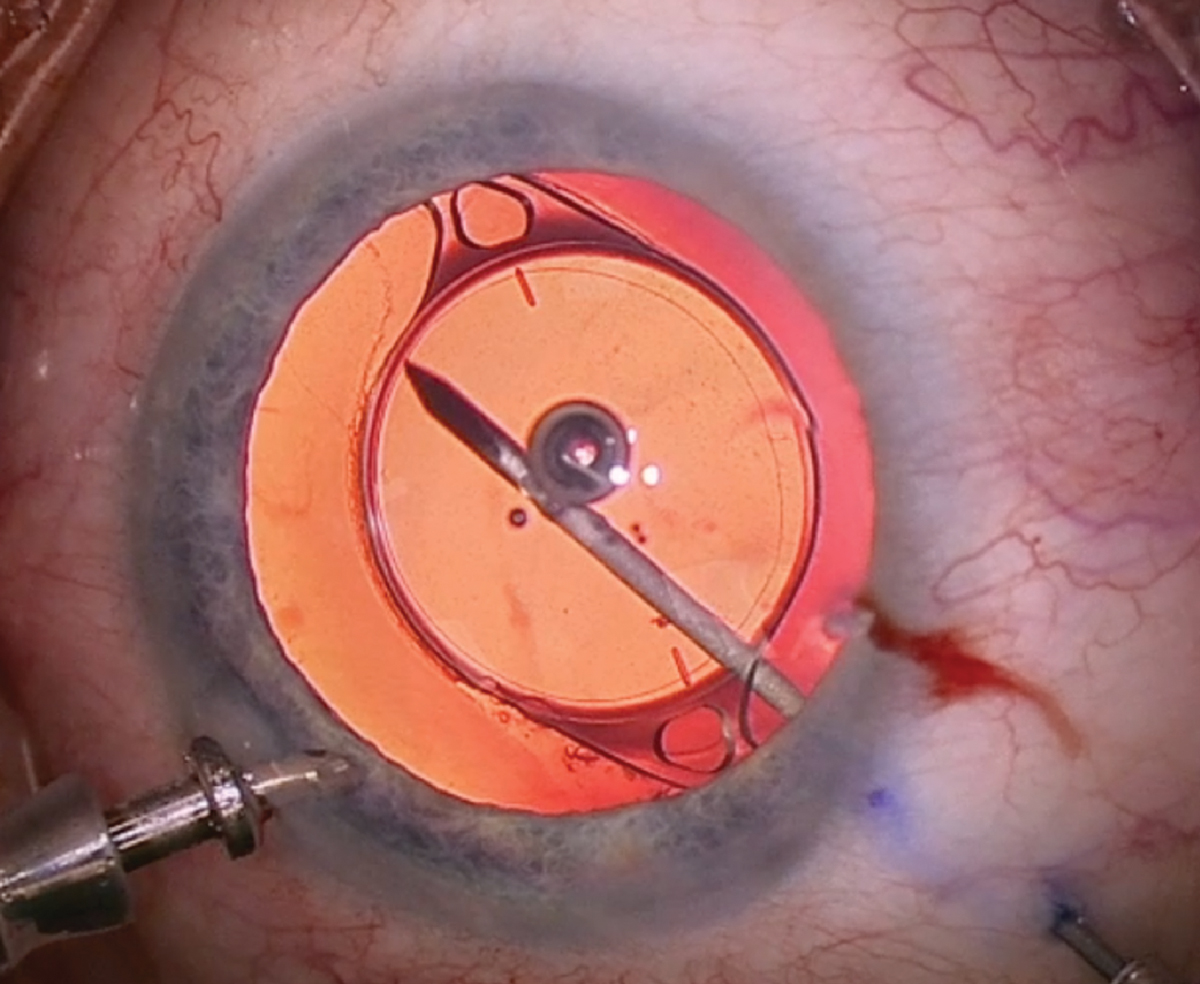
1-Step can be performed in an office-based surgical suite with oral anesthesia and topical lidocaine. A single-use 27-gauge needle vitrector is used. With a typical vitrectomy, there is a three-port system. The vitrectomy probe is intended to remove the vitreous and dissect the tissue by vitreous aspiration and cutting.
Silk 6-0 sutures are placed to help keep the eye stable, in primary position and provide counter traction. A 1mm paracentesis is made through the clear cornea and preservative-free lidocaine is instilled into the anterior chamber. Then, the anterior chamber maintainer is inserted through the paracentesis wound. About 3.5mm from the limbus in the superior or inferior temporal region, the 1-step vitrector is inserted into the vitreous cavity in perpendicular fashion to the globe. The irrigation is set to about 60mm Hg to keep the globe formed. The liquified vitreous opacities come to the tip of the vitrector using low (100mm Hg or less) vacuum. The cut rate is defined by the phaco machine, typically ranging from 5,000 to 15,000 cuts per minute. The vitrector is kept in the middle of the anterior vitreous, and due to the length, it cannot reach the other side or posterior pole.
After a few minutes, once the view is clear, the irrigation is decreased and the 1-step vitrector is removed. The surgeon then checks for a leak, removes the anterior chamber maintainer and hydrates all wounds. Lastly, a subconjunctival injection of gentamicin and dexamethasone is completed.
 |
|
1-Step limited vitreous removal allows surgeons to remove a significant portion of the vitreous without viscoelastic or sutures. Click image to enlarge. |
Post-operation
Patients are seen on the same day, one day, one week and one month post-op, and are on a combination drop of an antibiotic and steroid for one month. At each of these visits, visual acuity, IOP, aberrometry, dilated fundus exam and fundus photos are performed. Eyes are usually quiet but may experience a temporary IOP spike and can be treated with topical and/or oral ocular hypertensive medications.
Many who underwent 1-Step limited vitreous removal previously underwent vitreolysis treatments. While the risk is very low with 1-Step, as the vitreous being removed is primarily anterior and low vacuum, there is the chance of retinal breaks, holes and/or detachments.
A majority of our patients reported their floater symptoms have resolved and described the experience as life-changing. Seeing such incredible improvement reminds us how important it is to educate patients about all of the floater treatments available.
Dr. Banas practices at The Eye Centers of Racine and Kenosha in Kenosha, WI. He is a key opinion leader for Alcon, Ziess and New World Medical. Dr. Schiffbauer practices at The Eye Centers of Racine and Kenosha in Kenosha, WI.
Dr. Cunningham is the director of optometry at Dell Laser Consultants in Austin, TX. He has no financial interests to disclose. Dr. Whitley is the director of professional relations and residency program supervisor at Virginia Eye Consultants in Norfolk, VA. He is a consultant for Alcon.
1. Liu R, Rong B, Tu P, et al. Analysis of cytokine levels in tears and clinical correlations after intense pulsed light treating meibomian gland dysfunction. Am J Ophthalmol. 2017;183:81-90. 2. Jiang P, Liu Y, Zhang J, et al. Mast cell stabilization: new mechanism underlying the therapeutic effect of intense pulsed light on rosacea. Inflamm Res. 2023;72(1):75-88. |

