 |
Q:
A patient presents for a second opinion after being diagnosed with episcleritis three weeks ago and unresponsive to topical steroids. What are some other differentials to think about?
A:
“Despite being the first diagnosis, is episcleritis the correct diagnosis?” asks Mahsa Masoudi, OD, an ocular disease resident at Omni Eye Services of Atlanta. When faced with the presentation of sectoral bulbar conjunctival injection, most clinicians rush to judgment with a diagnosis of episcleritis.
 |
|
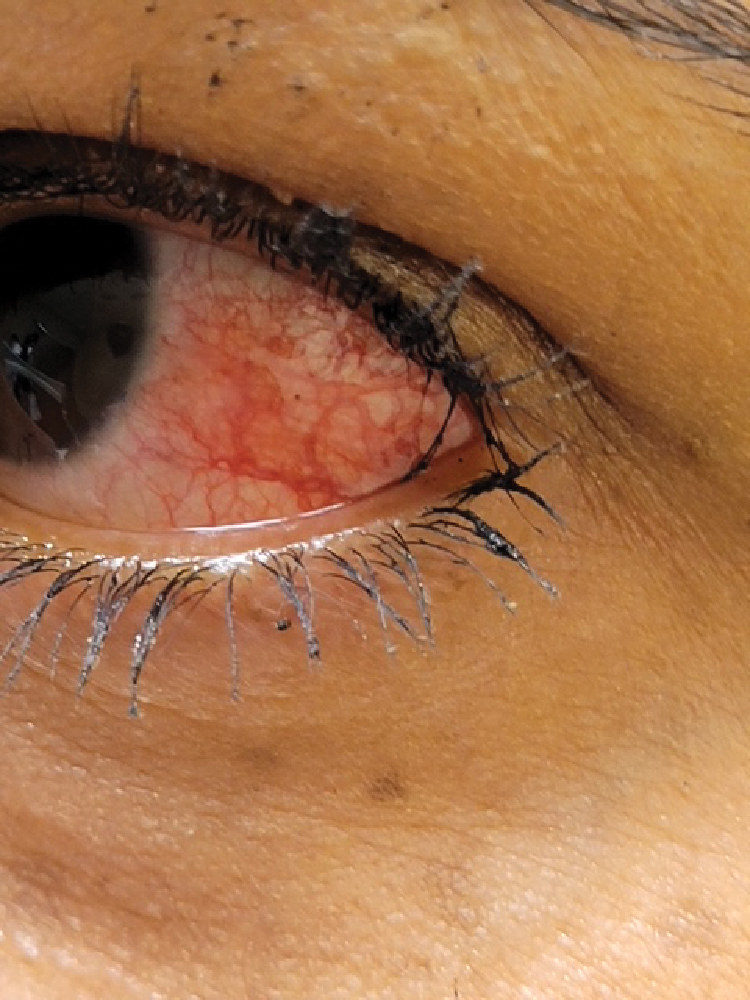
Don’t jump to conclusions when faced with sectoral injection. Click image to enlarge. |
Explore Your Options
Take a moment, rather, and consider other possibilities. Lids and lashes can be causative offenders when considering secondary sectoral redness due to possible ingrown lashes, floppy eyelid syndrome, canaliculitis or Staph-related toxicity or hypersensitivity.1 Marginal corneal ulcers and infiltrates erupt in smaller patches of sectoral injection proximal to the cornea as well.
Beyond episcleritis, other conjunctival differentials a clinician must consider include pingueculitis, inflamed pterygium, phlyctenulosis, subconjunctival hemorrhage and conjunctival abrasion.2 Also keep in mind obvious and occult foreign bodies and trauma. Always start with a good case history to rule out several of these differentials. History includes not only a patient’s ocular and medical status but their social and hygiene habits as well.
“Sometimes you have to dig for information and repeat your questioning in different ways,” Dr. Masoudi says. “A patient we saw recently adamantly denied trauma, but, on repeat questioning, ‘remembered’ that a branch whacked him in the eye while doing yardwork a day earlier, she says. Dr. Masoudi advises that following a comprehensive case history, a thorough slit lamp exam and fluorescein will often tell you the rest.”
In this case, the patient’s long, mascara-coated lashes pointed straight to the answer with fluorescein lighting up the conjunctival runaway. Repetitive mechanical trauma from her lashes alone led to a significant temporal conjunctival abrasion.
A little fluorescein goes a long way. If you think about a conjunctival abrasion first and confirm it with fluorescein staining, then you can go right to an antibiotic rather than using a steroid that will only delay proper healing.
Removing the offending agent, followed by treatment with a topical antibiotic four times a day for one week, helped totally resolve the issue. Epilating the particular misdirected lashes and educating our patient on the effects of less eye makeup and more lid hygiene will hopefully help prevent this from happening again.
Bottom Line
When you see sectoral injection, think conjunctival abrasion until proven otherwise! Once you rule that out, hone in on the other differentials, including episcleritis. Mild cases can resolve on their own or may require a steroid. More advanced simple or nodular episcleritis cases may be accompanied by pain and a systemic history, so think about a workup, especially if episodes are recurrent.
Lab testing should include antinuclear antibody (ANA), rheumatoid factor (RF), erythrocyte sedimentation rate (ESR), fluorescent treponemal antibody absorption (FTA-ABS), microhemagglutination-Treponema pallidum (MHA-TP), rapid plasma reagin (RPR), serum uric acid and a chest X-ray.4 Consider more aggressive topical therapy along with oral NSAIDs as you comanage these cases with rheumatology.
In the end, Dr. Masoudi reminds us, “though episcleritis is not rare, it certainly is not very common either, so first consider conjunctival abrasion when confronted with sector injection.”
Dr. Ajamian is the center director of Omni Eye Services of Atlanta. He currently serves as general chairman of the education committee for SECO International and is vice president of the Georgia State Board of Optometry. He has no financial interests to disclose.
1. Townsend W. Contact Lens Spectrum. 2014;29(11):9. 2. Bagheri N, Wajda B, Calvo C, Durrani A. The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease. 8th ed. Philadelphia: Wolters Kluwer; 2016. 3. Bowling B. Kanski’s Clinical Ophthalmology. 8th ed. WB Saunders; 2015. 4. Schonberg S, Stokkermans TJ. Episcleritis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. www.ncbi.nlm.nih.gov/books/NBK534796. Updated August 25, 2021. Accessed February 10, 2022. |

