 |
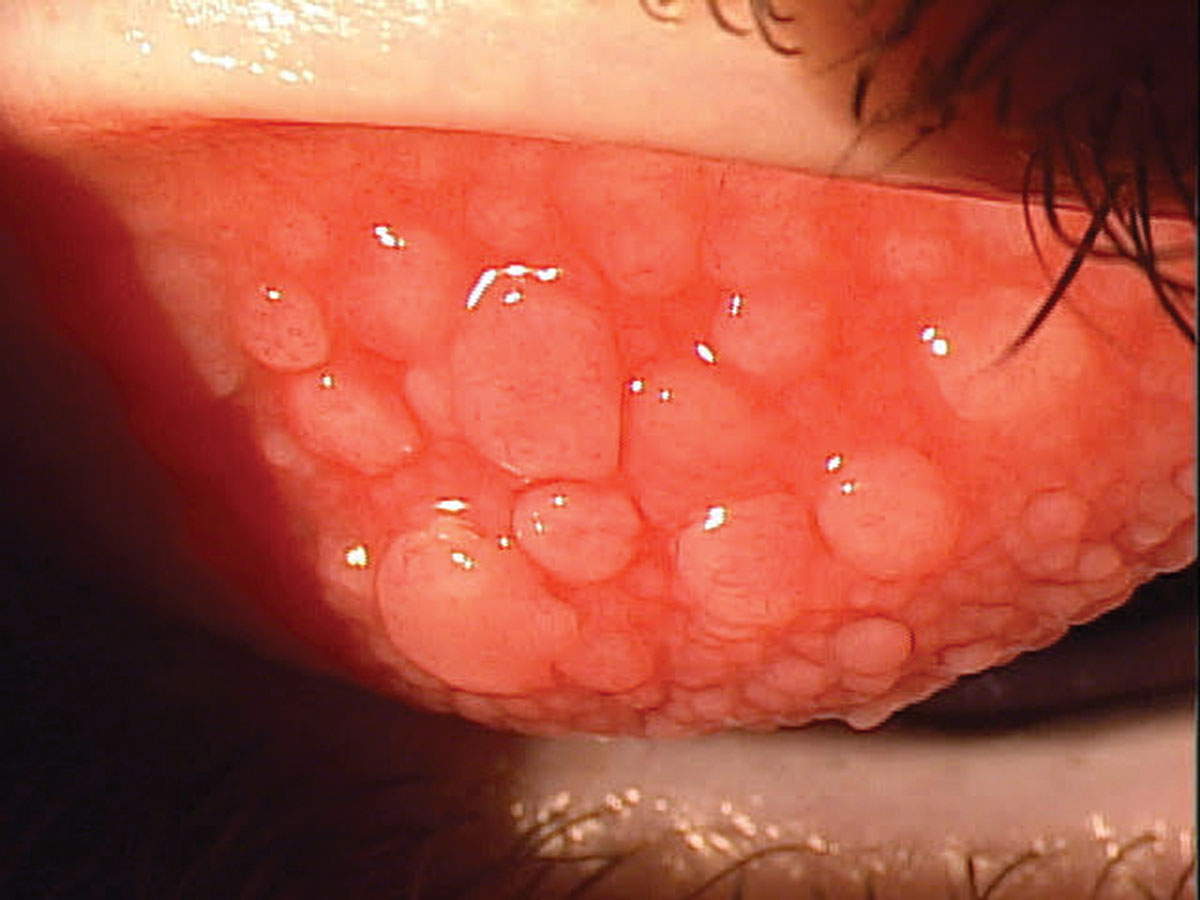
| This study found tacrolimus to be an effective therapeutic to treat patients with VKC and AKC. Photo: Paul M. Karpecki, OD. Click to enlarge. |
The effects of the prolonged use of tacrolimus ophthalmic suspension for the treatment of vernal (VKC) and atopic keratoconjunctivitis (AKC) are not fully understood. Looking to bridge this gap, researchers in Japan recently conducted a retrospective study to clarify the clinical improvement and safety associated with the use of tacrolimus ophthalmic suspension 0.1% over a 24-month follow-up period in patients with VKC and AKC. They found that it was an effective method for inducing and maintaining stability in VKC and AKC.
The study had three important findings:
Continuous therapy with tacrolimus ophthalmic suspension showed that the clinical scores recorded in the 24th month were significantly improved compared with those recorded in the sixth month.
Increased age was significantly associated with a decreased requirement for steroid eye drops on logistic regression analysis.
Cluster analysis showed that, based on background characteristics, patients could be divided into three clusters: adolescent, pediatric and adult.
The retrospective study included 36 eyes of 36 patients who had VKC and AKC and were treated with topical tacrolimus ophthalmic suspension 0.1% for 24 months. The researchers assessed clinical scores, remission rates, number of relapses and concomitant use of steroids and refractory indices. Clinical outcomes were determined using papillae-limbus-cornea scores and 5-5-5 exacerbation grading scale scores. Clinical characteristics associated with the need for concomitant steroid eye drop administration were determined using logistic regression analysis.
Papillae-limbus-cornea scores recorded at six months were significantly improved compared with those recorded at baseline. The scores recorded at 18, 21 and 24 months were significantly improved compared with those recorded at six months. Remission rates increased diachronically and significantly, reaching 92% in the 24th month. Logistic regression analysis showed that, for every 10-year increase in patient age, the risk for requiring concomitant administration of steroid eye drops was reduced by half (odds ratio, 0.53).
A cluster analysis divided the patients into three clusters depending on characteristics. The adolescent subgroup included those who used tacrolimus ophthalmic suspension 0.1% alone and did not have relapses or use steroids concomitantly. The pediatric subgroup included those who occasionally developed acute exacerbation and required concomitant use of steroids. The adult subgroup consisted mostly of patients with AKC who had persistent mild inflammation with a moderate refractory index and did not have relapses or use steroids.
“These results indicate that the severity of VKC and AKC may vary depending on the age group of the patient, which may modify the effectiveness of treatment with tacrolimus ophthalmic suspension 0.1%,” the researchers noted. “When acute exacerbations of AKC and VKC make topical tacrolimus treatment inadequate, treatment of allergic inflammation needs to be augmented with a steroid regimen.”
Hirota A, Shoji J, Inada N, et al. Evaluation of clinical efficacy and safety of prolonged treatment of vernal and atopic keratoconjunctivitis using topical tacrolimus. Cornea. 2022;41(1):23-30. |

