Optometric SurgeryThe scope of practice has expanded for optometrists in several states over the last few years to include minor ocular surgery and use of lasers. Today, 10 states allow ODs to perform these advanced procedures, which are on their way to becoming ingrained into the profession's DNA. Whether your state already has or has yet to expand its optometric practice scope, this month's issue of Review of Optometry intends to prepare ODs across the country to tackle these new opportunities when their time comes. Check out the other articles featured in the December issue:
|
Modern cataract surgery has become so refined that risks are relatively low and complications are minimal. Posterior capsular opacification (PCO) is the most common postoperative complication, and most cases are easily managed. Capsulotomy using a neodymium-doped yttrium aluminum garnet (Nd:YAG) laser is the most effective treatment currently available.1,2
PCO
This condition impairs patients’ quality of vision through reduced visual acuity, decreased contrast sensitivity, glare disability and monocular diplopia; ophthalmic examinations are also impeded.2 Despite today’s advancements in surgical technologies and lens design, PCO still occurs in up to 23% of patients from a few months to years after cataract surgery.3 The overall occurrence has been reported as high as 50% in adults and 100% in children.2
Development of PCO is influenced by a multitude of factors. Patient-related characteristics known to increase the risk of PCO include younger age, advanced-stage cataract, type of cataract (i.e., subcapsular) and history of uveitis. Intraocular lens (IOL) factors such as rounded-edge IOLs, hydrophilic materials and one-piece IOLs have shown a higher association with PCO formation.2,4
PCO involves residual lens epithelial cells still present in the capsular bag after cataract removal. Migration, proliferation and differentiation of leftover lens epithelial cells is thought to be a wound-healing response following cataract surgery and the main cause of PCO.
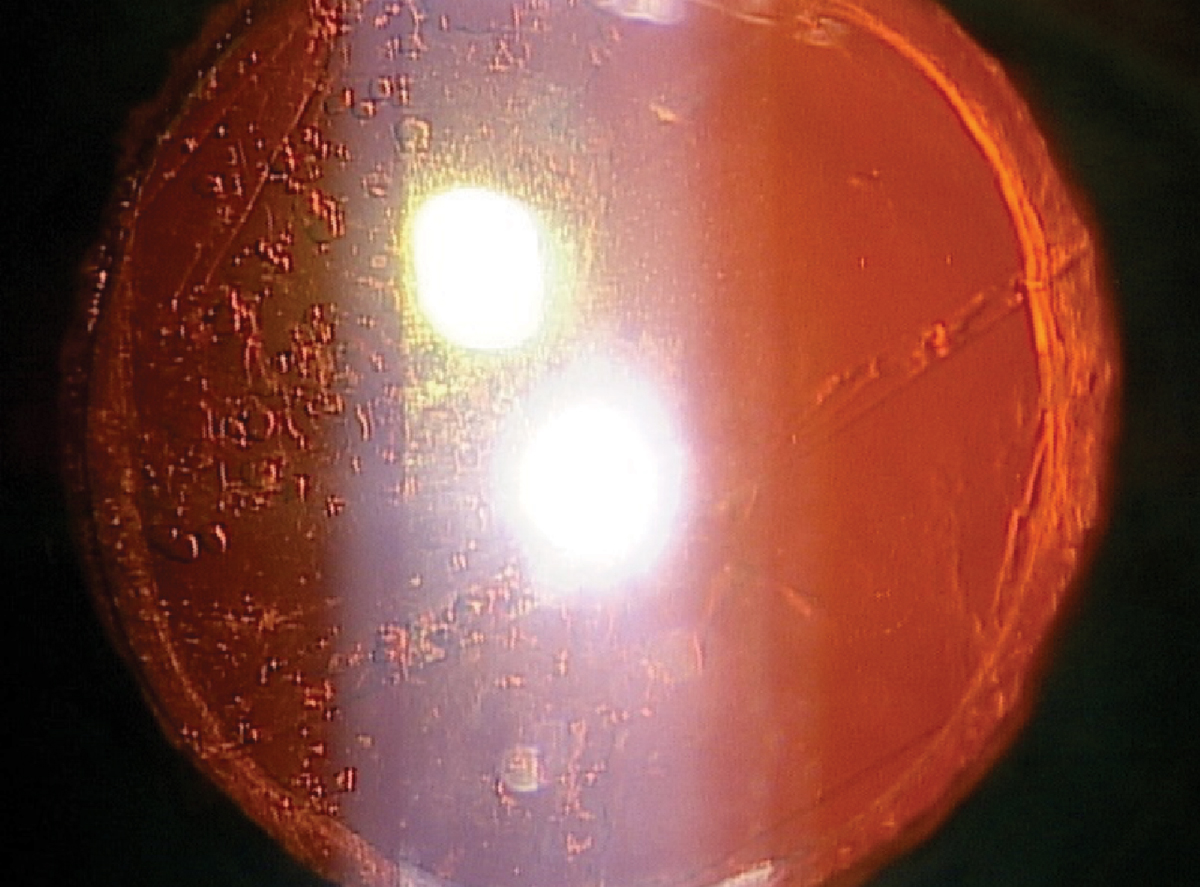
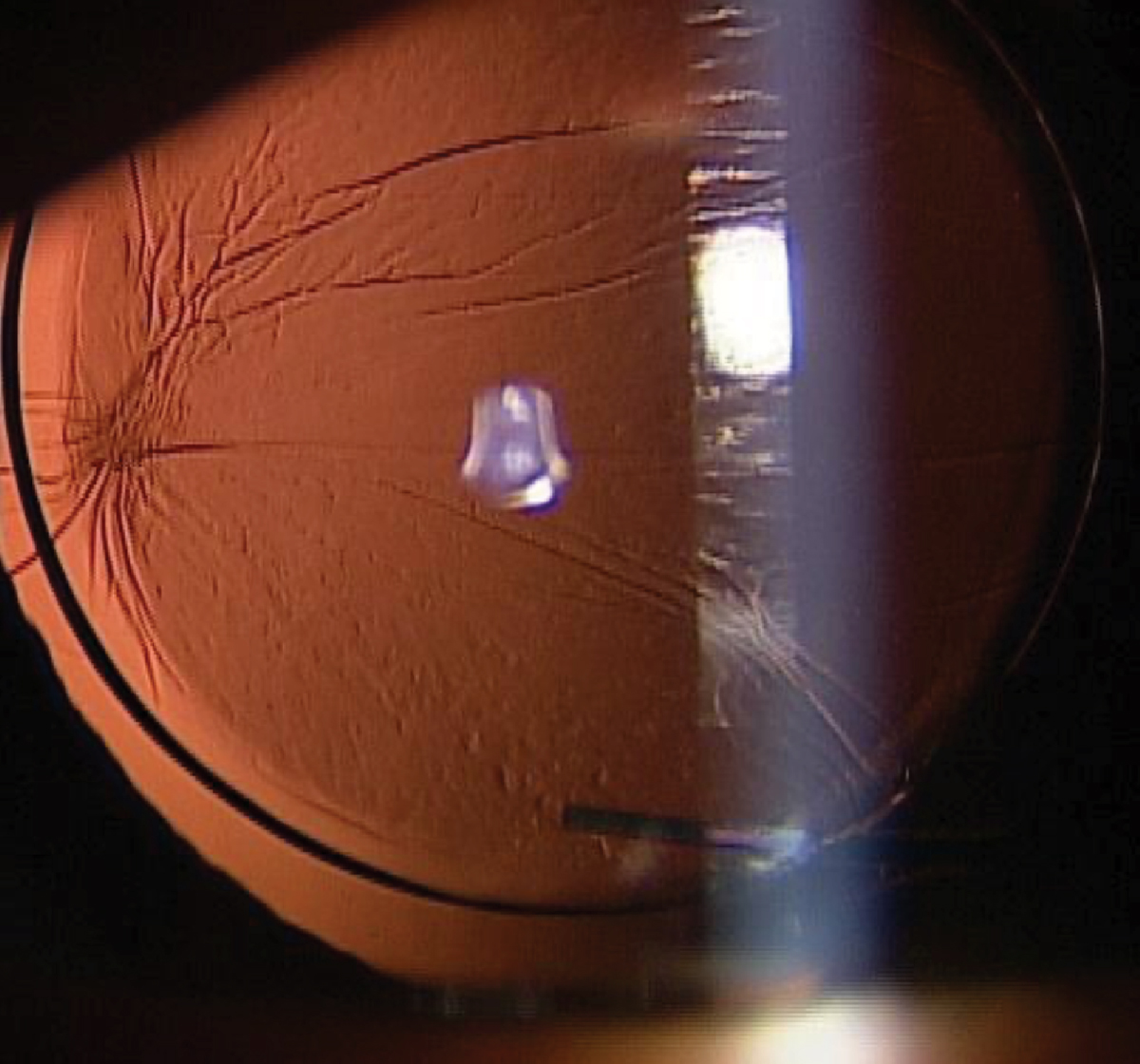
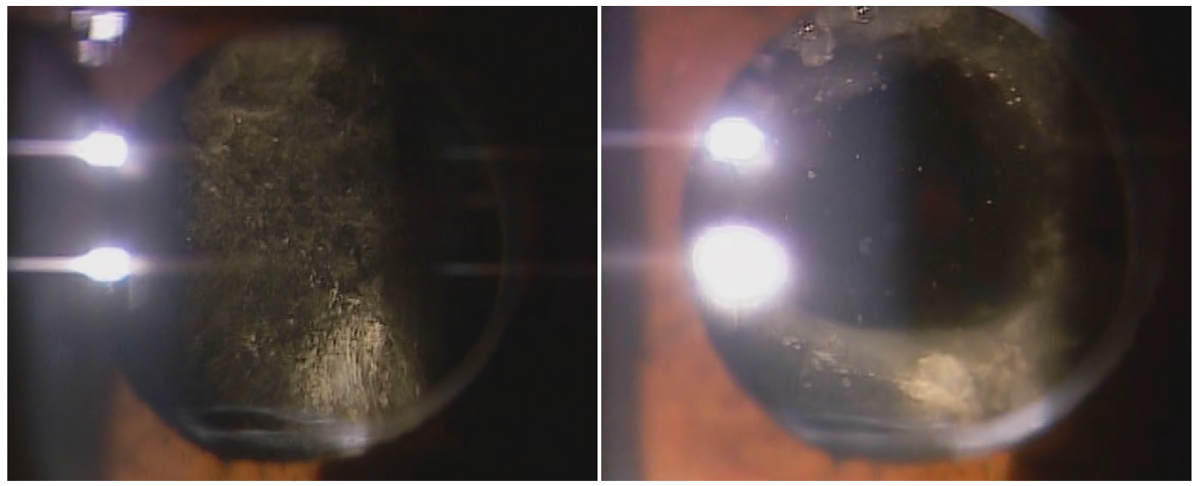
There is more than one pattern of opacification. Pearl-type (vacuolated) PCO forms when lens epithelial cells undergo crystalline-expressing lenticular regeneration, appearing as clusters or grape-like collection of swollen lens epithelial cells commonly termed Elschnig pearls, or a peripheral annular ring of cells called a Soemmering ring. Fibrosis-type PCO is caused by fibrous metaplasia that produces folds and wrinkles in the posterior capsule. Posterior capsular distension syndrome occurs when the lens remnants become trapped, absorb water and appear fluffy white. Intraoperative distortion of the bag can lead to mechanical PCO irregularities of variable presentations.
Clinically, PCO classification comes into play when choosing energy level settings used during laser treatment.1
 |
|
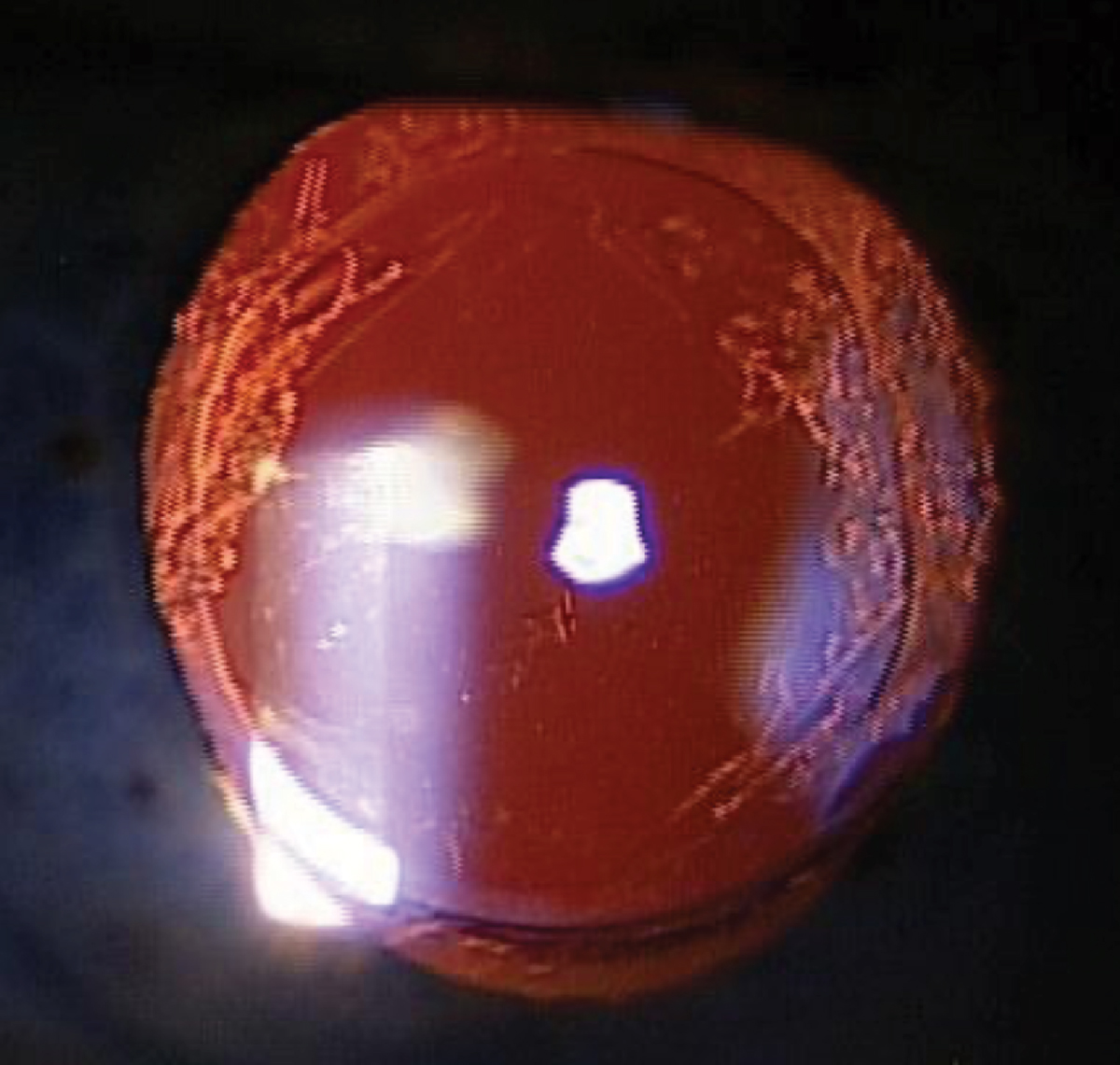
Elschnig pearls observed by retroillumination. Click image to enlarge. |
Laser History
Nd:YAG laser capsulotomy is the standard treatment for PCO. Ophthalmic use of the laser was first introduced in the early 1980s, offering a safer and less invasive alternative to earlier surgical discission techniques.5 A quick, high-powered pulse of the 1,064nm wavelength laser produces a plasma microexplosion that induces a shockwave that disintegrates the offending opacified capsule tissue.6
Although Nd:YAG capsulotomy offers a relatively fast and safe treatment for PCO, it may still pose risks to the patient. Careful consideration must be taken before, during and after the procedure to ensure effective surgical outcomes and limit potential complications.
Indications and Contraindications
Nd:YAG capsulotomy is indicated in cases of PCO that limit patients’ vision-related activities or interfere with ocular disease management. Multifocal IOLs are more likely to render visual symptoms with earlier stages of PCO. Decreased visual acuity of two lines or more in normal lighting or by glare testing, known as brightness acuity testing (BAT), may be required for insurance qualifications; however, it is important to consider treatment in cases where subjective visual decline is greater than clinical signs.
Capsular contraction syndromes require treatment if opacification within the pupil margin or refractive shifts are observed, especially with plate haptic or pseudo-accommodating IOLs. Additionally, if pseudophakic patients undergo corneal refractive surgery enhancement, a “pre-refractive” capsulotomy is warranted.6
Contraindications for performing Nd:YAG capsulotomy include patients who are unable to fixate or sit still, glass IOL material and calcified IOL surfaces seen with older implant materials. Address any active ocular pathologies like uveitis or cystoid macular edema (CME) beforehand. Corneal pathology (scars, opacities and dystrophies) may obscure adequate views, thus making the procedure slightly more challenging. Patients with a high risk of retinal detachment must be monitored closely in the postoperative period.7
 |
|
Folds and wrinkles observed by retroillumination. Click image to enlarge. |
Informed Consent Considerations
Paper or electronic means of informed consent with signatures from the patient, the clinician and a witness (typically a staff member) are important to obtain before the procedure. The form should include a simple explanation of the Nd:YAG capsulotomy, its indications, alternative treatments, postoperative expectations and possible adverse effects. A statement outlining that the counseling clinician discussed the procedure, risks, benefits, contraindications and expected results with the patient should be documented.6
Pre-op Care
A comprehensive eye examination is required prior to performing the Nd:YAG capsulotomy with a record of best-corrected visual acuity and/or BAT. Dilated assessment of the anterior segment should include careful attention to any corneal opacities, the degree of capsular opacification and IOL positioning.6 Posterior segment evaluation is also required to assess the risk of retinal detachment, CME, ocular inflammation or other ocular pathology that may contribute to the patient's visual complaints.6
Procedure
Let’s now review how to perform a Nd:YAG capsulotomy.6
1. Instill preoperative medications. One drop of topical alpha-agonist, such as brimonidine (0.1% to 0.2%) or apraclonidine (0.5% to 1%), is instilled into the eye being treated. Use topical proparacaine in both eyes to control blink reflexes and improve patient comfort.
2. Review the laser settings.
a. Offset: 100µm to 250µm posterior for posterior capsulotomies. The offset allows the actual center of the shockwave away from the targeted plane to avoid unwanted damage to adjacent structures like the IOL.
b. Energy: 1.0mJ to 1.8mJ initially. The lowest energy to complete the procedure is best; however, higher energy may be needed when treating more dense opacification.
c. Pulse: Single
d. Spot size and pulse duration: fixed. This cannot be altered with the Nd:YAG laser.
3. Align the patient in the slit lamp. Advise the patient to focus on the fixation light and hold steady. Stabilization with an assistant or strap may be helpful in certain situations. Patients should be made aware of what to expect, including any “pops” or “clicks” as the laser fires and sensations behind the eye or head may be felt throughout the procedure.
4. Insert the capsulotomy laser lens (optional). Using a coupling solution such as Celluvisc (1% carboxymethyl cellulose, Allergan) or Gonak (2.5% hypromellose ophthalmic demulcent, Akorn) in the lens well, place the lens on the patient’s eye. A survey of ophthalmologists in 2015 reported 53% used a contact laser lens for this procedure.8 If not using the lens, artificial tears may be helpful in patients with ocular surface disease.
5. Fire the laser. The laser emits two beams that become one when the laser is focused. Starting outside the visual axis, align the laser on the posterior capsule and fire each laser spot immediately adjacent to the prior one. The capsular tissue can often be seen peeling away after the tension lines are loosened with each shot. Maintain at least 1mm to 1.5mm of untreated capsule from the edge of the IOL. There are two main patterns to firing depending on the physician:
a. Cruciate pattern. Starting at 12 o’clock, work vertically to six o’clock, then create the cross pattern, dissecting the horizontal from the center to periphery. Treat the remaining capsule flaps to retract out of the visual axis and enlarge the opening.
b. Circular pattern (“can opener”). Starting at seven o’clock, following a clockwise fashion peripherally until the inner capsular tissue falls posteriorly. With this method, no shots are along the visual axis, which may be beneficial for patients with retinal conditions or increased risk of CME.
 |
|
Posterior capsular distension syndrome before and after Nd:YAG capsulotomy. Click image to enlarge. |
6. Re-examine the capsule. Using retroillumination, inspect the treatment area for any strands or capsule remaining requiring further treatment.
7. Instill postoperative medications. After the procedure, one drop of topical alpha-agonist is instilled in the treated eye to reduce the risk of an intraocular pressure (IOP) spike.
8. Check IOP. Do this within one hour after the procedure, usually around 30 minutes.
9. Document the case. Thorough documentation of the laser settings, number of shots and total energy must be recorded, along with any intraoperative issues and the post-laser IOP measurement. The number of laser shots and total energy is highly variable depending on the severity of capsular opacification. A gross estimate is typically between 15 to 50 pulses with a total energy of 30mJ to 40mJ.
Studies show higher complication rates associated with total energy levels around 60mJ to 80mJ. If high energy levels are reached before treatment is completed, a second treatment on a different day may be indicated based on risk assessment.9
Post-op Care
Prescribing topical NSAID or topical corticosteroid for one to two weeks following the procedure is strongly recommended to control postoperative inflammation.6 Educate the patient on the likelihood of them experiencing a mild amount of floaters within the first few days, which will decrease with time. They should also be counseled on signs and symptoms of a retinal detachment and advised to return to the clinic immediately should they occur.
A follow-up appointment should be booked one to two weeks post-procedure. Visual acuity, IOP measurement and dilated fundus examination should be performed at this visit. If the desirable outcome is reached, the other eye may be treated at this time, if required.6
 |
|
Clear posterior lens capsule after Nd:YAG capsulotomy. Click image to enlarge. |
Managing Complications
As with any ocular procedure, there is a risk of potential complications associated with YAG capsulotomies. Visually debilitating adverse events are uncommon but can include IOP elevation, IOL damage, uveitis, CME and retinal detachment.5
IOP elevation. The most common complication reported following laser capsulotomy treatment is increased IOP, with incident rates of 15% to 30% of cases in several studies.7 IOP begins to rise immediately post-procedure, although it is almost always transient, peaking at three to four hours.
Different explanations proposed for the rise in IOP include deposition of debris in the trabecular meshwork and angle closure from inflammation of the ciliary body. Other procedural factors like larger capsulotomy size and higher total energy have been correlated to greater increases in IOP. Prophylactic use of IOP-lowering medications substantially reduces the risk of IOP spikes, especially important in high-risk patients such as those with advanced glaucoma or steroid-responders.10
IOL damage or “pitting.” Laser energy focused too far anteriorly can result in shockwave damage to the IOL. Patient movement, inaccurate focusing of the laser and IOL material can be attributed to IOL pitting.6 Silicone material is more susceptible to damage, while acrylic materials are more forgiving. Pitting is rarely visually significant, although damage can occasionally cause glare or distortion, more so with multifocal IOLs. Adjusting the offset and starting treatment outside the visual axis can help minimize IOL pitting.10,11
IOL movement. The Nd:YAG capsulotomy procedure has been shown to induce a posterior movement of the IOL. However, the significance of this on refractive error is debated. Both reported findings are more pronounced with larger capsulotomy openings, thus smaller treatment areas can limit this complication.5
Uveitis. Transient anterior chamber reaction can be observed after Nd:YAG capsulotomy, which should be controlled with postoperative topical corticosteroids. Delayed complications and persistent iritis and vitritis are rare.5
CME. Any intraocular surgical procedure, trauma and several inflammatory conditions can cause a nonspecific inflammatory response in the macular area. The movement of the vitreous cavity, vitreous damage and vitreoretinal traction, resulting in the release of inflammatory mediators have been postulated mechanisms that induce CME development. Occurrences are low, especially if Nd:YAG capsulotomy was delayed for over six months after cataract surgery, but should be treated with topical corticosteroids and topical NSAIDs.10
Retinal detachment. Although data on the incidence of this after Nd:YAG capsulotomy is inconsistent, the rare but significant potential complication has been estimated to occur in 0.5% to 3.6% in patients who undergo laser treatment compared with no treatment.10 Stronger associations were found in patients with a history of retinal detachment, lattice degeneration, axial length greater than 24mm and posterior capsule rupture during surgery. This reiterates the significance of a thorough peripheral fundus examination prior to performing Nd:YAG capsulotomy to preoperatively address retinal defects or identify patients who need close monitoring.5
Takeaways
Nd:YAG capsulotomy is extremely effective and is the standard of care for treating symptomatic PCO. Improvement in visual acuity occurs in up to 96% of patients with guarded prognosis in patients with pre-existing ocular disease.7 Despite being a frequently performed, safe and noninvasive procedure, knowledge regarding appropriate techniques is key to limit the risk of potential complications and open a world of clear vision for our patients.
Suggested reading: The Ophthalmic Laser Handbook Chapter 17: Nd:YAG Capsulotomy written by Jason Ellen, OD, and Sophia Leung, OD.6
Dr. Cappellani is a cornea and contact lens resident at Northeastern State University Oklahoma College of Optometry in Tahlequah, OK. She is a Fellow of the American Academy of Optometry. She has no financial disclosures.
Dr. Leung practices at Seema Eye Care Centre in Calgary, Alberta in Canada. She is a Diplomate of the American Board of Optometry, a Fellow of the American Society of Optometric Surgeons and a Diplomate of the American Academy of Optometry in the anterior segment section. Dr. Leung has been a consultant and speaker for Lumenis.
1. Awasthi N, Guo S, Wagner BJ. Posterior capsular opacification: a problem reduced but not yet eradicated. Arch Ophthalmol. 2009;127(4):555-62. 2. Konopińska J, Młynarczyk M, Dmuchowska DA, Obuchowska I. Posterior capsule opacification: a review of experimental studies. J Clin Med. 2021;10(13):2847. 3. Ursell PG, Dhariwal M, O'Boyle D, et al. Five-year incidence of YAG capsulotomy and PCO after cataract surgery with single-piece monofocal intraocular lenses: a real-world evidence study of 20,763 eyes. Eye. 2020;34(5):960-8. 4. Wu S, Tong N, Pan L, et al. Retrospective analyses of potential risk factors for posterior capsule opacification after cataract surgery. J Ophthalmol. 2018;2018:9089285. 5. Karahan E, Er D, Kaynak S. An overview of Nd:YAG laser capsulotomy. Med Hypothesis Discov Innov Ophthalmol. 2014;3(2):45-50. 6. Ellen J, Leung S. Nd:Yag capsulotomy. In: Freisber L, Lighthizer N, Skorin L, et al., eds. The Ophthalmic Laser Handbook. Lippincott Williams & Wilkins; 2021:274-89. 7. Steinert RF. Nd:YAG laser posterior capsulotomy. American Academy of Ophthalmology. www.aao.org/current-insight/ndyag-laser-posterior-capsulotomy-3. Published November 4, 2013. Accessed October 5, 2022. 8. Gossman, M. YAG capsulotomy, part 1. EyeWorld. 2015;20(6),29-30. 9. Bhargava R, Kumar P, Phogat H, Chaudhary KP. Neodymium-yttrium aluminium garnet laser capsulotomy energy levels for posterior capsule opacification. J Ophthalmic Vis Res. 2015;10(1):37-42. 10. Aslam TM, Devlin H, Dhillon B. Use of Nd:YAG laser capsulotomy. Surv Ophthalmol. 2003;48(6):594-612. 11. Borkenstein AF, Borkenstein EM. Analysis of YAG laser-induced damage in intraocular lenses: characterization of optical and surface properties of YAG shots. Ophthalmic Res. 2021;64(3):417-31. |