 |
|
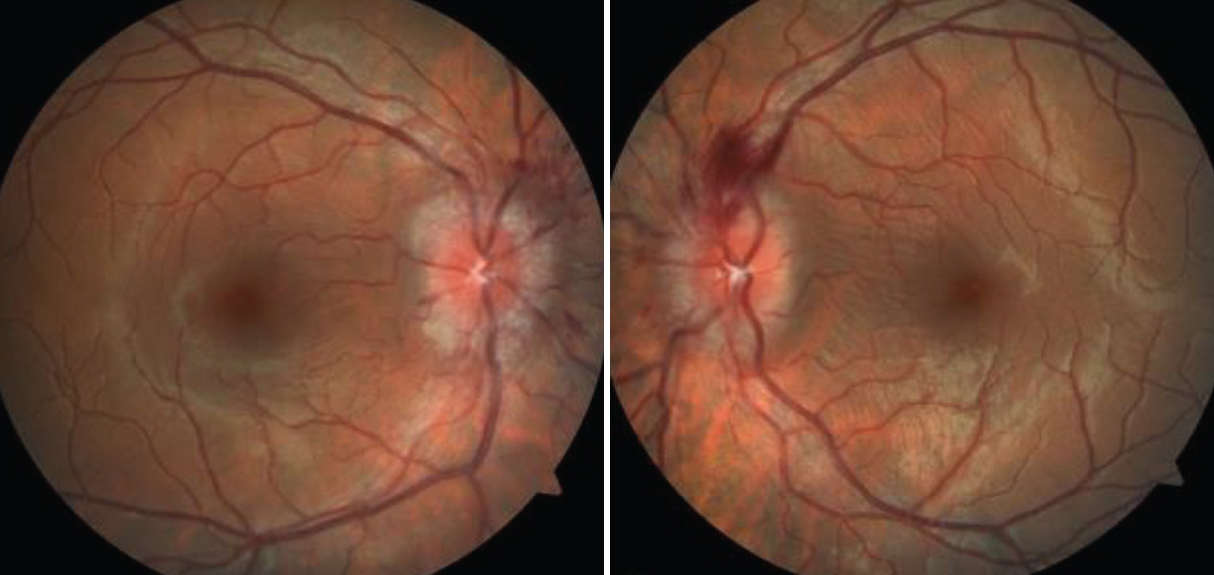
“Papilledema” is commonly used erroneously to describe other visual occurrences. Photo: Paige Thompson, OD. Click image to enlarge. |
Most practicing clinicians know that papilledema refers to optic disc edema (ODE) secondary to raised intracranial pressure (ICP) and that the condition is a leading reason for referral to neuro-ophthalmology. If managed inappropriately, papilledema may cause permanent blindness. Given the gravity of such a diagnosis, it must be distinguished from other causes of ODE as the word implies a unique pathophysiology and management strategy; however, a study in Ophthalmology has determined that the term is often applied wrongly.
Upon conducting a database search, a team of researchers included case reports with “papilledema” in the title, abstract or keywords. Studies were graded for the following errors:
- using papilledema without evidence of elevated ICP (type one)
- declaring papilledema on examination before finding evidence of elevated ICP (type two)
- both of the above (type three)
Among 722 case reports, there were 12 type one errors, 360 type two errors, 110 type three errors and 240 studies had no errors. Ophthalmology, neurology and neurosurgery were the most represented fields, yet only ophthalmology had a low prevalence of errors among all specialties. Regardless, all specialties with at least 10 included reports had a high error prevalence (>30%).
Two potential consequences can arise from error types one and three, especially when papilledema and its unique clinical workup are no longer distinguished from other causes of ODE. In the case of “false” papilledema, a misinformed practitioner may apply papilledema-specific diagnostic and management strategies to this unrelated case of ODE. This error limits the scope of clinical workup to finding and reducing ICP, thereby overlooking the true and potentially harmful diagnosis that goes unmanaged. Alternatively, in the case of “true” papilledema, the misinformed practitioner may apply diagnostic and management strategies that are unrelated to ICP but indicated for other causes of ODE. The type two error is misleading as it falsely implies underlying raised ICP, which can influence practitioners to overdiagnose and treat for papilledema according to its unique clinical workup.
Reduced error prevalence was significantly associated with higher-impact journals, non-open access publication models and origin countries with English as the official language. Error prevalence was not significantly associated with publication year. The relationship between article citation counts and the prevalence of error did not reach significance. Risk of bias analysis indicated that error occurrence was unrelated to the quality of the case report study design.
“When allowed to propagate, this error can mislead care delivery to patients with ODE,” the study authors wrote. “Our results, while limited to case reports, indicate a need for more thorough peer review standards and neuro-ophthalmology exposure in medical education.”
They noted that clinicians who routinely evaluate patients for ODE and optic neuropathy should continue offering medical education to clarify misconceptions on papilledema and inform more effective clinical practice.
Tao B, Vosoughi A, Margolin E, Micieli J. Inappropriate use of the team “papilledema” in the medical literature: a systematic review of case reports across specialties. Ophthalmology. October 1, 2022. [Epub ahead of print]. |

