Obesity is the fastest-growing epidemic in the United States, according to the U.S. Assistant Surgeon General.1 The prevalence of obesity in the United States was 20.9% in 2001, a 5.6% increase from a year earlier and a 74% increase from 1991.2 With an estimated U.S. population of 296.5 million, that means about 62 million adults in the United States were obese in 2001.3
A national health objective for the year 2010 is to reduce the prevalence of obesity among adults to less than 15%.4 However, statistics indicate that the situation is getting worse rather than improving.4 Globally, more than 1 billion adults are overweight, and at least 300 million of them are obese.5 With an estimated world population of 6.5 billion, that means 15.4% are overweight, and 4.6% are obese.6
Obesity affects ocular as well as systemic health. Given our role in the patients well being, we cannot turn a blind eye to obese patients.
Measures of Obesity
Obesity is defined as excess body fat relative to lean body mass.7 We most commonly measure and diagnose obesity by body mass index (BMI). BMI is a simple calculation of weight (kg) divided by height (m2). Using pounds and inches, BMI equals weight divided by [height (inches)]2 and then multiply the quotient by 703.
Adults ages 20 years and older are considered underweight if BMI is less than 18.5, normal if BMI is 18.5 to 24.9, overweight if BMI is 25 to 29.9 and obese if BMI is 30 or more. BMI for children and teens (ages 2 to 20) is plotted on age- and gender-specific growth charts.
Another measure of obesity: abdominal obesity. This represents the additional weight an individual gains in the abdominal region. There are two ways to determine abdominal obesity:
Waist circumference. A normal waist circumference is less than 40 inches for men and less than 35 inches for women. A waist circumference that exceeds these normal values is a health risk.8-10
Waist-to-hip ratio. This measure compares the waist measurement at the smaller circumference of the natural waist, usually just above the navel, to the hip measurement at the widest part of the buttocks. Individuals who have apple- shaped bodies (more weight around the waist) face more health risks than those whose bodies are pear-shaped (more weight around the hips).11
Any person whose waist is bigger than his or her hips is at high risk for obesity-related complications (see Waist-to-Hip Ratio Health Risk Factors, below).
|
Waist-to-Hip Ratio |
| Health Risk Male Female Low 0.95 or 0.80 or less less Moderate 0.96 to 0.81 to |
Systemic Problems
Obesity is a major contributor to chronic disease and disability.
Diabetes is the most common comorbidity associated with obesity.13 Diabetes is so closely associated with obesity that Shape Up America, a nonprofit organization that raises public awareness about obesity, coined the term Diabesity, which refers to the causal connection between obesity and type 2 diabetes.14 According to Shape Up America, 97% of all cases of type 2 diabetes are due to excessive weight. Obese people are five times more likely to develop diabetes than smokers, and they are at an even higher risk than that due to the effects of 20 years of aging.15
Obesity also is a well-known independent risk factor for heart disease, which itself is the most common cause of mortality in developed countries.16,17 Other common complications of obesity are genitourinary complications, obesity hypoventilation syndrome, sleep apnea, acid reflux, osteoarthritis, gout, hepatic disease, various forms of cancer, depression, dementia, periodontitis, gallstones, kidney stones, various dermatological conditions and premature death.18-40
Metabolic syndrome is a combination of several of the entities mentioned above. It is characterized by central obesity, dyslipidemia, raised blood pressure and insulin resistance.41
Visual Impact
In addition to these systemic conditions, obesity can result in serious consequences to patients ocular health and may cause significant visual disabilities. Ocular complications of obesity include:
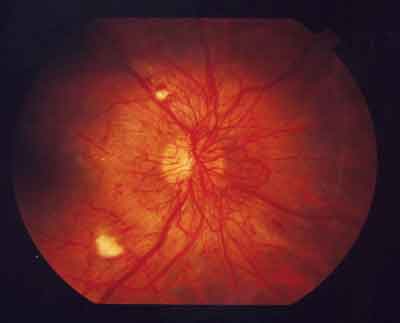
Diabetic retinopathy. Besides its link to diabetes, obesity is a risk factor for the pathogenesis of diabetic retinopathy and other microvascular abnormalities associated with diabetes.42-45 Specifically, high BMI and a high waist-to-hip ratio are significant risk factors for the development of diabetic retinopathy.
|
|
|
Obesity is a risk factor for the pathogenesis of diabetic retinopathy. |
Obesity increases the risk of AMD due to the physiologic changes that occur with obesity.49 These include increased oxidative stress, changes in the lipoprotein profile and increased inflammation. Such changes result in increased destruction and decreased circulatory delivery of lutein and zeaxanthin to the macula of the eye.49
Overall obesity and abdominal obesity increase the risk that patients in the early or intermediate stages of macular degeneration will progress to advanced AMD.50 However, increased physical activity tends to decrease the risk of AMD progression.
Cataracts. Numerous studies cite obesity as a risk factor for cataract development, particularly cortical and posterior subcapsular cataracts.51-56 In one study, for example, patients whose BMI was 30kg/m2 had a 36% higher risk of any type of cataract than those whose BMI was less than 23kg/m2. The association was strongest for posterior subcapsular cataract (PSC), possibly due to glucose intolerance and insulin resistance, even in the absence of clinical diabetes.51
Analysis of data from more than 20,000 patients in the Physicians Health Study found that BMI as well as height and abdominal adiposity are independent risk factors for cataract, suggesting that weight loss and reduction of central obesity would lessen the incidence and costs of cataract.53 And, the Barbados Eye Study found that high prevalence of cortical opacities was related to diabetes, hypertension and abdominal obesity, which also are common in this and black populations. Interventions to modify these risk factors, especially in high-risk populations, may help stem cataract-induced vision loss .54
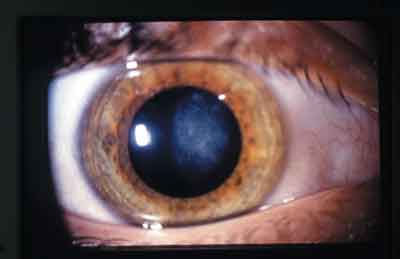 |
| Numerous studies cite obesity as a risk factor for cataract development. |
Obesity can also affect IOP measurements. IOP in obese patients was falsely elevated by an average 4.7mm Hg when measured with the Goldmann applanation tonometer vs. a Perkins hand-held tonometer, one study found.62 These patients had an average BMI of 34. By contrast, patients whose BMI was normal had a mean difference of 0.33mm Hg.
One possible explanation for these findings: Obese patients may hold their breath as they strain to get their faces into the slit-lamp biomicroscope for Goldmann tonometry. This compresses the thorax, causing a subsequent increase in venous pressure and a transitory elevation of IOP. Hand-held tonometry in obese patients may help avoid a false diagnosis of elevated IOP. (See Accommodate the Obese Patient, below.)
|
Accommodate the Obese Patient |
| Many obese patients are effectively disabled and require special considerations when they visit an optometric office. Some ways to accommodate obese patients: Make sure your office is wheelchair accessible. This includes ramps or elevators and doors that are wide enough even for wide wheelchairs to pass through. Have proper seating. A loveseat or a couch in your waiting area will make ambulatory obese patients more comfortable than if they had to squeeze between the arm rests of a standard-sized chair. Also, have an examination chair with armrests that tilt back or can be removed if the patient cannot fit between the armrests. Use hand-held instruments. It is difficult for extremely obese patients to lean forward and put their chin in a chin rest. A hand-held tonometer and slit lamp biomicroscope can be very useful for these patients. |
Floppy eyelid syndrome (FES). The recent literature and several well-known textbooks list obesity as a risk factor for floppy lid syndrome.65-67 FES usually affects middle-aged obese men.65 There is some association between FES and obstructive sleep apnea, which is also associated with obesity.65
Pseudotumor cerebri. Pseudotumor cerebri, also known as benign intracranial hypertension, has long been associated with obesity in females.68-70 Although pseudotumor cerebri rarely occurs among males, obesity does not appear to be a risk factor for males who do develop the condition.71
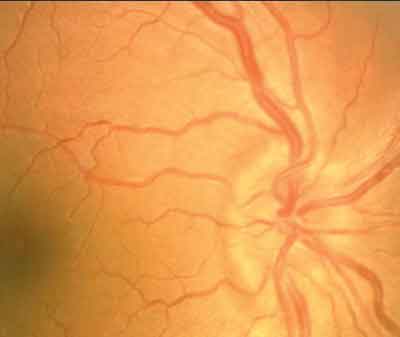 |
|
This patient with pseudotumor cerebri has an edematous optic nerve. |
The Optometrists Role
Given the association of obesity with blinding eye diseases, you must educate patients about the complications that can result from obesity. To do so, you need to:
Identify which patients require education and counseling. A diagnosis of obesity can be made according to the patients BMI. O.D.s who work in multi-disciplinary settings have access to this information. However, we normally do not collect those vital signs as part of our examination.
Some possible solutions: Acquire a scale, and measure each patients height and weight; include height and weight questions in your patient history (keep in mind that the reliability of the patients answers can be questionable); or visually assess the patients waist-to-hip ratio.
Educate the patient about the ocular manifestations of obesity. Make sure the patient understands that you are concerned about his or her ocular health and not just appearance. Patients may be more concerned about their vision than their systemic health, so education may motivate them to pursue a healthier lifestyle and lose weight.
Offer ideas about how to lose weight. One possible resource: the National Weight Control Registry (www.nwcr.ws), a database of people who have self-reported a weight loss of 30 pounds or more and kept it off for at least a year. Participants answer researchers questions about how they achieved their weight loss. The researchers who maintain the NWCR found that 89% changed their diets and increased physical activity (10% used diet modification only and 1% used activity only).73
Because obesity generally results from too much caloric intake combined with too little physical activity, treatment of obesity should address both causes. The three basic approaches for the prevention and treatment of obesity are to reduce the dietary energy intake, increase the energy spent on activity, and reduce inactivity.74 One way to help obese patients is to offer specific suggestions on how to lose weight. (See Prescription for Weight Loss, below).
|
Prescription for Weight Loss 78 |
| Nutrition Set regular times to eat. Eat three meals and no Increased physical activity Reduced inactivity |
Seek additional help. Consider referring the patient to a dietician or general practitioner for more detailed education and follow-up care. Other resources that may be helpful: an exercise physiologist, physical therapist and bariatric surgeon (for gastric bypass surgery).
As a primary health-care provider, you must know how obesity affects your patients ocular health. It is equally important to educate overweight and obese patients about healthier lifestyle choices, as these choices will reduce their risk for co-morbid ocular and systemic conditions.
Dr. Bohlman practices at the Mountain Home VA Medical Center in Johnson City, Tenn., and lectures on obesity.
1. Blumenthal S. US Assistant Surgeon General discusses Obesity Problem. Harvard Public Health NOW. March 19, 2004. www.hsph.harvard.edu/now/mar19/. (Accessed August 18, 2005)
2. Overweight and Obesity: Obesity Trends: 19912001 Prevalence of Obesity Among U.S. Adults by State www. cdc.gov/nccdphp/dnpa/obesity/trend/prev_reg.htm. (Accessed August 22, 2005)
3. Population Reference Bureau. www.prb.org/. (Accessed September 14, 2005.)
4. An overview of Overweight and Obesity. www.bodyweight. com/0bodyweight/index.htm. (Accessed August 22, 2005)
5. Puska P, Nishida C, Porter D. Global Strategy on Diet, Physical Activity and Health. World Health Organization Fact Sheet. www.who.int/hpr/NPH/docs/gs_obesity.pdf. (Accessed September 14, 2005.)
6. Population Reference Bureau. www.prb.org/. (Accessed September 14, 2005.)
7. Bray GA, Greenway FL. Current and potential drugs for treatment of obesity. Endocr Rev 1999 Dec;20(6):805-75.
8. Janssen I, Katzmarzyk PT, Ross R. Body mass index, waist circumference, and health risk evidence in support of current
National Institutes of Health guidelines. Arch Intern Med 2002 Oct 14;162(18):2074-9.
9. Jose Santi M, Carrozas MA, Barba A, et al. Waist circumference as a predictor of insulin resistance in young men. Med Clin (Barc) 2005 Jun 11;125(2):46-50.
10. Yalcin BM, Sahin EM, Yalcin E. Which anthropometric measurements is most closely related to elevated blood pressure? Fam Pract 2005 Oct;22(5):541-7.
11. University of Maryland medical system. www.healthcalculators.org/calculators/waist_hip.asp. (Accessed June 22, 2005)
12. Finkelstein EA, Fiebelkorn IC, Wang G. National medical spending attributable to overweight and obesity: How much, and whos paying? Health Aff (Millwood). 2003 Jan-Jun; Suppl Web Exclusives:W3-219-26.
13. Formiguera X, Canton A. Obesity: epidemiology and clinical aspects. Best Pract Res Clin Gastroenterol 2004 Dec; 18(6):1125-46.
14. Executive Summary, Shape Up Americas Diabesity Conference. March 24-25, 2001. www.shapeup.org/profcenter/ diabesity/ExecSumm.htm. (Accessed March 7, 2005)
15. The Diabesity Connection. www.shapeup.org/diabesity. html. (Accessed September 15, 2005)
16. Hubert HB, Feinleib M, McNamara PM, et al. Obesity as an independent risk factor for cardiovascular disease: a 26-year follow-up of participants in the Framingham Heart Study. Circulation 1983 May;67(5):968-77.
17, Zhu S, Heymsfield SB, Toyoshima H, et al. Race-ethnicity-specific waist circumference cutoffs for identifying cardiovascular disease risk factors. Am J Clin Nutr 2005 Feb;81(2): 409-15.
18. Vahratian A, Zhang J, Troendle JF, et al. Maternal prepregnancy overweight and obesity and the pattern of labor progression in term nulliparous women. Obstet Gynecol 2004 Nov;104(5 Pt 1):943-51.
19. Masho SW, Adera T, South-Paul J. Obesity as a risk factor for premenstrual syndrome. J Psychosom Obstet Gynaecol 2005 Mar;26(1):33-9.
20. Agnani S, Vachharajani VT, Gupta R, et al. Does treating obesity stabilize chronic kidney disease? BMC Nephrol 2005 Jun 15;6(1):7.
21. Kessler R, Chaouat A, Schinkewitch P, et al. The obesity-hypoventilation syndrome revisited: a prospective study of 34 consecutive cases. Chest 2001 Aug;120(2):369-76.
22. Moreno CR, Carvalho FA, Lorenzi C, et al. High risk for Obstructive Sleep Apnea in truck drivers estimated by the Berlin questionnaire: prevalence and associated factors. Chronobiol Int. 2004;21(6):871-9.
23. Di Francesco V, Baggio E, Mastromauro M, et al. Obesity and gastro-esophageal acid reflux: physiopathological mechanisms and role of gastric bariatric surgery. Obes Surg 2004 Sep;14(8):1095-102.
24. Manek NJ, Hart D, Spector TD, et al. The association of body mass index and osteoarthritis of the knee joint: an examination of genetic and environmental influences. Arthritis Rheum 2003 Apr;48(4):1024-9.
25. Sayer AA, Poole J, Cox V, et al. Weight from birth to 53 years: a longitudinal study of the influence on clinical hand osteoarthritis. Arthritis Rheum 2003 Apr;48(4):1030-3.
26. Janssens HJ, van de Lisdonk EH, Bor H, et al. Gout, just a nasty event or a cardiovascular signal? A study from primary care. Fam Pract 2003 Aug;20(4):413-6.
27. Moretto M, Kupski C, Mottin CC, et al. Hepatic steatosis in patients undergoing bariatric surgery and its relationship to body mass index and co-morbidities. Obes Surg 2003 Aug;13(4):622-4.
28. Brea A, Mosquera D, Martin E, et al. Nonalcoholic fatty liver disease is associated with carotid atherosclerosis. A case-control study. Arterioscler Thromb Vasc Biol 2005 May;25(5):1045-50.
29. Roberts EA. Non-alcoholic fatty liver disease (NAFLD) in children. Front Biosci 2005 Sep 1;10:2306-18.
30. Powell EE, Jonsson JR, Clouston AD. Steatosis: Co-factor in other liver diseases. Hepatology 2005 Jun 16;42(1):5-13.
31. Engel LS, Chow WH, Vaughan TL, et al. Population attributable risks of esophageal and gastric cancers. J Natl Cancer Inst 2003 Sep 17;95(18):1404-13.
32. Calle EE, Rodriguez C, Walker-Thurmond K, et al. Overweight, Obesity, and Mortality from Cancer in a Prospectively Studied Cohort of U.S. Adults. N Engl J Med 2003 Apr 24; 348(17):1625-37.
33. Chapman DP, Perry GS, Strine TW. The vital link between chronic disease and depressive disorders. Prev Chronic Dis 2005 Jan;2(1):A14.
34. Rosengren A, Skoog I, Gustafson D, et al. Body mass index, other cardiovascular risk factors, and hospitalization for dementia. Arch Intern Med 2005 Feb 14;165(3):321-6.
35. Ritchie CS, Kinane DF. Nutrition, inflammation, and periodontal disease. Nutrition 2003 May;19(5):475-6.
36. Saito T, Shimazaki Y, Kiyohara Y, et al. Relationship between obesity, glucose tolerance, and periodontal disease in Japanese women: the Hisayama study. J Periodontal Res 2005 Aug;40(4):346-353.
37. Tsai CJ, Leitzmann MF, Willett WC, et al. Prospective study of abdominal adiposity and gallstone disease in US men. Am J Clin Nutr 2004 Jul;80(1):38-44.
38. Taylor EN, Stampfer MJ, Curhan GC. Obesity, weight gain, and the risk of kidney stones. JAMA 2005 Jan 26; 293(4):455-62.
39. Scheinfeld NS. Obesity and dermatology. Clin Dermatol 2004 Jul-Aug;22(4):303-9.
40. Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA 2004 Mar 10;291(10):1238-45.
41. American Heart Association. Metabolic syndrome. Available at: www.americanheart.org/ presenter.jhtml?identifier=4756. (Accessed June 23, 2005)
42. van Leiden HA, Dekker JM, Moll AC, et al. Blood pressure, lipids, and obesity are associated with retinopathy: the hoorn study. Diabetes Care 2002 Aug;25(8):1320-5.
43. van Leiden HA, Dekker JM, Moll AC, et al. Risk factors for incident retinopathy in a diabetic and nondiabetic population: the Hoorn study. Arch Ophth 2003 Feb;121(2):245-51.
44. Costa LA, Canani LH, Lisboa HR, et al. Aggregation of features of the metabolic syndrome is associated with increased prevalence of chronic complications in Type 2 diabetes. Diabetic Medicine 2004 Mar;21(3):252-5.
45. Shera AS, Jawad F, Maqsood A, et al. Prevalence of chronic complications and associated factors in type 2 diabetes. J Pak Med Assoc. 2004 Feb;54(2):54-9.
46. Schaumberg DA, Christen WG, Hankinson SE, et al. Body mass index and the incidence of visually significant age-related maculopathy in men. Arch Ophthalmol 2001 Sep;119(9):1259-65.
47. Smith W, Mitchell P, Leeder SR, et al. Plasma fibrinogen levels, other cardiovascular risk factors, and age-related maculopathy: the Blue Mountains Eye Study. Arch Ophthalmol 1998 May;116(5):583-7.
48. Hammond BR Jr, Ciulla TA, Snodderly DM. Macular pigment density is reduced in obese subjects. Invest Ophthalmol Vis Sci 2002 Jan;43(1):47-50.
49. Johnson EJ. Obesity, lutein metabolism, and age-related macular degeneration: a web of connections. Nutr Rev 2005 Jan;63(1):9-15.
50. Seddon JM, Cote J, Davis N, et al. Progression of age-related macular degeneration: association with body mass index, waist circumference, and waist-hip ratio. Arch Ophthalmol 2003 Jun;121(6):785-92.
51. Weintraub JM, Willett WC, Rosner B, et al. A prospective study of the relationship between body mass index and cataract extraction among US women and men. Int J Obes Relat Metab Disord 2002 Dec;26(12):1588-95.
52. Sanchez-Castillo CP, Lara J, Romero-Keith J, et al. Nutrition and cataract in low-income Mexicans: experience in an Eye camp. Arch Latinoam Nutr 2001 Jun;51(2):113-21.
53. Schaumberg DA, Glynn RJ, Christen WG, et al. Relations of body fat distribution and height with cataract in men. Am J Clin Nutr 2000 Dec;72(6):1495-502.
54. Leske MC, Wu SY, Hennis A, et al. Diabetes, hypertension, and central obesity as cataract risk factors in a black population. The Barbados Eye Study. Ophthalmology 1999 Jan;106(1):35-41.
55. Younan C, Mitchell P, Cumming R, et al. Cardiovascular disease, vascular risk factors and the incidence of cataract and cataract surgery: the Blue Mountains Eye Study. Ophthalmic Epidemiol 2003 Oct;10(4):227-40.
56. Jacques PF, Moeller SM, Hankinson SE, et al. Weight status, abdominal adiposity, diabetes, and early age-related lens opacities. Am J Clin Nutr 2003 Sep;78(3):400-5.
57. Gasser P, Stumpfig D, Schotzau A, et al. Body mass index in glaucoma. J Glaucoma 1999 Feb;8(1):8-11.
58. Lee JS, Choi YR, Lee JE, et al. Relationship between intraocular pressure and systemic health parameters in the Korean population. Korean J Ophthalmol 2002 Jun;16(1):13-9.
59. Savinova OV, Sugiyama F, Martin JE, et al. Intraocular pressure in genetically distinct mice: an update and strain survey. BMC Genet 2001;2(1):12. Epub 2001 Aug 09.
60. Zafra Perez JJ, Villegas Perez MP, Canteras Jordana M, et al. Intraocular pressure and prevalence of occult glaucoma in a village of Murcia. Arch Soc Esp Oftalmol 2000 Mar;75(3):171-8.
61. Oh SW, Lee S, Park C, et al. Elevated intraocular pressure is associated with insulin resistance and metabolic syndrome. Diabetes Metab Res Rev 2005 Sep-Oct;21(5):434-40.
62. dos Santos MG, Makk S, Berghold A, et al. Intraocular pressure difference in Goldmann applanation tonometry versus Perkins hand-held applanation tonometry in overweight patients. Ophthalmology 1999 Dec;105(12):2260-3.
63. Patterson RE, Frank LL, Kristal AR, et al. A comprehensive examination of health conditions associated with obesity in older adults. Am J Prev Med 2004 Dec;27(5):385-90.
64. Bohlman H. Communicating the Ocular and Systemic Complications of Obesity to Patients. Optometry Dec;76(12):701-12.
65. McNab AA. Floppy eyelid syndrome and obstructive sleep apnea. Ophthal Plast Reconstr Surg 1997 Jun;13(2):98-114.
66. Dufek MA, Shechtman DL. Floppy eyelid syndrome: a diagnostic dilemma. J Am Optom Assoc 1999 Jul;70(7):450-4.
67. Mortemousque B, Williamson W, Poirier L, et al. Floppy eyelid syndrome. Apropos of 4 cases and review of the literature J Fr Ophtalmol 1995;18(8-9):542-7.
68. Galvin JA, Van Stavern GP. Clinical characterization of idiopathic intracranial hypertension at the Detroit Medical Center. J Neurol Sci. 2004 Aug 30;223(2):157-60.
69. Carta A, Bertuzzi F, Cologno D, et al. Idiopathic intracranial hypertension (pseudotumor cerebri): descriptive epidemiology, clinical features, and visual outcome in Parma, Italy, 1990 to 1999. Eur J Ophthalmol 2004 Jan-Feb;14(1):48-54.
70. Onwuchekwa AC, Nwankwo CN, Chapp-Jumbo EN. A 14-year-old Nigerian female with idiopathic intracranial hypertension Afr Health Sci 2002 Dec;2(3):124-6.
71. Kesler A, Goldhammer Y, Gadoth N. Do men with pseudomotor cerebri share the same characteristics as women? A retrospective review of 141 cases. J Neuroophthalmol 2001 Mar; 21(1):15-7.
72. Smolders MH, Graniewski-Wijnands HS, Meinders AE, et al. Exophthalmos in obesity. Ophthalmic Res 2004 Mar-Apr;36(2):78-81.
73. American Obesity Association. Achieving weight loss. Available at: www.obesity.org/treatment/weight.shtml. (Accessed October 25, 2005)
74. World Health Organization. Life in the 21st Centurya vision for all. The World Health Report. Geneva, Switzerland: World Health Organization; 1998.
75. Browning DJ. Positioning the obese or large-breasted patient for macular laser photocoagulation. Am J Ophthalmol 2004 Jan;137(1):178-9.
76. Seidell JC, Bakx JC, De Boer E, et al. Fat distribution of overweight persons in relation to morbidity and subjective health. Int J Obes 1985;9(5):363-74.
77. Heart Health Analyzer at www.heartanalyzer.com/whratio.shtml. (Accessed Feb. 22, 2005)
78. Manson JE, Skerrett PJ, Greenland P, et al. The escalating pandemics of obesity and sendentary lifestyle: A call to action for clinicians. Arch Intern Med 2004 Feb 9;164:249-58.