 |
A 68-year-old man presented urgently complaining of vision loss in his right eye that he described as a film or veiling of several days’ duration. He reported an obstruction in his superior right visual field that he felt happened abruptly, though he acknowledged that he may not have fully noticed it for about one day. He couldn’t remember any precipitating incidents.
He didn’t report flashes or cobwebs in his vision, but his retinal history included a retinal break in his right eye that had been lasered several years earlier, and he was alert to any possible symptoms of retinal detachment. The retinal tear occurred shortly after YAG capsulotomy and was promptly treated without subsequent retinal detachment.
The patient also had a history of ocular hypertension, for which he was using timolol 0.5% BID OU, and he reported that his intraocular pressure (IOP) was slightly elevated at his last visit with his previous doctor.
Best-corrected visual acuity was 20/40 OD and 20/20 OS. His eyes were white and quiet. His pupils were reactive without afferent defect. Biomicroscopic evaluation showed a well-centered intraocular lens (IOL) OD with posterior opacification. This, however, was confounding, as he had a solid history of bilateral posterior capsulotomy. There was also a grade 2 anterior chamber cell reaction without flare. IOP was 31mm Hg OD and 21mm Hg OS. His left eye had a well-centered IOL and an open posterior capsule.
Dilated examination revealed that he did indeed have an open capsule in his right eye from the previous capsulotomy. But the opacification seen through his undilated pupil was not the posterior capsule but a large superiorly located piece of retained lens fragment between the IOL and remaining posterior capsule. What was remarkable about this postoperative complication was that his cataract surgery occurred 13 years earlier.
Clearly, his visual obscuration, inflammation and elevated IOP came from the subsequent antigenic response induced by the retained lens, which had now dislodged from a protected space between the IOL and posterior capsule. Hence, his diagnosis was retained lens fragment with late-onset inflammation, often referred to as phacoanaphylaxis, or phacolytic glaucoma.
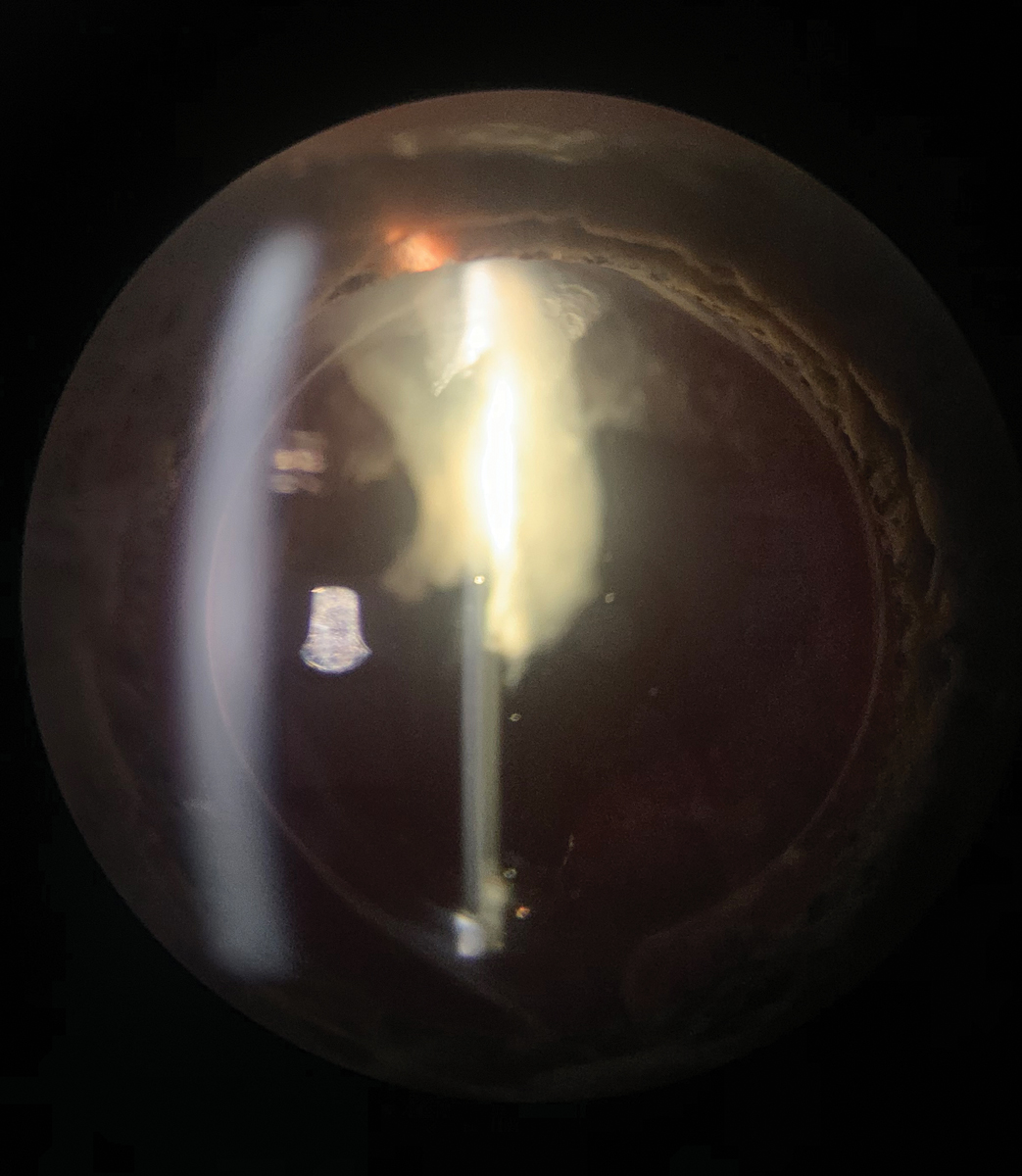 |
| This large retained lens fragment protruding into this patient’s visual axis caused phacoanaphylaxis. Click image to enlarge. |
Dangerous Fragments
Phacoanaphylaxis describes inflammation caused by the crystalline lens and has been referred to as phacoanaphylactic uveitis, phacoanaphylactic endophthalmitis, phacoanaphylactic glaucoma, phacolytic glaucoma, retained lens fragment and lens particle glaucoma.1-6
In nearly all cases, patients are elderly with cataracts, though younger patients experiencing penetrating lens trauma or ocular surgery can also undergo phacoanaphylaxis. Typically, the patient has undergone cataract extraction, often seemingly without complications. In the immediate (and sometimes late) postoperative period, the eye will demonstrate persistent inflammation in the anterior chamber or the vitreous unresponsive to topical steroid treatment. IOP may be elevated, and, when this occurs, the condition is called phacoanaphylactic or phacolytic glaucoma.1-6
Post-surgically, there may be either lens cortex or nucleus material that was inadvertently not completely removed during surgery. Retained lens fragments may be biomicroscopically visible in either the anterior or posterior chamber, though they may be elusive and visible only gonioscopically.7
Phacoanaphylaxis is an inflammatory response to release of sequestered lens proteins, which are recognized as foreign and antigenic even though they are the body’s own tissue. Cortical and nuclear material are enveloped by the lens capsule and thus protected from the body’s immune system. Once released into the anterior or posterior chamber, cortical and nuclear materials induce an antigen-antibody response. Exposed nuclear fragments are more likely to induce phacoanaphylactis than cortical remnants.
Retained lens fragments are extensively infiltrated by polymorphonuclear leukocytes, histiocytes, eosinophils and giant cells. The iris and ciliary body are also inflamed and infiltrated by lymphocytes and plasma cells.2,8 Concurrent inflammation of the trabecular meshwork, as well as blockage by inflammatory cells and a poorly flowing proteinaceous aqueous, contribute to IOP rise and glaucoma development.
The timing of onset of phacoanaphylaxis can be perplexing. Most cases of phacoanaphylaxis occur and are discovered soon after surgery. However, there are numerous reports of phacoanaphylaxis from retained lens fragments occurring years after surgery.9-11
The general consensus held that in late-onset cases, the retained lens material gets stuck in a pocket between the peripheral IOL and posterior capsule, essentially existing in a compartment that retains residual protection from the immune system. However, this does not explain every case of delayed-onset phacoanaphylaxis.
Inflammation Control
Initial inclination in managing persistent postoperative inflammation is to continue or increase steroid use. This may be done initially to temporarily ameliorate the condition, but it is rarely curative. While phacoanaphylaxis from retained cortical fragments may have success with conservative therapy with topical steroids, virtually all cases involving retained nuclear fragments will fail on topical therapy alone, requiring surgical removal.12
As it is difficult to clinically differentiate cortical from nuclear fragments, if the complication of phacoanaphylaxis or phacoanaphylactic glaucoma arises, it is advocated to remove all retained lens fragments as soon as possible.
Topical steroids and cycloplegics can be used temporarily to ameliorate inflammation prior to surgery. Topical aqueous suppressants can be used to manage any significant IOP rises. Therapy is dictated by the severity of the inflammation and IOP rise.
However, if fragments are seen and the eye is quiet, there is no emergent need for extraction; many cases never convert to the inflammatory disease, while others do years later.
Vitrectomy is successful in removing retained lens fragments within the vitreous.13 Surgical irrigation and aspiration with phacoemulsification if necessary is the best approach for lens material in the anterior chamber.14
Prolonged duration of lens fragments in the setting of an inflammatory response increases the risk of corneal decompensation, so prompt intervention is necessary. Unfortunately, some eyes will continue to decompensate even after surgical removal, necessitating keratoplasty.
To Sum Up
The patient presented here was educated on his condition and the nature of his visual disturbance. Upon questioning, we determined that running while playing tennis may have precipitated the dislodgement of his IOL.
He was prescribed prednisolone actetate 1% QID OD and an additional ocular hypotensive fixed combination of brinzolamide 1%/brimonidine 0.2% and referred for removal of the residual lens material. Topical therapy in the four days prior to surgical consultation greatly reduced the patient’s inflammation and IOP. He underwent successful removal of the retained lens fragments with a resultant visual acuity of 20/20.
Dr. Sowka is an attending optometric physician at Center for Sight in Sarasota, FL, where he focuses on glaucoma management and neuro-ophthalmic disease. He is a consultant and advisory board member for Carl Zeiss Meditec and Bausch Health.
1. Mardelli PG, Mehanna CJ. Phacoanaphylactic endophthalmitis secondary to capsular block syndrome. J Cataract Refract Surg. 2007;33(5):921-2. 2. McMahon MS, Weiss JS, Riedel KG, Albert DM. Clinically unsuspected phacoanaphylaxis after extracapsular cataract extraction with intraocular lens implantation. Br J Ophthalmol. 1985;69(11):836-40. 3. Marak GE Jr. Phacoanaphylactic endophthalmitis. Surv Ophthalmol. 1992;36(5):325-39. 4. Oprescu M. The etiopathology of phacoantigenic uveitis and phacolytic glaucoma. Oftalmologia. 1992;36(3):207-13. 5. Moisseiev E, Kinori M, Glovinsky Y, et al. Retained lens fragments: nucleus fragments are associated with worse prognosis than cortex or epinucleus fragments. Eur J Ophthalmol. 2011;21(6):741-7. 6. Teo L, Chee SP. Retained lens fragment in the anterior segment as a cause of recurrent anterior uveitis. Int Ophthalmol. 2010;30(1):89-91. 7. Mokhtarzadeh A, Kaufman SC, Koozekanani DD, Meduri A. Delayed presentation of retained nuclear fragment following phacoemulsification cataract extraction. J Cataract Refract Surg. 2014;40(4):671-4. 8. Hochman M, Sugino IK, Lesko C, et al. Diagnosis of phacoanaphylactic endophthalmitis by fine needle aspiration biopsy. Ophthalmic Surg Lasers. 1999;30(2):152-4. 9. Mokhtarzadeh A, Kaufman SC, Koozekanani DD, Meduri A. Delayed presentation of retained nuclear fragment following phacoemulsification cataract extraction. J Cataract Refract Surg. 2014;40(4):671-4. 10. Pandit RT, Coburn AG. Sudden corneal edema due to retained lens nuclear fragment presenting 8.5 years after cataract surgery. J Cataract Refract Surg. 2011;37(6):1165-7. 11. Asensio-Sánchez VM, Ajamil S, Ramoa-Osorio R, Trujillo-Guzmán L. Sudden macular edema two years after cataract surgery due to retained nuclear fragment. Arch Soc Esp Oftalmol. 2014;89(7):272-4. 12. Zavodni ZJ, Meyer JJ, Kim T. Clinical features and outcomes of retained lens fragments in the anterior chamber after phacoemulsification. Am J Ophthalmol. 2015;160(6):1171-1175. 13. Barthelmes D, Alexander S, Mitchell P, Chandra J. Hybrid 20/23-gauge pars plana vitrectomy for retained lens fragments after cataract surgery. Retina. 2012;32(9):1749-55. 14. Stefaniotou M, Aspiotis M, Pappa C, et al. Timing of dislocated nuclear fragment management after cataract surgery. J Cataract Refract Surg. 2003;29(10):1985-8. |

