Optometrists are the frontline workers in eye care and should be the first source patients turn to for reliable and accurate information about eye health and vision. We also should be providing patient education before problems arise or questions are asked. Finally, we should help patients recognize the circumstances under which they should contact us and help them understand what could happen.
Certainly, the information we give is broadly contextual—we educate aging patients about cataracts, we educate diabetic patients about retinopathy—so who would you preemptively educate about visual hallucinations? How do you frame a conversation around them? How often do you talk to your patients about visual hallucinations in general, especially when they didn’t bring it up? My guess would be “not enough.”
A major area where visual hallucination becomes relevant is in the context of neurodegenerative diseases on the dementia spectrum, all of which involve irreversible and progressive neuronal loss.1 Here, we’ll focus on visual hallucinations in the context of common dementia spectrum disorders.
 |
|
One minor visual hallucination—illusion—involves the patient transiently seeing one object as another, such as a book for a bird. Click image to enlarge. |
Classification and Causes
Visual hallucinations are visual perceptions that occur without a corresponding visual stimulus; they occur due to neural activity without visual input. They can be simple (e.g., photopsias, lines, dots, shapes or checkerboard patterns) or complex (formed images, e.g., people, animals, objects).2 There are even more minor forms of visual hallucinations such as a sensation or perception of a presence (e.g., a person or animal standing behind them), a passage (e.g., a the sensation of a dog passing by) or an illusion (e.g., an actual object being seen as another object for a time, like a book momentarily appearing to be a bird).3
Minor visual hallucinations are transitory, and other hallucination episodes are typically short-lived; complex visual hallucinations usually last less than five minutes, can be static or kinetic and can occur any time throughout the day; most patients, even those with dementia, maintain understanding that these sightings are in fact hallucinations.3,4
Eyecare providers should be well-versed on Charles Bonnet syndrome (CBS), which involves complex visual hallucinations in cognitively sound individuals in the context of acquired visual impairment, but many are far less familiar with hallucinations in other settings.
Visual hallucinations in schizophrenia or other psychiatric disorders and in hallucinogen-induced states seem straightforward enough; but these stereotypical hallucinations—such as geometric patterns (e.g., checkerboard, cobwebs, tunnel, spiral) that reduplicate and/or change in size/shape or in object composition—also occur in non-psychiatric conditions such as epilepsy or narcolepsy, due to tumors or strokes involving the visual pathway, brainstem or thalamus, and even in normal individuals just before falling asleep.5,6
While the exact mechanisms of the dysfunctional visual information processing that produces visual hallucinations still eludes researchers, several areas along the visual pathway—spanning from the outer retina and optic nerve to the frontal, parietal and temporal cortices—have all been implicated.7 Irritation to any of these areas may be to blame for visual hallucinations, but the type of irritation can vary from photoreceptor dysfunction to inflammation or ischemia, compression, medications, recreational drugs or migraines, among others, depending on the visual hallucination-provoking disorder.8
In CBS, visual hallucinations have been attributed to a “release phenomenon” that occurs from deafferenation of the cerebral cortex’s visual association areas after acquired visual impairment causes defective visual input.6 While the precise source of the irritation leading to visual hallucination in the dementia spectrum is not well-defined, it is understood to be different than the release phenomenon in CBS. Much work remains to fully understand the pathophysiology of visual hallucinations in neurodegenerative disorders.
CBS should be touched on with every visually impaired patient since visual hallucinations in CBS occur in about 11% of people with severe vision loss, but don’t miss another broad demographic of patients at even higher risk: those on the dementia spectrum.9
Table 1. Visual Hallucination Types | |
Type | Examples |
| Minor | |
| Perception of a person/animal standing behind/nearby |
| Sensation of a person/animal passing by |
| One object briefly looking like another object |
| Simple | Photopsias, lines, dots, shapes, checkerboard |
| Complex | Formed images (people, animals, objects) |
Dementia Spectrum
The most common dementias include Alzheimer’s disease (AD), Parkinson’s disease with dementia (PDD) and dementia with Lewy bodies (DLB); classification of these diseases is very complex but largely boils down to which proteins are misfolded. Amyloid-β extracellular plaques and hyperphosphorylated tau proteins causing intracellular neurofibrillary tangles (NFT) are characteristic of AD, whereas PDD and DLB demonstrate α-synuclein deposition in Lewy bodies and neurites.1
Clinically, patients with AD typically have a form of cognitive impairment whose domains include memory, language and perceptual processing deficits.1 Parkinsonian motor dysfunction comprises typical features of Parkinson’s disease (PD) such as rigidity, bradykinesia, gait impairment and rest tremor.10 When cognitive function has become impaired enough that it affects social, occupational or basic activities of daily living, the criteria has been met to diagnose dementia.10 The prevalence of dementia in PD is up to 78%; mortality follows the dementia diagnosis by about four years, on average.10,11
Clinical features of PDD and DLB overlap and include cognitive difficulties chiefly involving attention, executive dysfunction, memory impairment and visuospatial abnormalities in the context of the parkinsonian motor dysfunction.1,10 PDD and DLB are differentiated from each other by the timing of whether parkinsonism or dementia develop first: those with parkinsonism who develop dementia less than one year after motor symptoms have PDD, whereas DLB includes those who develop dementia before parkinsonism or who develop dementia and parkinsonism within one year of each other.1,10
These patients—our patients on the dementia spectrum—need to hear from you about visual hallucinations. This phenomenon has been reported in up to 25% of those with AD.12 In early stages of AD, minor visual hallucinations are the much more prevalent type to occur, and they may begin quite early in the disease process; other visual hallucination forms are not likely in early AD but are associated with moderate AD and more severe AD dementia.4
In patients with PD, visual hallucinations are reported in about 16% to 40%—more so in those with PDD where they’re seen in up to 65%.3,13 Minor hallucinations are the most frequent hallucinatory symptom in PD.4 Interestingly, these minor visual hallucinations can also be experienced by patients—up to 30% of them—months to even several years before they develop any motor symptoms of PD.14 The main predictive factor for having visual hallucinations in treated PD patients is cognitive impairment; others include older age, duration of disease, depressive symptoms, sleep-wake cycle disturbances and more severely affected motor status.3,15 In PDD and DLB, complex hallucinations have been associated with increasing density and the distribution of Lewy bodies and NFTs in the temporal cortex in particular.16
Not surprisingly, complex visual hallucinations tend to worsen with time, both regarding frequency and severity, and are unfortunately a risk factor for dementia and a higher rate of mortality.17-19 Visual hallucinations are overwhelmingly common in DLB, where they occur in up to 80% of patients.20 In fact, recurrent complex visual hallucinations are one core diagnostic criteria for DLB and, along with early dementia, are a typical presenting feature of the disease.10 While illusions are also common in DBL, they are less specific than the complex hallucinations that are diagnostically helpful.10
Table 2. Visual hallucinations and Neuro Diseases | ||||
| Alzheimer’s Disease | Parkinson’s Disease | Parkinson’s Dementia | Dementia with Lewy Bodies | |
| Characteristic findings | Neurofibrillary tangles of amyloid-β extracellular plaques and hyperphysphorylated tau proteins | Lewy bodies and neurites with α-synuclein deposits | ||
| Parkinsonian motor dysfunction | ||||
| Dementia develops less than one year after motor symptoms | Dementia develops before motor symptoms or within one year of motor symptoms | |||
| Frequency of patients who have VH | Up to 25% | 16% to 40% | 65% | Up to 80% |
| Predominant VH type | Minor VH forms in early AD; other VH forms in later AD stages | Minor VH | Complex | |
| Temporal development and key features of VH | Minor VH may occur at the beginning of early AD stages | Up to 30% may have minor VH months to years prior to motor symptoms | Complex VH are a typical early presenting feature of DLB | |
Patient Inquiry
Visual hallucinations are under-reported by patients, likely for many reasons. Minor ones are often quickly dismissed by patients and are often not reported at all, largely because they may not be particularly bothersome. On the other hand, some patients may be afraid of stigma or have concern for cognitive decline when they experience a hallucination, so they may not share these symptoms with their healthcare providers. Because visual hallucinations can be quite complex and very well-formed, while surprisingly sometimes perceived as pleasant, they can also be very distressing to patients.
In one study of patients with minor visual hallucinations, they had been occurring for a mean duration of nearly one year and were not mentioned by the patients until they were explicitly asked.3 Other studies have similarly demonstrated that these patients do not volunteer experiencing them unless they’re prompted by leading questions or a direct inquiry.21 The bottom line is that we should be directly asking our at-risk patients—those on the dementia spectrum—if they have had any hallucinatory experiences.
Case One
An 80-year-old man presented, in part due to “floaters.” On further questioning about what they looked like, these were not vitreous floaters as I had expected; what he described as “floaters” was the sensation of a full-sized and -shaped person passing by on the right side (passage visual hallucination). They had been occurring about once per month over the past year.
He had no previous diagnosis of any form of neurodegenerative process. He denied tremors and couldn’t comment on gait changes such as shuffling, reduced arm swinging and rigidity because he couldn’t walk much due to other health issues. He denied any noticeable changes in cognition. His eye exam was non-contributory. His primary care physician was consulted and the patient was scheduled for an evaluation of his motor function, reflexes and cognition to evaluate for a correlating diagnosis; early PD would be highly suspected and early AD would also be a consideration.
Takeaways: (1) Ask good clarifying history questions to elicit what the patient is really trying to tell you—ask them to describe in detail what they mean so you hear what they’re communicating. (2) Minor visual hallucinations can precede motor symptoms in PD and can present early in AD—if a patient is reporting these hallucinations, recommend a further workup.
Discussion. While more formal interview templates are available regarding visual hallucinations, such as the North-East Visual Hallucinations Interview, eyecare clinicians can start with simple probing questions to classify any problem as relevant, such as onset, frequency, intensity and associated features; however, consider also asking about the complexity of the hallucination, and any associated thoughts, emotions and behaviors.2
Being empathetic to the patient’s experience by attentively listening and explaining what is occurring may provide emotional relief to the patient that there likely is a physiologic reason in addition to pointing them to additional help.
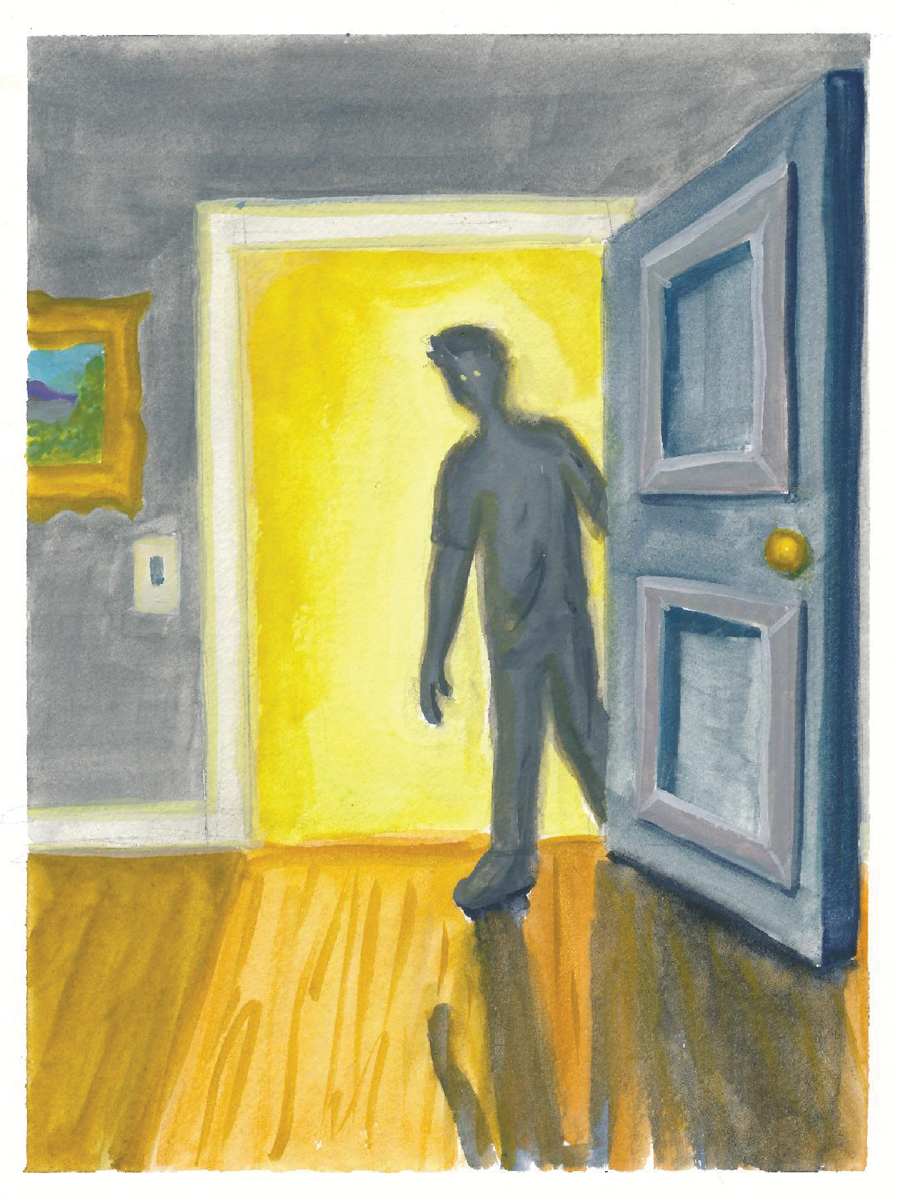 |
| When a patient experiences the minor visual hallucination known as presence, they often mistake shadows for people. Click image to enlarge. |
Case Two
A 74-year-old presented for a comprehensive exam. He had a history of treated PD, diagnosed 11 years prior, which was managed by neurology. When I asked him directly about visual hallucinations, he endorsed them. They had first started three years ago after an increase in Sinemet (carbidopa/levodopa, Merck) dosage, where he described thinking someone was sitting at a picnic table across the street but would then realize it was a garbage can (illusion). It occurred about weekly at first. He had told his neurologist about it at the time, and amantadine was started; the hallucinations were then only occasional.
However, in the past nine to 10 months prior to seeing me, he was seeing formed shapes and animals (complex visual hallucination) along with a more constant palinopsia that was noticeably worsening in complexity and frequency. He had seen two local optometrists in his hometown specifically regarding this but wasn’t given any insight as to what was happening, so he wasn’t even going to mention it. He also had developed worsening intense nightmares that were causing him to thrash quite violently in his sleep. I discussed the hallucination in the context of PD with him and his wife and consulted with his neurologist who decreased his Sinemet dosage.
Initially, he did feel the change helped with lessening the frequency of the hallucination during the day; however, months later they were again worsening and had progressed to very frequent, more complex and very troublesome. He also noticed more illusions: “I can turn the chair into a bear or the computer screen into a hat.” Because of this, he stopped driving. Additionally, his sleep symptoms were continuing to worsen, so much so that he feared for his wife’s safety.
Amantadine was then stopped by his neurologist. Six months later, his daytime visual hallucinations had improved, but he would still occasionally misinterpret shadows as people and see illusions out of his window, such as park benches. Overall, this was a welcomed improvement. Meanwhile, however, his sleep symptoms had become more violent and severe. Next, mirtazapine was stopped, melatonin was increased and an updated consult with Sleep Medicine was ordered due to the REM sleep behavior disorder. This change in medication did further improve his daytime visual hallucinations, and perhaps lessened the frequency but not intensity of his RBD. By the next six-month interval with neurology, he was demonstrating increased irritability, anger, frustration and confusion in the evenings. Donepezil was added, and continued management is ongoing.
Takeaways: (1) He asked two eye doctors about his visual hallucinations and wasn’t given an answer—don’t be that doctor. (2) He didn’t volunteer to me that he had experienced hallucinations but told me all about them when I asked—so, ask! (3) Visual hallucinations can be very troublesome to patients, both emotionally and functionally—they led this patient to stop driving. (4) Medication changes can help, but it’s tricky to balance motor function symptoms, hallucinations, REM sleep behavior disorder and more—be sure to direct these patients to neurology for medication management and share salient information such as details and duration of patient-reported symptoms and relevant exam findings. (5) Complex visual hallucinations tend to worsen, and are a risk factor for dementia—this case developed functional changes in mood and mental status about two years after the onset of worsening complex visual hallucinations.
Discussion. How I tend to approach this clinically in patients with known AD, PD, PDD or DLB is first by offering basic information about visual hallucinations in these conditions, then asking if they have experienced the phenomenon. It might sound something like this:
“I see that you have Parkinson’s. Interestingly, a high percentage of these patients eventually develop what’s called visual hallucinations, which means seeing or perceiving things that aren’t actually there. Sometimes these are more shadow-like shapes or patterns in the vision, or sometimes even just a sensation or feeling like someone is standing near you or passing by you, but isn’t really there; however, sometimes they can become quite complex and realistic, like animals or people. There are medications available that may help if these develop. Have you ever experienced anything like this?”
You might just be surprised by what you hear, and how often you hear it.
 |
|
Complex hallucinations involve formed images and can occur any time throughout the day. Click image to enlarge. |
Case Three
A 74-year-old male presented who had a history of symptoms including mild tremors, urinary incontinence, gait instability and cognitive impairment. Two years prior, after neuropsychological testing, neurology felt these symptoms were likely independent with multifactorial etiologies, not indicative of a neurodegenerative process at the time; however, about one year later, he developed visual hallucinations.
These initially presented only upon awakening when he’d see spiders on the nearby wall. He even would get out of bed and try to hit them before realizing they were not there. They only happened in that setting and would last about 60 to 90 seconds.
At that point, with relatively early development of complex visual hallucinations, his symptom constellation became particularly concerning for DLB so carbidopa/levodopa was started. I saw him about a year later, and when I inquired about his hallucinations, he said he had been seeing “like a mouse or a squirrel in my house. I went after it and got it into the corner, but it wasn’t even there. I see mice and stuff like that, and it’s not there at all. Sometimes I see a spider that is not even there.” The squirrels and mice were full-sized and very realistic appearing, and the spiders were the diameter of a cup. Because he saw them so often, he was no longer reacting to them. He continues to follow with neurology for management but was very grateful for the information and reassurance that these hallucinations are common in the context of DLB.
Takeaways: (1) Visual hallucinations are a helpful symptom diagnostically—in this case, it finally allowed the neurologist to connect the symptom constellation into a unifying diagnosis. (2) Patients appreciate compassionate listening, information and reassurance about what they are experiencing.
Management
As there have been no large-scale studies regarding treatment for visual hallucinations, case report, anecdotal and consensus literature are relied upon.5 It is definitely not one-size-fits-all, and response to various medication classes varies from patient to patient, and depending on its cause.5 Dopamine replacement medications may precipitate or exacerbate hallucinations, but dose adjustments or medication class changes can often help.10
Various abnormalities on office-based tests such as electroretinogram (ERG), visual evoked potential (VEP) and optical coherence tomography (OCT) have been demonstrated in certain subsets of this population, but these abnormalities have not yet proven to be diagnostic or specific to the dementia spectrum, so are of limited utility—and are not routinely recommended as of now in dementia spectrum patients.13,22,23 In addition to a comprehensive dilated eye exam, ERG, VEP, OCT and visual field testing may be relevant to evaluate for clues that may point to or help rule out other sources of visual hallucinations.
Takeaways
Optometrists should be asking about symptoms of visual hallucinations and educating all patients on the dementia spectrum about the possibility. Preemptively educating patients about this possibility can soothe a lot of surprise and fear if and when they do develop and lets them know that treatments do exist. I would challenge you to ask—and educate—every patient (and/or their caregivers) who has a relevant medical history concerning visual hallucinations.
Dr. Weidmayer practices at the LTC Charles S. Kettles Medical Center, VA Ann Arbor Healthcare System in Ann Arbor, MI. She is also a clinical assistant professor for the Department of Ophthalmology and Visual Sciences, WK Kellogg Eye Center of the University of Michigan.
Dr. McDowell is chief of pediatrics, pediatric residency supervisor and professor at Michigan College of Optometry at Ferris State University in Big Rapids, MI. She is an avid painter in her free time. They have no financial disclosures.
1. Wilson H, Pagano G, Politis M. Dementia spectrum disorders: lessons learnt from decades with PET research. J Neural Transmission. 2019;126:233-51. 2. Mosimann UP, Collerton D, Dudley R, et al. A semi-structured interview to assess visual hallucinations in older people. Int J Geriatr Psychiatry. 2008;23(7):712-18. 3. Fénelon G, Mahieux F, Huon R, Ziégler M. Hallucinations in Parkinson’s disease: Prevalence, phenomenology and risk factors. Brain. 2000;123(4):733-45. 4. Ruiz M, Arias A, Sanchez-Llanos E, Gil MP, et al. Minor Hallucinations in Alzheimer’s Disease. J Alzheimer’s Disease. 2018;64:543-9. 5. ffytche DH. Visual hallucinatory syndromes: past, present, future. Dialogues Clin Neurosci. 2007;9(2):173-89. 6. Manford M, Andermann F. Complex visual hallucinations. Clinical and neurobiological insights. Brain. 1998;121(Pt 10):1819-40. 7. Kurita A, Koshikawa H, Akiba T, Seki K, et al. Visual hallucinations and impaired conscious visual perception in Parkinson disease. J Geriatr Psychiatry Neurol. 2020;33(6):377-85. 8. Trobe J. Neuro-ophthalmology at your fingertips. Visual Hallucinations. fingertips.neuro-ophthalmology.med.umich.edu/visual_hallucinations/visual_hallucinations.html. Accessed March 17, 2022. 9. Teunisse RJ, Cruysbert JR, Hoefnagels WH, Verbeek AL, et al. Visual hallucinations in psychologically normal people: Charles Bonnet’s syndrome. Lancet. 1996;347(9004):794-7. 10. Gomperts SN. Lewy body dementias: dementia with Lewy bodies and Parkinson disease dementia. Continuum. 2016 Apr;22(2Dementia):435-63. 11. Kempster PA, O’Sullivan SS, Holton JL, et al. Relationships between age and late progression of Parkinson’s disease: a clinic-pathological study. Brain. 2010;133(pt6):1755-62. 12. Ballard C, Holmes C, McKeith I, Neill D, et al. Psychiatric morbidity in dementia with Lewy bodies: a prospective clinical and neuropathological comparative study with Alzheimer’s disease. Am J Psychiatry. 1999; 156(7):1039-45. 13. Murphy N, Killen A, Gupta RK, Graziadio S, et al. Exploring bottom-up visual processing and visual hallucinations in Parkinson’s disease with dementia. Front Neurol. 2021 Jan 28;11:579113. 14. Pagonabarrage J, Martinez-Horta S, de Bobadilla RF, et al. Minor hallucinations occur in drug-naïve Parkinson’s disease patients, even from the premotor phase. Mov Disord. 2016;31(1):45-52. 15. Merims D, Shabtai H, Korczyn AD, Peretz C, et al. Antiparkinsonian medication is not a risk factor for the development of hallucinations in Parkinson’s disease. J Neural Transm (Vienna). 2004;111(10-11):1447-53. 16. Harding AJ, Broe GA, Halliday GM. Visual hallucinations in Lewy body disease relate to Lewy bodies in the temporal lobe. Brain. 2002;125:391–403. 17. Goetz CG, Fan W, Leurgans S, Bernard B, et al. The malignant course of “benign hallucinations” in Parkinson disease. Arch Neurol. 2006;63(5):713-6. 18. Goetz CG, Stebbins GT. Mortality and hallucinations in nursing home patients with advanced Parkinson’s disease. Neurology. 1995;45(4):669-71. 19. Hobson P, Meara J. Risk and incidence of dementia in a cohort of older subjects with Parkinson’s disease in the United Kingdom. Mov Disord. 2004;19(9):1043-9. 20. McKeith IG, Boeve BF, Dickson DW, Halliday G, et al. Diagnosis and management of dementia with Lewy bodies: Fourth consensus report of the DLB Consortium. Neurology. 2017;89(1):88-100. 21. Menon GJ. Complex visual hallucinations in the visually impaired: a structured history-taking approach. Arch Ophthalmol. 2005;123(3):349-55. 22. Devos D, Tir M, Maurage CA, Waucquier N, et al. ERG and anatomical abnormalities suggesting retinopathy in dementia with Lewy bodies. Neurology. 2005;65:7. 23. Lee J-Y, Kim JM, Ahn J, Kim HJ, et al. Retinal nerve fiber layer thickness and visual hallucinations in Parkinson’s disease. Mov Disord. 2014;29(1):61-7. |

