 |
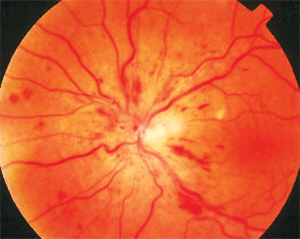
| Complete PVD may be protective against neovascularization in eyes with ischemic CRVO. Photo: Joseph W. Sowka, OD, and Alan G. Kabat, OD. Click image to enlarge. |
The vitreomacular interface is known to have important implications in the manifestations of retinal disease processes including retinal vein occlusion. Prior studies evaluating the influence of posterior vitreous detachment (PVD) status in central retinal vein occlusion (CRVO) on retinal neovascularization in CRVO have suggested that complete PVD may be protective against neovascularization in eyes with ischemic CRVO. A recent study published in Retina has determined that cases of CRVO with complete PVD had significantly lower rate of cystoid macular edema (CME), lower central subfield thickness (CST) and lower anti-VEGF injection burden at one year.
The retrospective longitudinal cohort study assessed patients with acute, treatment-naïve CRVO diagnosed who had at least 12 months of follow-up. Clinical characteristics, treatment patterns and outcomes were analyzed between eyes stratified based on presence or absence of a complete PVD on OCT at presentation.
Of the 102 acute, treatment-naïve CRVOs identified, 52 (51%) had complete PVD at presentation and 50 (49%) did not. CST was significantly lower in those with complete PVD (12 months: 284.9μm vs 426.8μm; last follow-up: 278µm vs 372.8μm. One-year intravitreal injection burden was significantly less for those with a complete PVD than those without (5.1 injections vs 6.7 injections). At 12 months, those with complete PVD at presentation had significantly less CME than those with incomplete PVD at presentation (32% vs 65%).
“We suspect that the vitreous may serve as a reservoir and microenvironment for pro-inflammatory cytokines and molecules present in eyes with retinal vein occlusion,” the researchers wrote in their paper. “The presence of a complete PVD in eyes with CRVO contributes to reduced levels of locally circulating pro-inflammatory molecules at the vitreomacular interface, as has been demonstrated in eyes with diabetic retinopathy.”
They concluded that, “Assessment of the vitreomacular relationship on OCT at presentation in eyes with CRVO may serve as a prognostic imaging biomarker.”
Zheng Y, Woodward R, Feng HL, et al. Implications of complete posterior vitreous detachment in eyes with central retinal vein occlusion. Retina. September 5, 2023. [Epub ahead of print]. |

