 |
A 49-year-old Hispanic male first presented with complaints of blurred vision in his left eye during a telemedicine exam. He also reported a few months earlier seeing “broken glass,” or what looked like colored crystals, in his vision in the same eye, which was accompanied by tingling on the left side of his body.
Nothing was seen during the exam but, given his symptoms and history of blurred vision, it was recommended that he come in for an in-person visit the following week, where he underwent a comprehensive eye exam and reaffirmed he thought vision in his left eye was slightly blurry.
His medical history was significant for hypertension and high blood sugar but reported that he is on a vegan diet and lost over 20 pounds. His blood pressure is under control and he takes lisinopril.
Upon exam, his uncorrected distance visual acuities measured 20/20 in each eye. Confrontation visual fields were full to careful counting OU. His pupils were equally round and reactive to light; there was no afferent pupillary defect. His extraocular motility was full and cover test was ortho at distance. His anterior segments and intraocular pressures were unremarkable.
On dilated fundus exam, the vitreous in both eyes was clear. He had small cups with good rim coloration and perfusion in each eye. The fundus exam findings of the right eye were completely normal. In the left eye, there were obvious changes of note (Figure 1). Fundus photos, OCT and OCT-A were obtained of the macula and peripheral retina.
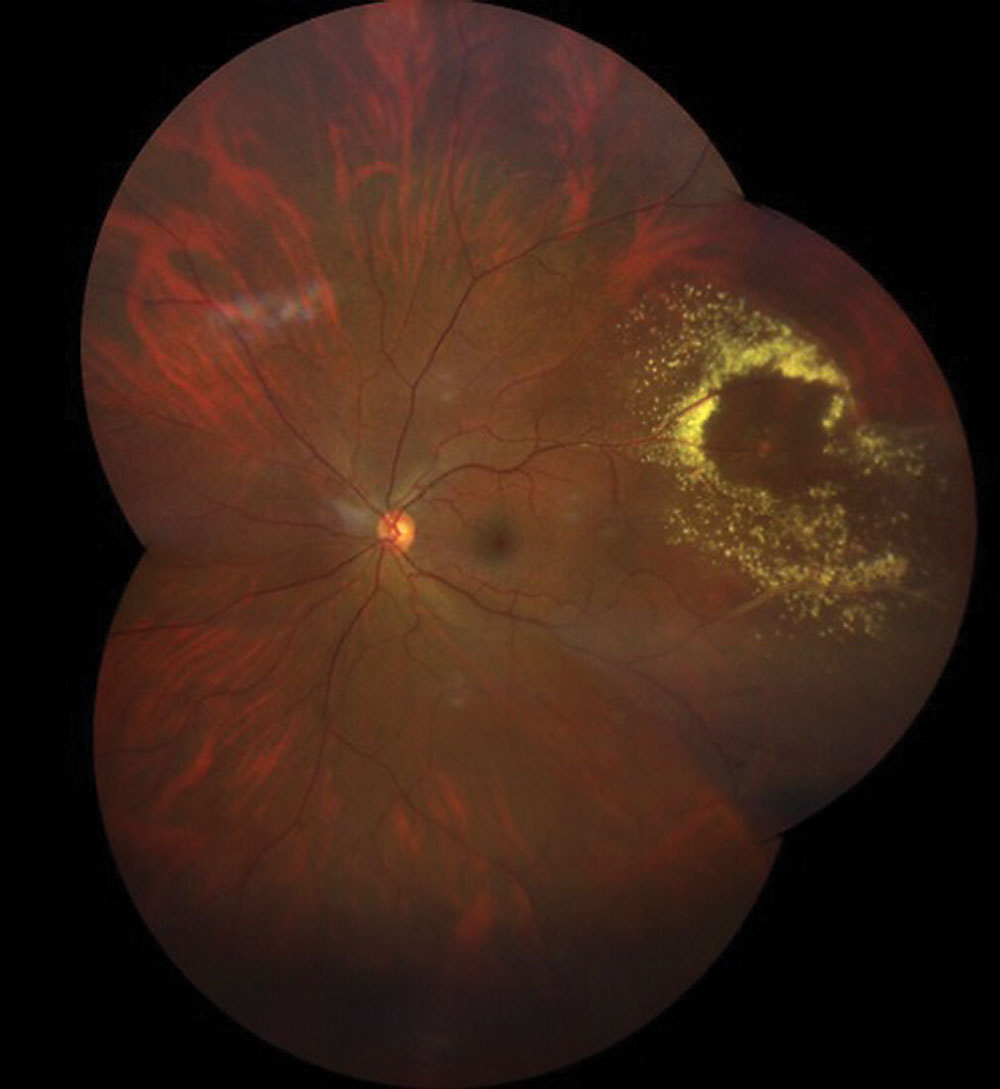 |
Fig. 1. A widfield fundus image of the retina in the patient. What is the diagnosis? Click image to enlarge. |
Take the Retina Quiz
1. What is the most likely diagnosis?
a. Congenital retinal telangiectasis, Type 1.
b. Peripheral choroidal neovascularization.
c. Coats disease.
d. Retinal arterial microaneurysm (RAM).
2. How should this patient be managed?
a. Observation.
b. Focal laser.
c. Anti-VEGF injection.
d. Either B or C.
3. What is the most common underlying condition?
a. Congenital vascular incompetency.
b. Diabetes.
c. Hypertension
d. Hyperlipidemia.
4. Which statement is most accurate for this condition?
a. Mainly develops from dysfunction within the superficial capillary network.
b. Develops from dysfunction with the venous system.
c. Develops from dysfunction of the arterial system.
d. Develops subretinally from increased VEGF expression.
5. Which patient is more likely to develop this condition?
a. Young males
b. Young females.
c. Middle-aged males.
d. Elderly females.
For answers, see below.
Diagnosis
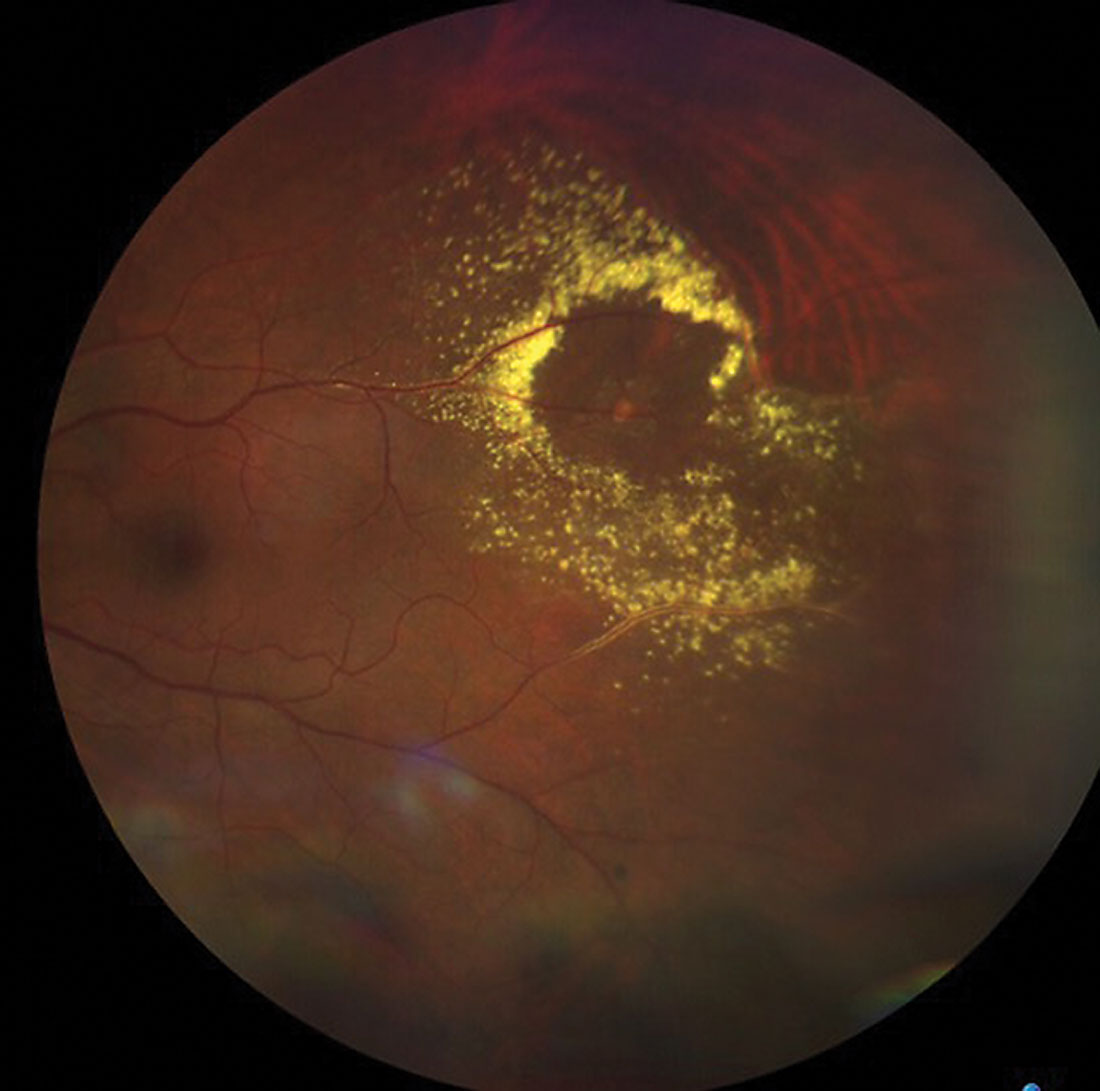
It was a surprise to discover a large area of circinate exudate superotemporally in the left eye of this patient. Within the center of the exudate, there is a yellow-white oval lesion that involves one of the branches of either the central retinal vein or central retinal artery, but which is it? At initial inspection, it looks like the central lesion is from one of the retinal veins, as there is significant sheathing of the veins above and below the lesion. But if you look more closely and follow the lesion back, it actually involves one of the branches of a retinal artery. Indeed, this is a retinal arterial microaneurysm (RAM).
Discussion
RAM represents a focal aneurysmal dilatation of one of the branches of the central retinal artery and usually occurs within the first three bifurcations of the arterial system or at an arteriovenous crossing. It most commonly takes place in the superotemporal quadrant, as was seen in our patient. RAM has a predilection for elderly hypertensive females, but also occurs in males, as also was seen in our patient. It is typically seen as a single isolated finding, but multiple RAMs can be seen in about 20% of patients.1
The pathophysiology of RAM is not well understood, but the underlying theme is hypertension and atherosclerotic disease. With aging, there is atrophy of the muscularis layers of the arteries that leads to thinning, fibrosis and loss of elasticity within the artery. With chronic hypertension, there is an increase in luminal pressure within the walls of the arteries that can lead to an increased susceptibility for these aneurysmal dilations.2 It’s also postulated that damage can occur in the endothelium of the arteries from emboli, which can weaken the vessel walls and be more susceptible to aneurysm formation.3
RAM generally takes on three forms: quiescent, hemorrhagic and exudative.4 The quiescent RAM is found during a routine exam in which an aneurysmal dilation of the retinal artery is discovered without any exudation and hemorrhage. It rarely causes any visual dysfunction and can be monitored without treatment.
In the hemorrhagic form, RAM has ruptured and there can be multilayered hemorrhaging that involves the intraretinal and subretinal space, but can also be in the vitreous as well as preretinal and/or intraretinal layers. This is due to the fact that arteries are high-flow vessels, and when one ruptures, it does so under significant pressure, which can push blood into multiple layers of the retina. If there is extensive hemorrhage, a RAM diagnosis may be difficult to establish if the hemorrhage obscures the RAM. In these instances, imaging becomes important in helping to make a definitive diagnosis.
In the exudative form, a circinate pattern of exudate may surround the lesion, as seen with our patient. With the accumulation of exudate, intraretinal edema can occur. Depending on the location of the fluid, vision loss may also occur if it involves the macula.
Our patient had extensive circinate exudate and it was clear there was retinal thickening and intraretinal fluid, but because it was in the peripheral retina, the fluid had not moved posteriorly and the macula and vision were not affected.
 |
|
Fig. 2. Take a closer look at the area of interest. Which blood supply is most affected? Click image to enlarge. |
Testing and Treatment
Ancillary testing can be helpful in establishing a diagnosis of RAM. Widefield fluorescein angiography will show early hyperfluorescence of the aneurysmal dilation as it fills up uniformly in the early phase of the angiogram, making this the preferred diagnostic test of choice. There may be areas of blocked fluorescence if overlying blood is obscuring the RAM. We did not perform widefield angiography in our patient as was felt the diagnosis was easily made based on our clinical exam. We tried to obtain OCT-A but were not able to get good scans of the RAM. An OCT of the macula was performed as a baseline and to establish the absence of macular involvement.
The natural history of RAM is spontaneous involution of the aneurysmal dilation. Therefore, peripheral lesions that do not involve or threaten the macula can be observed at one- to three-month intervals.
In instances where vision is affected, either because of macular edema or vitreous hemorrhage, treatment is recommended. Argon laser photocoagulation can be applied directly to the RAM, but care must be taken to avoid rupture. The laser is applied with low power, long burn duration and a large spot size.2 Indirect laser can also be used with the hope of reducing the oxygen consumption and blood flow to the RAM, which in turn would lower the amount of exudation from the RAM to the surrounding retina.
Finally, anti-VEGF injections can be used when macular edema is present in a similar fashion to injections that are routinely performed for other causes of macular edema. In the setting of a vitreous hemorrhage, pars plana vitrectomy may be indicated.
Fortunately, visual function was not affected in this patient. It is difficult to correlate his original symptoms of seeing broken glass or colored crystals two months earlier with the RAM, but it can’t be just a coincidence. During a follow-up a few months later, his vision still remained 20/20, but there was even more exudation and retinal edema in the same location. For that reason, he was advised to see a retina subspecialist on the next follow-up visit in two to three months.
Retina Quiz Answers
1) d; 2) a; 3) c; 4) c; 5: d
Dr. Dunbar is the director of optometric services and optometry residency supervisor at the Bascom Palmer Eye Institute at the University of Miami. He is a founding member of the Optometric Glaucoma Society and the Optometric Retina Society. Dr. Dunbar is a consultant for Carl Zeiss Meditec, Allergan, Regeneron and Genentech.
| 1. Robertson DM. Macroaneurysms of the retinal arteries. Trans Am Acad Ophthalmol Otolaryngol. 1973;77(1):55–67. 2. Ng, WY, Mathur R, Shu D. Diagnosis and management of retinal arterial macroaneurysm. Eyenet Magazine. June 2018. 3. Speilburg, A, Klemencic SA. Ruptured retinal arterial macroaneurysm: diagnosis and management. J Optom. 2014;7(3):131-7. 4. Lavin MJ, Marsh RJ, Peart S, Rehman A. Retinal arterial macroaneurysms: a retrospective study of 40 patients. Br J Ophthalmol. 1987;71(11):817-25. |

