 |
A 74-year-old Hispanic male presented with acute onset new red spots, “web-like” floaters and blurred vision in his left eye for five days. Past medical history included hypertension, hyperlipidemia and atrial fibrillation that were controlled with metoprolol, dofetilide, apixaban, telmisartan, atorvastatin and spironolactone. His ocular, social and family histories were unremarkable, and he denied history of trauma.
Acuity was 20/40 OD and 20/150 OS. Extraocular motilities were full, confrontation fields were full and there was no relative afferent pupillary defect. IOP was 15mm Hg OD and 11mm Hg OS. Anterior segment exam revealed 3+ nuclear sclerotic cataracts OU.
Take the Retina Quiz
1. Which of the following is true of the inferotemporal lesion in the right eye?
a. It is a choroidal effusion.
b. It is a choroidal hemangioma.
c. It is a retinal detachment.
d. It is a retinoschisis.
2. How would you interpret the B-scan of the left eye?
a. There is a full-thickness macular hole.
b. There is a retinal detachment.
c. There is an epiretinal membrane.
d. There is an inner retinal hole.
3. What is the appropriate management for the left eye?
a. Close observation.
b. Intravitreal anti-VEGF injection.
c. Laser retinopexy.
d. Pars plana vitrectomy.
4. Which of the following is a potential complication of this patient’s condition?
a. Glaucoma.
b. Irregular astigmatism.
c. Macular degeneration.
d. Retinal detachment.
5. Which of these is true regarding prognosis?
a. There is a high risk of progression to retinal detachment in the right eye.
b. There is a high risk of progression to retinal detachment in the left eye.
c. There is a low risk of progression to retinal detachment in the left eye.
d. Risk of retinal detachment is the same for inner retinal breaks as well as combined inner and outer retinal breaks.
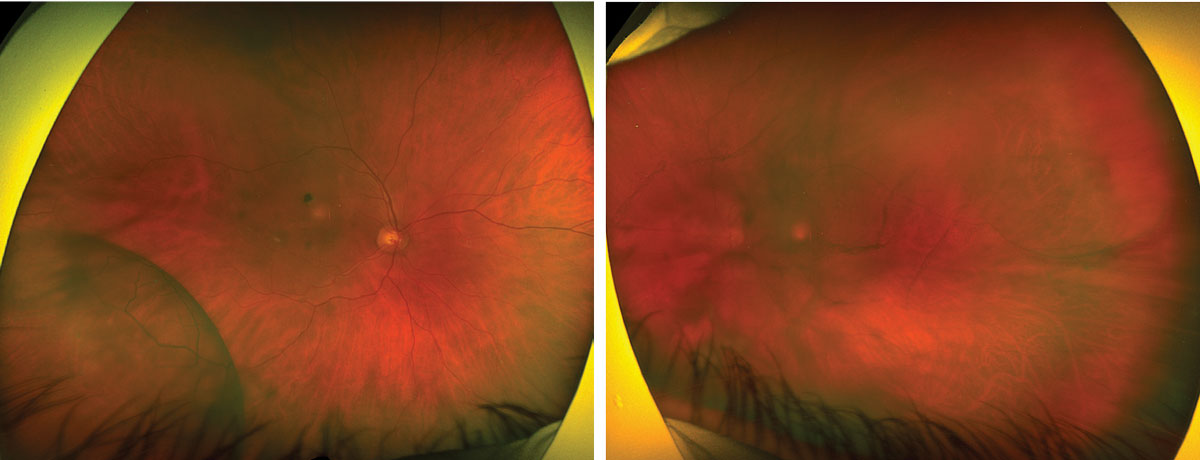 |
| Figs. 1 and 2. Optos widefield fundus photography of the right eye (left) and left eye (right). Click image to enlarge. |
Diagnosis
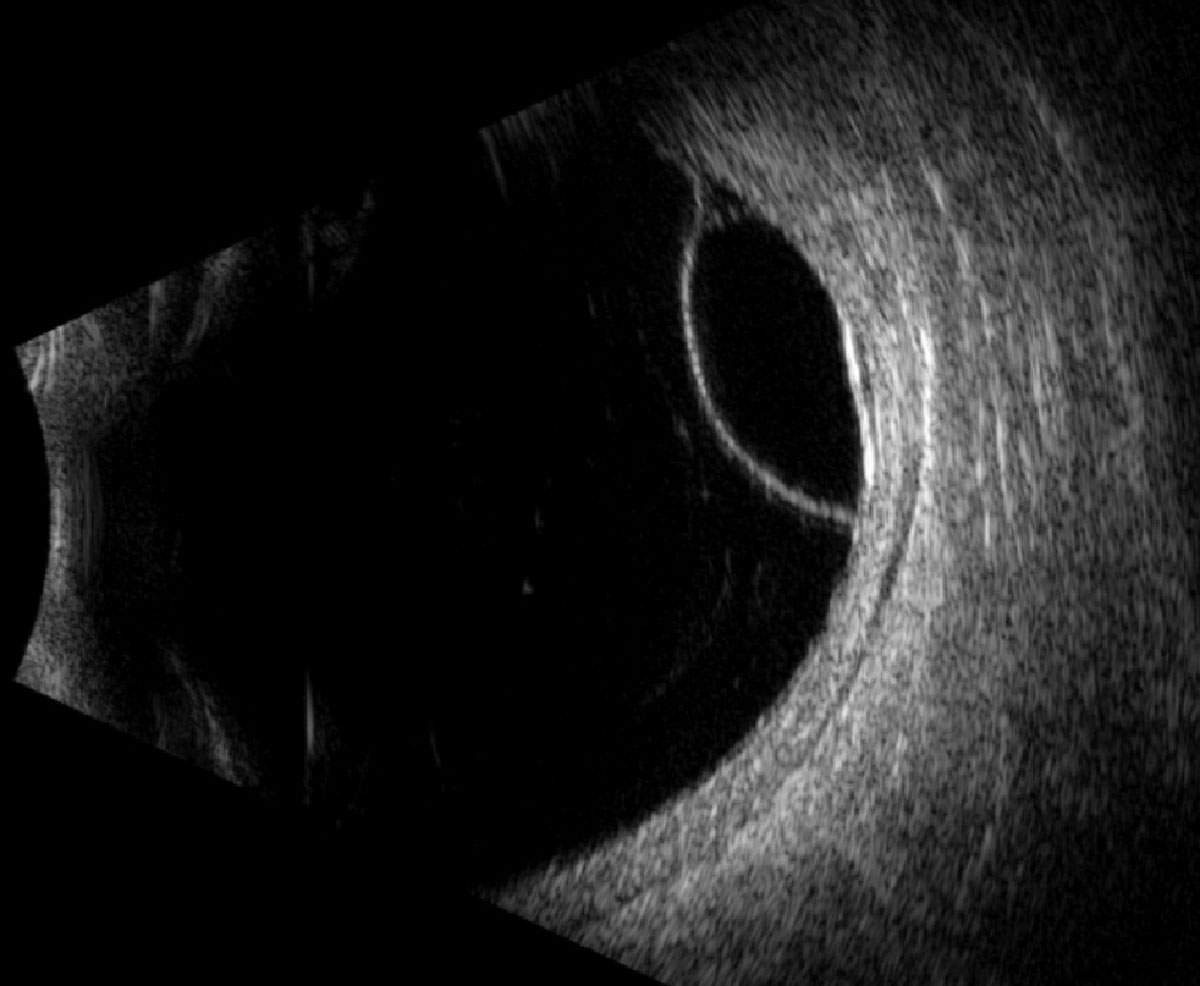
Fundus exam revealed a posterior vitreous detachment (PVD), macular scar and inferotemporal retinoschisis OD, and a vitreous hemorrhage and superotemporal retinoschisis OS (Figures 1 and 2). B-scan ultrasound confirmed the retinoschisis OU and identified a focal inner-retinal hole within the retinoschisis cavity OS that was otherwise challenging to locate on clinical exam due to presence of a vitreous hemorrhage (Figures 3 and 4).
Retinoschisis was diagnosed OU, and the vitreous hemorrhage OS was presumed secondary to a hemorrhagic PVD that created vitreoretinal traction and ultimately an inner-retinal hole within the superotemporal schisis pocket. Close observation was elected with serial dilated fundus exams and B-scans to rule out new retinal breaks, expansion of the schisis cavity or progression to combined retinoschisis and retinal detachment.
Discussion
Retinoschisis is defined as a splitting of the retina most commonly at the level of the outer plexiform layer; it can also occur at the level of the nerve fiber layer.1-3 Juvenile (X-linked) retinoschisis is inherited and the most common cause of juvenile macular degeneration in males, as it presents with a foveal schisis.4,5 Peripheral, degenerative (also known as acquired, senile) retinoschisis is typically found in middle-aged individuals with an incidence of 1% to 3.7% of adult patients and up to 7% of patients over the age of 40.5,6 It is most frequently bilateral (40% to 82% of patients) with a predilection for the inferotemporal quadrant (72%), and can expand posterior to the equator in up to 42% of patients.1,2,5,6 There is no sex predilection, and there is a trend towards hyperopic refractive error.2,6
This condition is typically seen as a round/ovoid, transparent, immobile, flat (typical) or dome-shaped (reticular), smooth bullous elevation involving the inferotemporal quadrant.1,2,6,7 The thin inner walls of a schisis cavity often contain retinal vessels that take on an attenuated or sheathed appearance.5 Nearly all retinoschises are anteriorly continuous with or begin just posterior to the ora serrata, and are delineated by cystoid degeneration at their posterior margins.5,6
It is crucial to differentiate retinoschisis from other conditions, including retinal detachment, combined retinoschisis-detachment, choroidal effusion and choroidal malignancy (e.g., melanoma). Unlike retinoschisis, retinal detachments are more opaque, mobile, have a corrugated/wrinkled surface and tend to produce a relative, rather than absolute, scotoma.1,5,6
 |
|
Fig. 3. Longitudinal B-scan of the right globe along the 7:30 meridian. Click image to enlarge. |
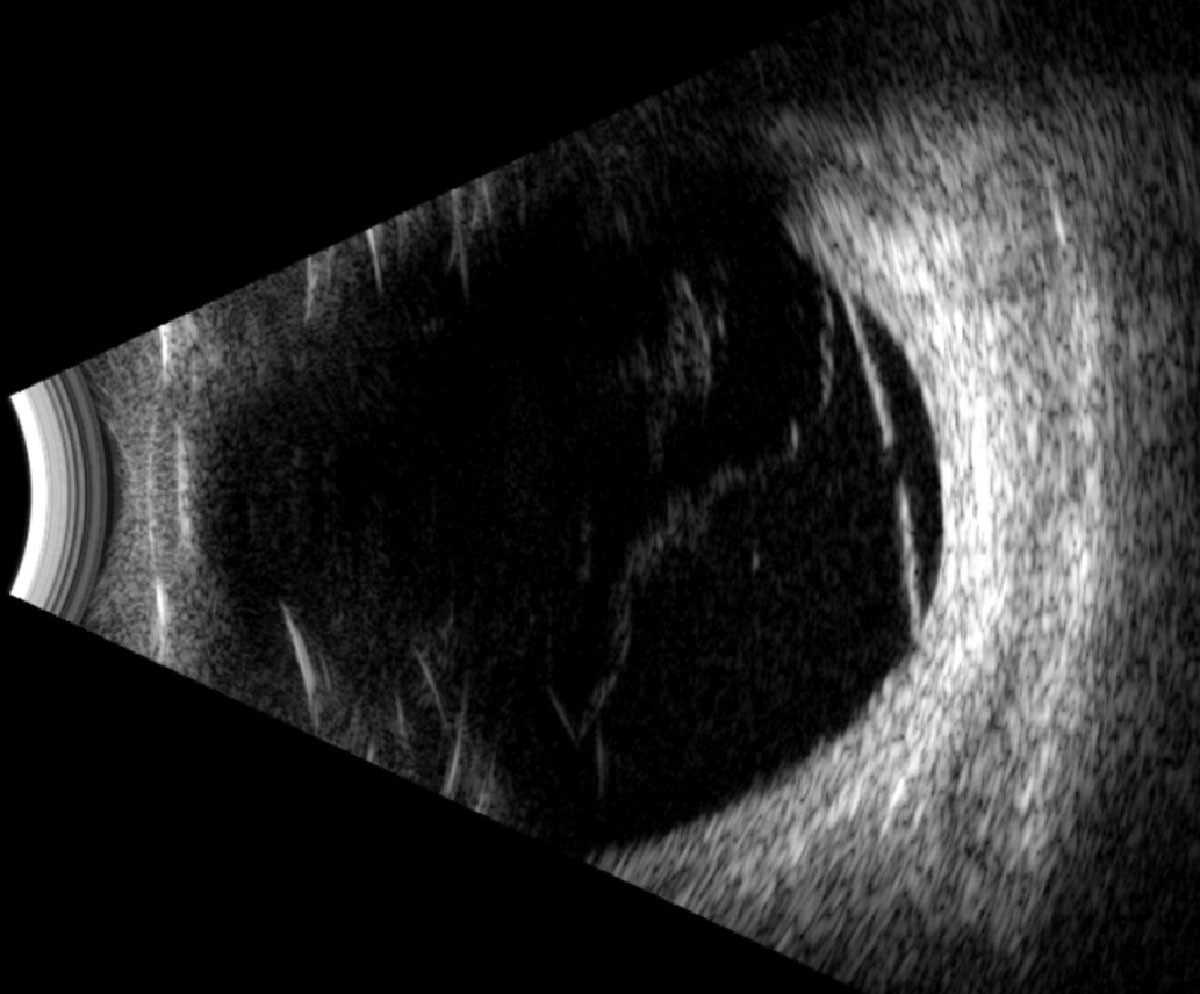 |
Fig. 4. Longitudinal B-scan of the left globe along the 1:30 meridian. Click image to enlarge. |
Prognosis and Treatment
Retinoschisis is asymptomatic and often remains stable in the absence of intervention.8 Observation is indicated to monitor for progressive enlargement of the schisis, development of inner and/or outer wall breaks and evolution to combined retinoschisis-detachment.8 Schisis cavities may enlarge laterally (6%), vertically (5%) and posteriorly (3%) toward the macula, but in a series of 218 eyes, none progressed to macular involvement over an average of nine years.7,8
Inner retinal breaks are less common than outer retinal breaks and are seen in up to 4% and 17% to 23% of retinoschisis, respectively.9 Outer retinal breaks create a direct communication with the schisis cavity and the subretinal space that can lead to retinal detachments; those associated with outer wall breaks tend to be localized, asymptomatic and nonprogressive, therefore infrequently requiring intervention.8,9
Progressive and symptomatic retinal detachments in the setting of retinoschisis are most common in patients with retinal breaks in the inner and outer schisis walls, allowing a direct communication between the vitreous cavity, schisis cavity and subretinal space, though there are cases of progressive retinal detachments related to large outer retinal breaks.8,9 Progressive combined retinoschisis-detachments necessitate prompt intervention to stabilize or repair the retinal detachment, depending on the extent.8,9
Prognosis is favorable as many retinoschisis patients retain baseline visual acuity. Treatment is seldom necessary for isolated retinoschisis irrespective of the presence or absence of retinal breaks.8 However, swift intervention is needed when progressive combined retinoschisis-detachments occur.8 Retinoschisis with localized detachment should be monitored closely for progression; intervention should be at the discretion of a retinal specialist.8 It is worth noting that retinoschisis cavities may occasionally undergo spontaneous collapse and regression.3,8
Our patient was observed with serial dilated fundus and scleral depressed exams every two weeks until the vitreous hemorrhage cleared, at which point appointments were extended. He ultimately underwent cataract surgery in both eyes after three months of stability following the resolution of vitreous hemorrhage and achieved final acuity of 20/20 OD and OS.
Retina Quiz Answers
1: d, 2: d, 3: a, 4: d, 5: c
Dr. Aboumourad currently practices at Bascom Palmer Eye Institute in Miami. Neither has any financial disclosures.
Dr. Dunbar is the director of optometric services and optometry residency supervisor at the Bascom Palmer Eye Institute at the University of Miami. He is a founding member of the Optometric Glaucoma Society and the Optometric Retina Society. Dr. Dunbar is a consultant for Carl Zeiss Meditec, Allergan, Regeneron and Genentech.
1. Ryan SJ, Davis JL, Flynn HW, et al. Retina, Fifth ed. London; New York: Saunders/Elsevier, 2013. 2. Thanos A, Todorich B, Pasadhika S, et al. Degenerative peripheral retinoschisis: observations from ultra-widefield fundus imaging. Ophthalmic Surg Lasers Imaging Retina. 2019;50(9):557-64. 3. Agarwal A, Gass JDM. Gass’ Atlas of Macular Diseases, Fifth ed. London: Elsevier, 2011. 4. Sikkink SK, Biswas S, Parry NR, et al. X-linked retinoschisis: an update. J Med Genet 2007;44(4):225-32. 5. Straatsma BR. Clinical features of degenerative retinoschisis. Aust J Ophthalmol. 1980;8(3):201-6. 6. Byer NE. Clinical study of senile retinoschisis. Arch Ophthalmol 1968;79(1):36-44. 7. Byer NE. Long-term natural history study of senile retinoschisis with implications for management. Ophthalmology. 1986;93(9):1127-37. 8. Byer NE. Perspectives on the management of the complications of senile retinoschisis. Eye. 2002;16(4):359-64. 9. Lewis H. Peripheral retinal degenerations and the risk of retinal detachment. Am J Ophthalmol. 2003;136(1):155-60. |

