 |
A 21-year-old Hispanic male presented with increasing redness, pain and blurred vision in the right eye. His review of systems was unrevealing, and he denied any similar prior episodes. His medical, ocular, social and family histories were all unremarkable. He denied any history of trauma or substance abuse.
His visual acuity (VA) was 20/40 OD and 20/20 OS. Extraocular motilities and confrontation visual fields were full OU. His pupils were equally round and reactive in both eyes, and there was no relative afferent pupillary defect; color vision was full OU. Intraocular pressure was 13mm Hg OD and 15mm Hg OS by applanation. Anterior segment exam revealed 3+ sectoral temporal injection of deep scleral vascular plexus OD without any corneal involvement, anterior chamber cell or flare or vitritis. There were no signs of inflammation OS. Furthermore, there was significant tenderness to palpation of the right globe and pain with lateral eye movements. Posterior segment findings can be seen below.
 |
|
Fig. 1. Optos widefield fundus photography of the right eye at presentation. Click image to enlarge. |
Take the Retina Quiz
1. How would you interpret the OCT findings of the right eye?
a. There are vitreous cells.
b. There is intraretinal fluid.
c. There is subretinal fluid.
d. There is a choroidal effusion.
2. How would you interpret the B-scan ultrasound?
a. There is a retinal detachment.
b. There is myositis.
c. There is infilitration of Tenon’s capsule and accumulation of sub-Tenon fluid.
d. All of the above are true.
3. What is the most likely diagnosis?
a. Central serous retinopathy.
b. Posterior scleritis or panscleritis.
c. Purtscher retinopathy.
d. Vogt-Koyanagi-Harada disease.
4. All of the following may accompany this disease at presentation except?
a. Ocular hypertension.
b. Orbital myositis.
c. Retinal detachment.
d. Severe vitritis.
5. Which of the following regarding prognosis is false?
a. There is an increased risk of mortality when scleral necrosis is present.
b. Vision loss is most frequently secondary to rhegmatogenous retinal detachments.
c. With prompt identification and treatment, vision loss may be limited to less than two lines of Snellen visual acuity.
d. None of the above.
Diagnosis
Fundus examination of the right eye revealed a hyperemic optic nerve with trace peripapillary edema (Figure 1). Additionally, there were chorioretinal striae and multifocal areas of whitened subretinal exudation dispersed throughout the posterior pole with extension into the temporal midperiphery (Figure 1). Fundus examination of the left eye was normal.
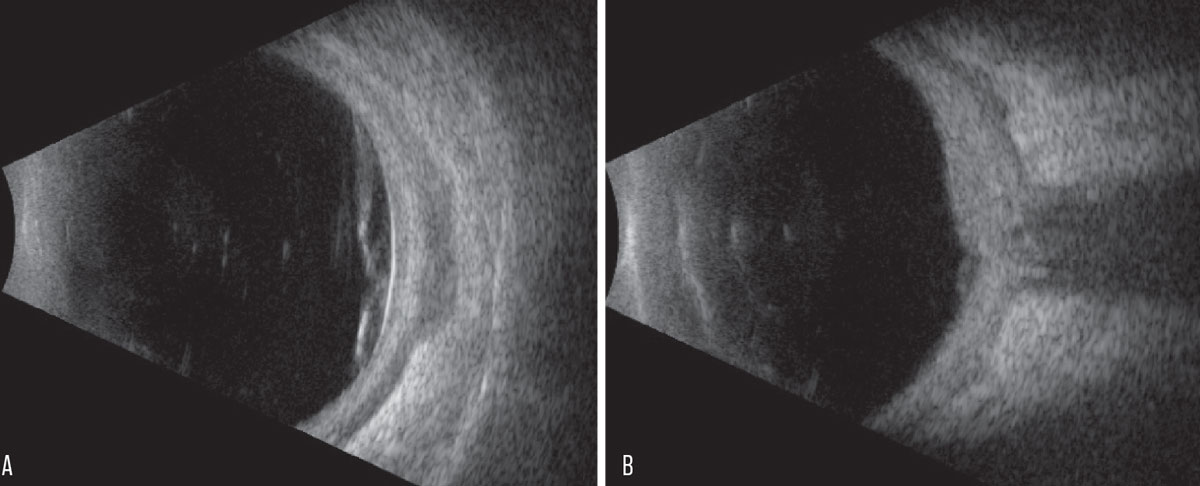
OCT confirmed subretinal fluid within the macula (Figure 2). B-scan ultrasonography demonstrated multifocal retinal detachment involving the macula and extending temporally, diffuse thickening of the fundus (retina, choroid, sclera) and a prominent “T sign” (Figures 3A & B). Additionally, the lateral rectus muscle was thickened and hypoechoic, suggestive of concomitant myositis (Figure 3A).
The patient was diagnosed with panscleritis of the right eye. Initial management involved indomethacin 50mg three times daily and obtaining standard scleritis labs. Once infectious etiologies (i.e., syphilis and tuberculosis) were excluded, he was switched to oral prednisone 60mg daily. This was tapered over five weeks, and he demonstrated complete resolution of inflammation and subretinal fluid. He achieved a final VA of 20/25 in the affected eye.
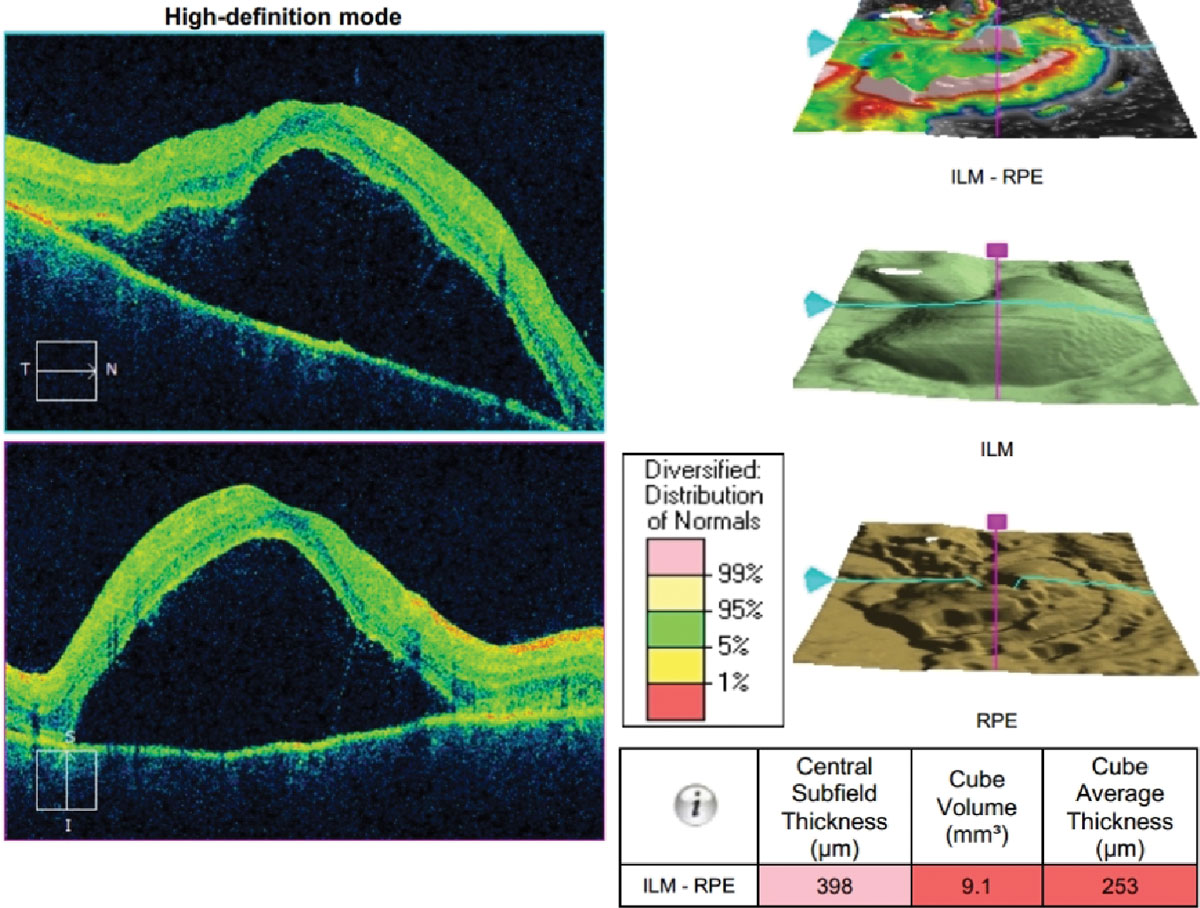 |
| Fig. 2. Cirrus OCT of the right macula. Click image to enlarge. |
Discussion
Posterior scleritis is an inflammatory disorder involving the scleral coat of the eye posterior to the equator and insertion of the rectus muscles.1 It is a potentially blinding condition that can present confined to the posterior segment or with concomitant anterior segment involvement as well (i.e., panscleritis). A case series of 99 posterior scleritis patients showed that 36% presented with panscleritis and 59% developed panscleritis during follow-up.2-4
While large-scale data regarding epidemiology, clinical features and prognosis are limited due to low clinical incidence, smaller case series have allowed for some understanding of the disease process. Posterior scleritis most commonly presents in the fifth decade of life with a female predilection.1,3,4 Scleritis is generally noninfectious and associated with an underlying systemic disease in 35% to 50% of cases but can also be infectious in nature.1,3,4 Patients who present with panscleritis or are 50 years and older have a greater risk of systemic disease.4
Posterior scleritis may be accompanied by orbital myositis, low-grade anterior or posterior uveitis, exudative retinal detachment, choroidal detachment, chorioretinal folds and optic disc edema.1,4,5 Ocular hypertension can occur but is frequently due to ciliochoroidal effusions with anterior rotation of the iridolenticular diaphragm and secondary angle closure.4
Differential diagnoses can include central serous retinopathy, Vogt-Koyanagi-Harada disease, sarcoidosis, Purtscher retinopathy and lupus retinopathy. Posterior scleritis is often a diagnosis of exclusion based on careful history, clinical exam and ancillary imaging. A thorough work-up is also necessary to exclude infections such as syphilis and tuberculosis and systemic vasculitides such as granulomatosis with polyangiitis, which can be life-threatening if untreated.1-4
Ancillary imaging may be useful to confirm diagnosis by visualizing the scleral inflammation on CT/MRI (“ring sign” of scleral enhancement) or B-scan ultrasonography (“T sign” of sub-Tenon fluid accumulation). Generally, B-scan ultrasound is the most informative adjunct imaging modality, with as many as 17% of posterior scleritis patients undetectable without it, but it can be limited in its ability to detect early scleral necrosis.1,3,4 The characteristic “T sign” describes the accumulation of fluid in the sub-Tenon space surrounding the optic nerve (the arms of the “T”) and the shadowing of the optic nerve (the stem of the “T”).1,3,4 However, the most common B-scan finding is diffuse or nodular scleral thickening more than 2mm, which is seen in greater than 50% of cases, whereas the “T sign” is only seen in 25% to 41% of cases.3,4
 |
|
Fig. 3. (A) Transverse B-scan of the globe at the 9 o’clock hour at the equator. (B) Vertical axial B-scan over the posterior pole. Click image to enlarge. |
Treatment
Oral NSAIDs are often a first-line option while awaiting serology results, then switching to targeted anti-microbial therapy is recommended if an infectious cause is identified.1,3,4 Once infectious etiologies are excluded, treatment is often escalated to oral prednisone at a starting dose of 1 to 1.5 mg/kg/day.1,3-5 Severe or refractory cases may be given an intravenous pulse of corticosteroid first, or even require steroid-sparing immunomodulatory therapy.1,3,4 Surgical intervention is rarely necessary but may be indicated to provide tectonic support for scleral necrosis with impending perforation.1,5
Visual prognosis is highly variable; the majority of patients maintain less than a two-line difference from baseline vision at up to 22 years of follow-up, and of those who suffer vision loss, the majority are 20/80 to 20/200.4 Vision loss is often due to chronic macular changes and/or optic atrophy.4 The necrotizing subtype portends a poorer visual and systemic prognosis, particularly if not identified promptly, further highlighting the importance of systemic evaluation for associated life-threatening vasculitides.
Although our patient achieved a desirable outcome, he was counseled on the serious nature of his condition and the need for continued monitoring to ensure that any recurrence is addressed promptly.
Retina Quiz Answers
1: c, 2: d, 3: b, 4: d, 5: d
Dr. Aboumourad currently practices at Bascom Palmer Eye Institute in Miami. He has no financial disclosures.
Dr. Dunbar is the director of optometric services and optometry residency supervisor at the Bascom Palmer Eye Institute at the University of Miami. He is a founding member of the Optometric Glaucoma Society and the Optometric Retina Society. Dr. Dunbar is a consultant for Carl Zeiss Meditec, Allergan, Regeneron and Genentech.
1. Yanoff M, Duker J. Ophthalmology. 5th Ed. 2019. 2. Gass JDM. Stereoscopic atlas of macular disease: a fundoscopic and angiographic presentation. Saint Louis: Mosby, 1st Ed. January 1, 1970. 3. Lavric A, Gonzalez-Lopez JJ, Majumder PD, et al. Posterior scleritis: analysis of epidemiology, clinical factors and risk of recurrence in a cohort of 114 patients. Ocul Immunol Inflamm. 2016;24(1):6-15. 4. McCluskey PJ, Watson PG, Lightman S, et al. Posterior scleritis: clinical features, systemic associations and outcome in a large series of patients. Ophthalmology. 1999;106(12):2380-6. 5. Watson PG, Hayreh SS. Scleritis and episcleritis. Br J Ophthalmol. 1976;60(3):163-91 |

