 |
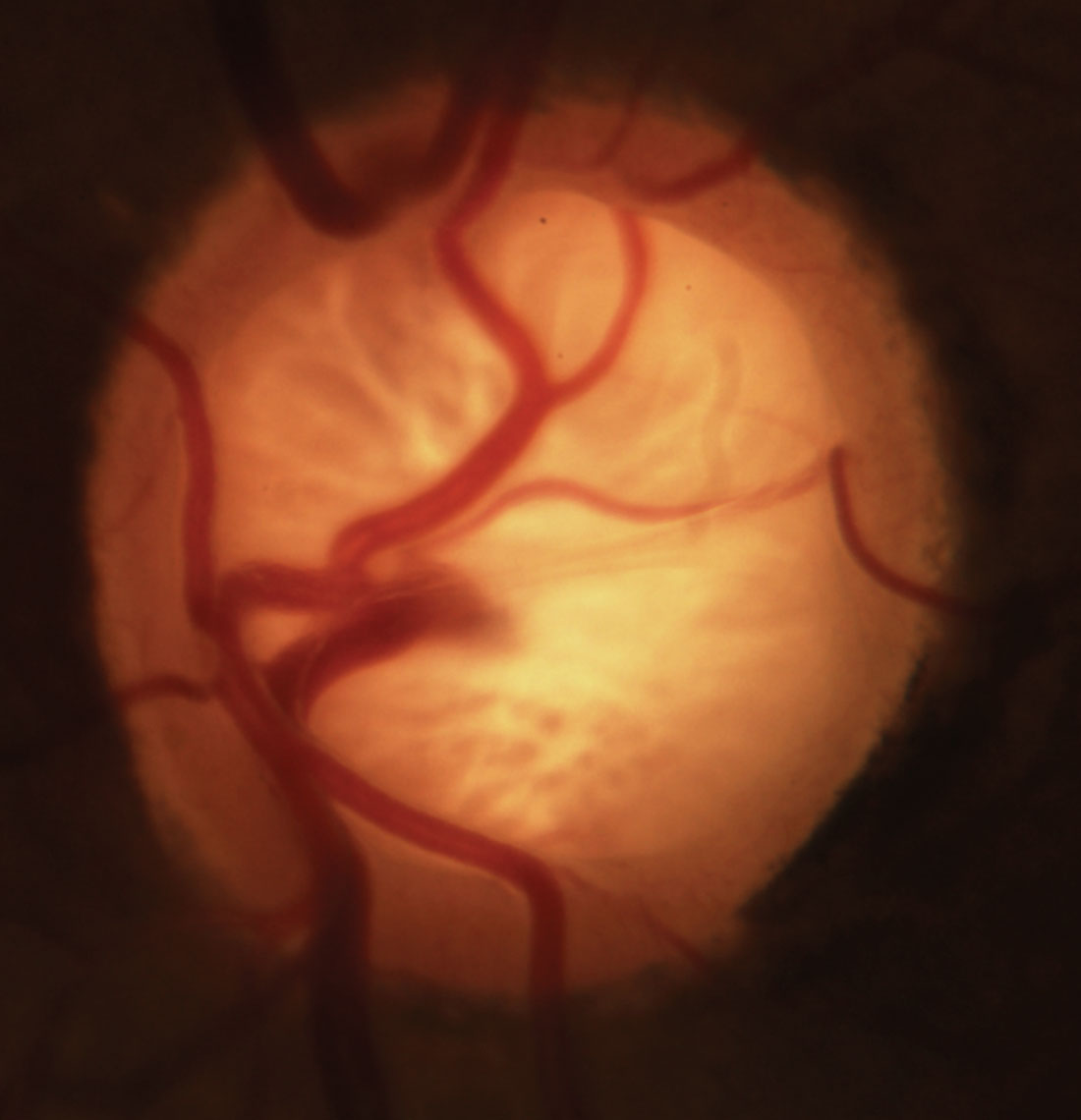
| Blood pressure dip in POAG may not be restricted to the well-established nocturnal phenomenon, as the patients in this study also experienced exaggerated dips when going from a seated to a supine position. Photo: Michael Dorkowski, OD. Click image to enlarge. |
Researchers recently identified a new potential marker of disease severity in patients with primary open-angle glaucoma (POAG): postural blood pressure dip. In their study, an exaggerated drop in blood pressure from a seated to a supine position was positively correlated with severity of glaucomatous optic neuropathy (GON).
To conduct the prospective observational study, 47 POAG patients (64% male; age range: 50 to 66 years) underwent the following measurements in a seated position and after 20 minutes of lying down: intraocular pressure (IOP) and systemic arterial blood pressure (SABP), including systolic (SBP) and diastolic (DBP). The team then calculated the mean arterial blood pressure (MABP) for both seated and recumbent positions, and participants were placed into one of three groups based on the percentage difference between seated and recumbent SBP, DBP and MABP: non-dippers, normal dippers and exaggerated dippers with percentage dips of <10%, between 10% and 20% and >20%, respectively. OCT scans of the optic nerve head were also obtained to measure RNFL thickness (RNFLT) as a biomarker of GON.
In exaggerated dippers, the researchers observed that RNFLT was lower than in non-dippers and normal dippers. They found a negative correlation between postural dip and average RNFLT. Additional analysis revealed that postural dip was associated with lower RNFLT independent of age and IOP.
The team performed a series of other tests to evaluate the data, such as a chi-square independence test, which showed a strong relation between corresponding dip groups for SBP, DBP and MABP but no significant relation between hypertension and postural dip. Additionally, Fisher’s exact test demonstrated no relation between antihypertensive medication and postural dip.
In their paper on the study, which was recently published in the Journal of Glaucoma, the authors relay that these findings support the vascular theory of glaucoma pathogenesis as opposed to the mechanical theory, which suggests that elevated IOP is the main contributor to GON.
“It has been suggested that blood pressure alterations in both hypertension and hypotension exert their effect on the optic nerve either directly through ischemic damage or indirectly through elevated IOP in case of ocular hypertension,” the authors wrote in their paper. “Complex regulation of SABP, IOP and ocular perfusion pressure is needed to maintain adequate perfusion of optic nerve head under different hemodynamic and metabolic conditions.” They go on to state that in POAG patients, this necessary ocular and systemic vascular regulation is deficient, which this study’s findings reflect.
The researchers made another primary observation from the data. Nocturnal blood pressure dip, which compares nocturnal to daytime SABP, is a well-established phenomenon. Recumbent dip, on the other hand, evaluates “the change in SABP secondary to postural change from seated to recumbent position during wakefulness,” the authors explained in their study. Because this study associated recumbent dip with GON severity, “This indicates that blood pressure dip in POAG may not be restricted to the nocturnal phenomenon, implying a more profound systemic vascular dysregulation,” the authors suggest. “Therefore, exaggerated recumbent dip of SABP may serve as a biomarker of systemic vascular dysregulation besides migraine, Raynaud’s phenomenon and nocturnal dip, which have all been associated with the incidence and progression of GON.”
Applying these findings to clinical practice, the researchers suggest that postural dip assessment could serve as “a simple clinic-based test of systemic vascular dysregulation as part of GON risk evaluation.”
Ismail AA, Sadek SH, Kamal MA, et al. Association of postural blood pressure response with disease severity in primary open angle glaucoma. J Glaucoma. November 28, 2023. [Epub ahead of print]. |

