 |
By offering glaucoma management services, you will inherit new patients who have previously been diagnosed with glaucoma and you will certainly have your share of undiagnosed patients who present to your office often for reasons unrelated to their uncontrolled glaucoma. In either case, the glaucoma patients you end up seeing will have mild, moderate or advanced disease.
It’s estimated that the majority of patients with glaucoma have either mild or moderate disease. When you account for the estimated 10% of glaucoma patients with advanced disease, upwards of 90% of glaucoma patients fall into the mild, moderate and advanced stages. The other 10% are the refractory cases, who seem to worsen even with advanced surgical care.
As primary eyecare providers, optometrists are perfectly positioned to manage mild, moderate and advanced cases of glaucoma. Sometimes, those with progressive disease who are unresponsive to topical therapy will need surgical interventions, some of which are successfully and regularly performed by optometrists. Even those advanced glaucoma patients who remain stable without the need for surgical intervention can remain in the realm of optometric care throughout their care.
This is the first of two columns dedicated to managing patients with advanced disease. Once you've finished reading this one, find the second column here.
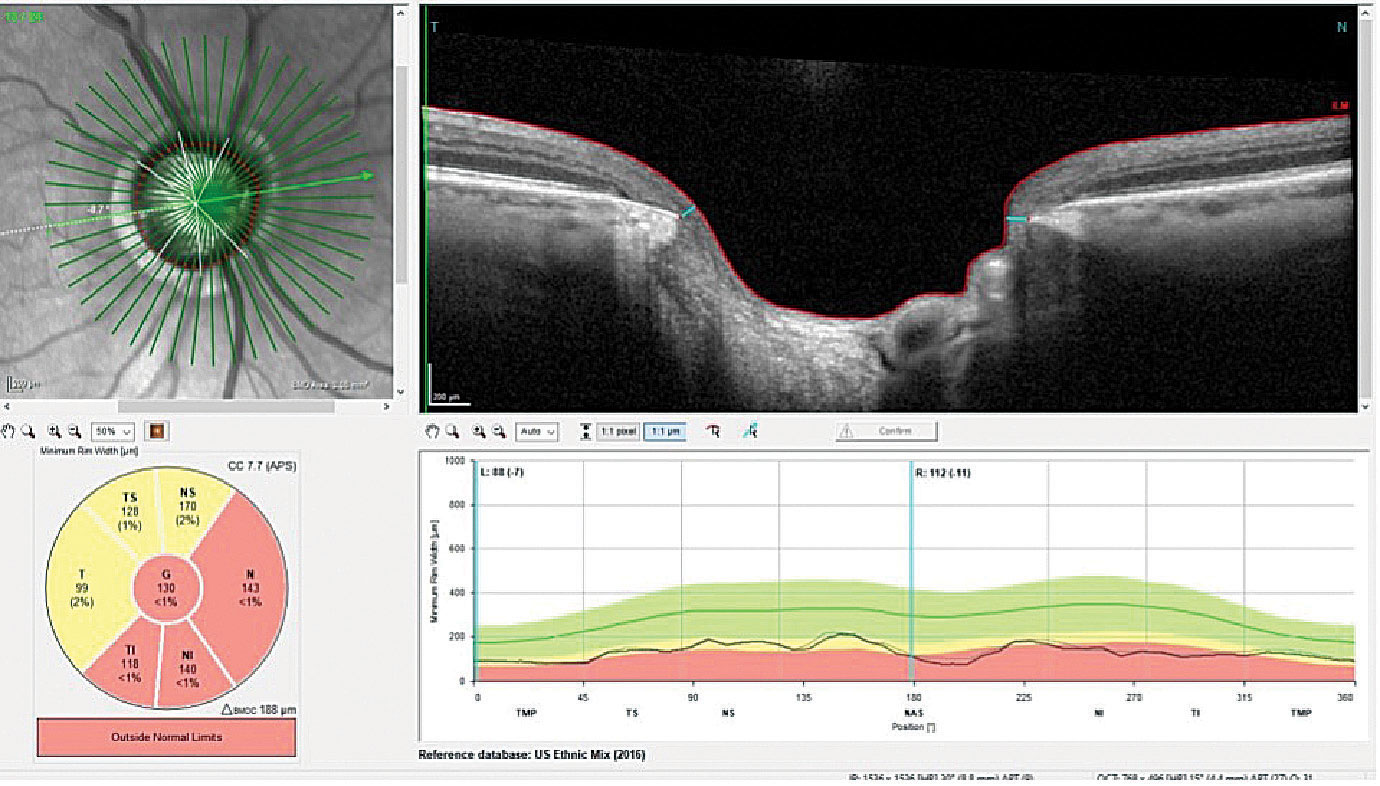 |
A thinned BMO 360° OD, with the temporal rim thinned to about 100µm. Click image to enlarge. |
Case
In November 2019, a new patient presented to establish care after moving to the area. This 78-year-old Caucasian male had an established history of glaucoma diagnosed approximately four years earlier. When initially seen he was prescribed latanoprost OU HS. Medications at that time consisted of losartan, atenolol, amlodipine, ezetimibe and 81mg of aspirin. He was intolerant of statins and reported no allergies to medications.
His initial IOPs were 13mm Hg OD and OS, with pachymetry readings of 596µm OD and 570µm OS. His best-corrected visual acuities were 20/25- OD and OS. His pupils were ERRLA with no afferent pupillary defect.
A slit lamp examination of his anterior segments was essentially unremarkable, with open angles and a clear anterior chamber. He was pseudophakic OU.
Through dilated pupils, his IOLs were clear and centered, and both capsules were clear and intact. His cup-to-disc ratios were judged to be 0.80x0.80 OD and 0.85x0.85 OS. The optic nerves were of average size. The retinal vasculature was characterized by mild arteriolarsclerosis OU. The maculae were clear with fine RPE granulation noted subfoveally OU. There was a small nevus along the superior arcade that was one disc diameter in size OS. The peripheral retinal evaluation was essentially unremarkable.
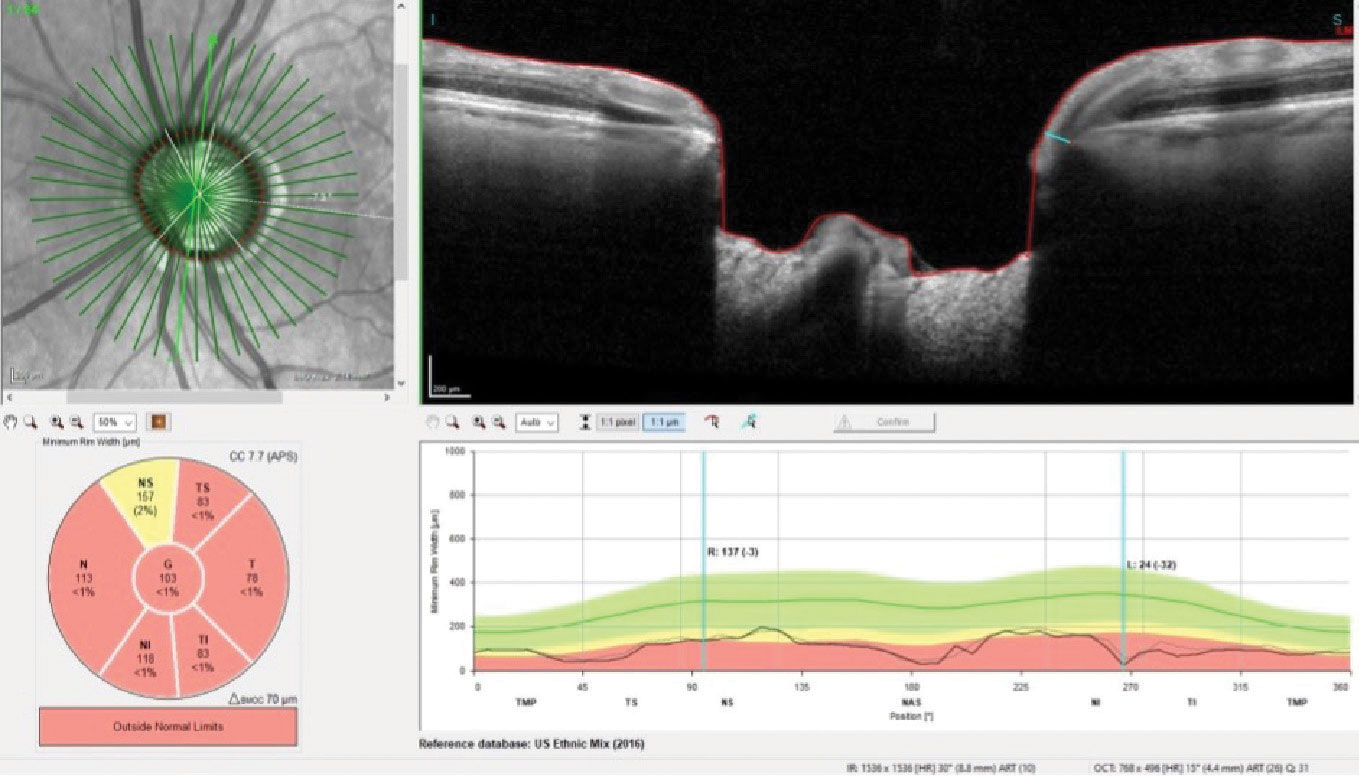 |
Thinned BMO neuroretinal rim tissue OS, with some thinning of the superior rim down to a paltry 24µm of tissue. Click image to enlarge. |
At the initial visit, HRT3 and OCT images of both optic nerves were obtained. The HRT3 findings coincided with the estimation of normal-sized optic nerves with thin neuroretinal rims OS>OD.
Given the patient was compliant with latanoprost, was establishing care with me for the first time and did not appear to be uncontrolled, I did not change his glaucoma treatment regimen and scheduled a follow-up. I explained to him that my goal was to establish that his glaucoma was well-controlled, and in order to do so I would need to see him twice more at three-month intervals to obtain various metrics related to his glaucoma. Once I determined him to be stable, we would then cut our visits back to approximately every five to six months.
The patient complied and was seen regularly as scheduled. Over the subsequent visits, visual fields were obtained that demonstrated arcuate defects OS>OD consistent with the structural findings. Gonioscopy revealed IV+ open angles with minimal trabecular pigmentation; there were no angle abnormalities. Multicolor optic nerve images were obtained.
The patient was seen most recently in November 2022 for a scheduled follow-up, at which time OCT images and visual fields were obtained. He was deemed stable from a glaucoma progression perspective.
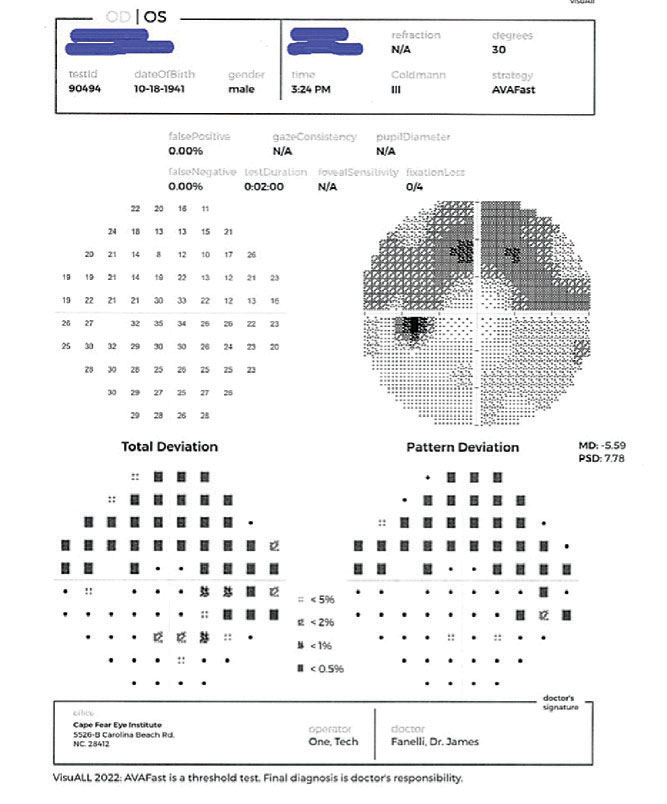 |
| The visual field defect seen in the patient’s left eye. Click image to enlarge. |
Discussion
Our protocol when obtaining OCT scans of the optic nerve in the context of glaucoma is to obtain scans of the neuroretinal rim, the perioptic RNFL and the macular ganglion cell layer in both maculae. Not surprisingly, the patient’s RNFL circle scans showed damage in the nerve fiber layer adjacent to the nerve consistent with the damage seen in the neuroretinal rim OS>OD. The macular ganglion cell layer of the left eye showed an inferior temporal wedge defect and superior temporal loss of the ganglion cells involving the foveal avascular zone.
While the patient’s latest visual field studies were stable, of particular note was the left eye’s results. The visual field showed a distinct superior arcuate defect, owing to the significant RNFL loss inferiorly. It also showed an inferior nasal defect related to the ganglion cell loss. Note also that both the superior and inferior hemifield defects spared a good portion of the central 10° of the visual field due to the relatively robust central ganglion cell layer.
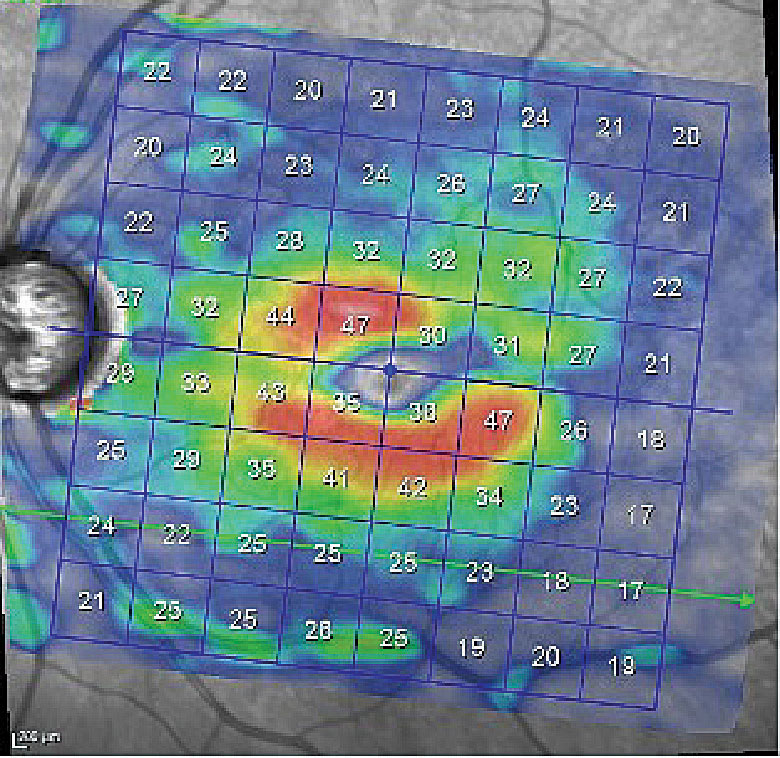 |
Ganglion cell layer loss just inside the inferior arcade and loss superotemporally to the foveola involving the perifoveal retina. Click image to enlarge. |
And herein lies the point of this case. While this patient has advanced glaucoma, he has remained stable for the two years I’ve seen him. Furthermore, his visual field defects, in particular that of the more advanced left eye, have not involved fixation, and that plays a significant role in his lack of symptomatology. In other words, his fields don’t look as bad as I was expecting given the extent of his damage.
Advancing Glaucoma, Pt. 2Find the second column by Dr. Fanelli on managing cases of progressing advanced glaucoma here. |
Does he need any change in therapy at this time? No, not at all. And that is because he has advanced glaucoma that is stable. Will he remain stable? There is no way to answer that question at this time, other than to say we will know the answer only after diligent and stringent follow-up and monitoring. Certainly, his disease won’t improve; he’ll either stay stable or get worse. Close surveillance will be key here. Can he get worse? Of course. Will he get worse overnight? Not likely, but he can show significant progression if he’s not being cared for by the right provider in the right way. And who is considered this adept provider? It should be you.
Dr. Fanelli is in private practice in North Carolina and is the founder and director of the Cape Fear Eye Institute in Wilmington, NC. He is chairman of the EyeSki Optometric Conference and the CE in Italy/Europe Conference. He is an adjunct faculty member of PCO, Western U and UAB School of Optometry. He is on advisory boards for Heidelberg Engineering and Glaukos.

