 |
This is the second of two columns dedicated to managing advanced open-angle glaucoma. The previous column dealt with a case that so far has had a good outcome; this one details a case of worsening and how to proceed.
As previously mentioned, approximately 10% of glaucoma cases are considered advanced, whereas the majority of cases (80%) are mild to moderate. Not considering the refractory cases of glaucoma that progress despite intervention (10%), the 10% of patients with advanced open-angle glaucoma can successfully be managed by a well-trained, knowledgeable OD.
However, given that these individuals have advanced disease, there is less margin of error, and extremely close monitoring needs to occur to preserve vision. But even with well-intentioned and regular surveillance, sometimes these individuals do still progress. Identifying progression and intervening early is critical. With advanced disease comes less healthy structural neural tissue and more advanced visual field loss. Significant progression can have significant effects on quality of life.
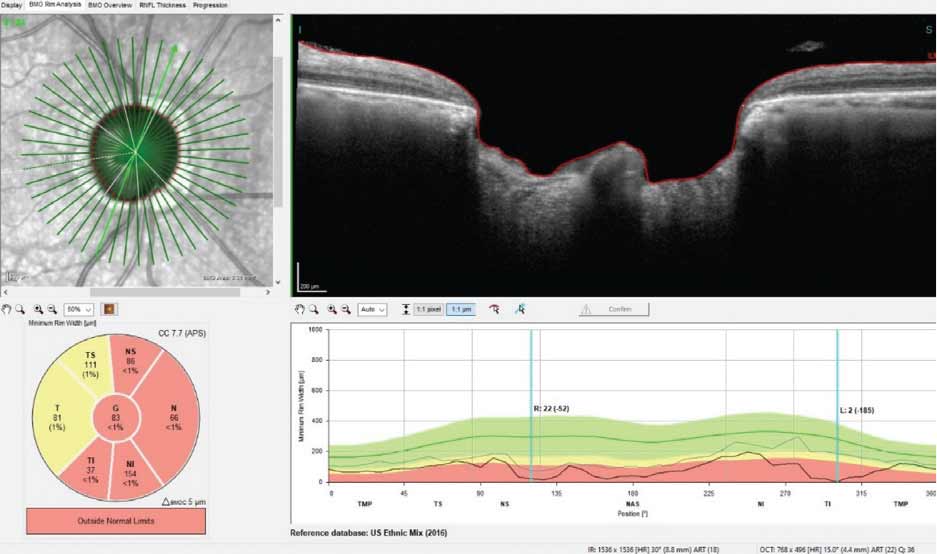 |
A significant loss of neuroretinal rim tissue inferotemporally, with loss of 185µm shown in the selected radial scan. Click image to enlarge. |
Case
A now 84-year-old African American male initially presented in 2009 for a wellness evaluation. He had noted some changes in his vision and was interested in updating his glasses. It had been four years since his previous visit.
Two significant findings were observed at the initial visit: moderate cataracts and significant neuroretinal rim loss consistent with glaucoma. Cataract surgery was put on hold until firm baselines were established for the glaucoma and it had adequately stabilized. While the diagnosis was pretty straightforward following the initial testing, the reality of a visual field defect involving fixation also played a role in the patient’s subjectively decreased vision.
Essentially, the patient had thin central corneal thickness readings (511µm OD and 501µm OS) and untreated intraocular pressures (IOPs) oscillating in the low 20s. The neuroretinal rims were essentially characterized by 0.80 x 0.90 cupping symmetrically with eroded rims OD in the inferotemporal sector and OS in the superotemporal sector. These structural defects were confirmed on both HRT3 and OCT scanning and were consistent with the initial visual field defects seen on formal perimetric studies.
Ultimately, the patient’s glaucoma was stabilized with a regimen of Lumigan HS OU as well as Azopt BID OU. Post-treatment IOPs hovered in the 10mm Hg to 14mm Hg range OD and 11mm Hg to 14mm Hg range OS over several treatment visits.
Initially, the glaucoma stabilized over a 12-month period, during which time the cataracts had further progressed to the point of affecting the clarity of the patient’s remaining vision and his quality of life. Cataract surgery ultimately occurred in 2011 with excellent results.
Best-corrected visual acuities following intraocular lens extractions were 20/30- OD and 20/25+ OS. While the anterior chamber angles were open prior to cataract surgery, they were fully open following surgery. Gonioscopy never revealed any angle abnormalities other than moderate trabecular pigmentation. IOPs essentially remained stable compared with treated preoperative IOPs. The anterior segment was unremarkable, except for occasional superficial punctate keratopathy and the concurrent complaints associated with ocular surface issues.
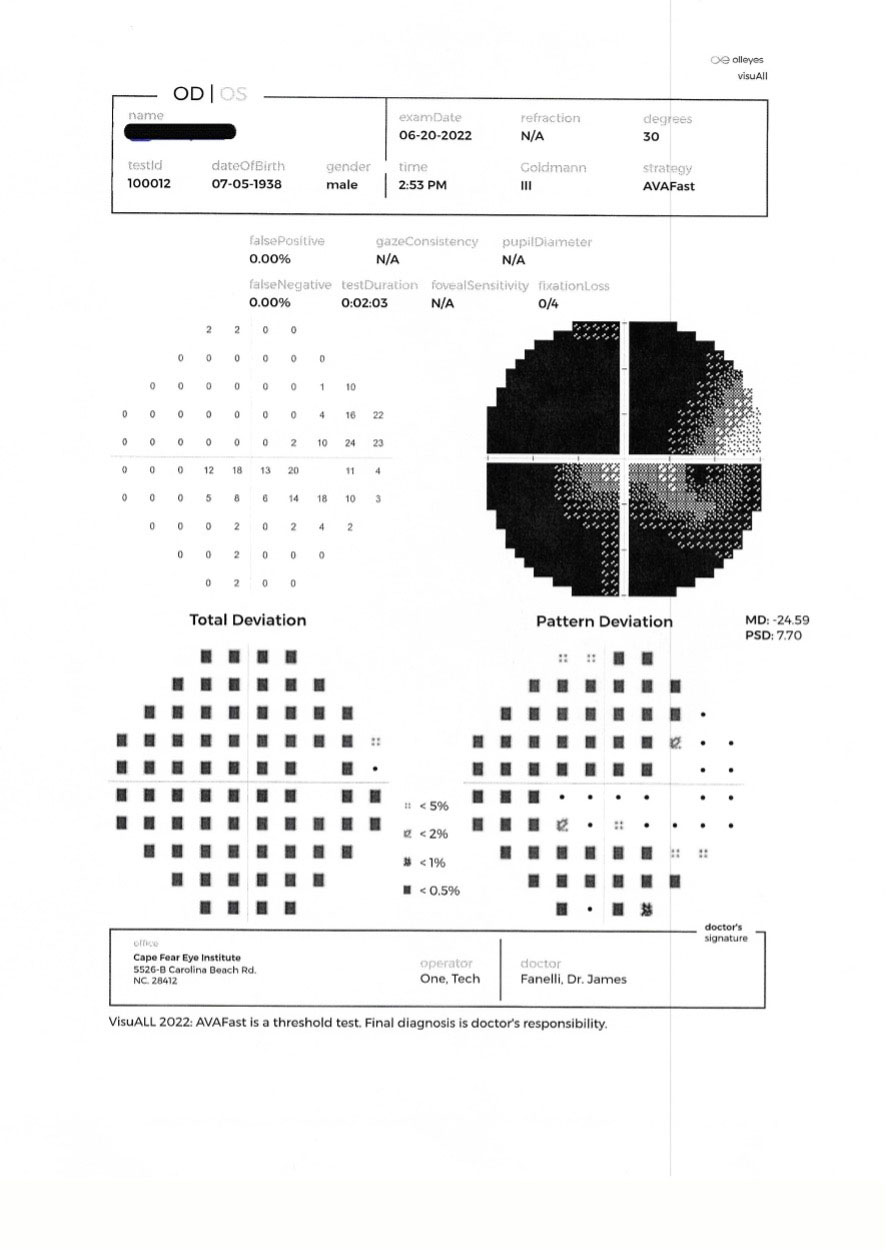 |
| A 30-2 threshold field following loss of control of the right eye in June 2022. This was the second VF since re-evaluation. Click image to enlarge. |
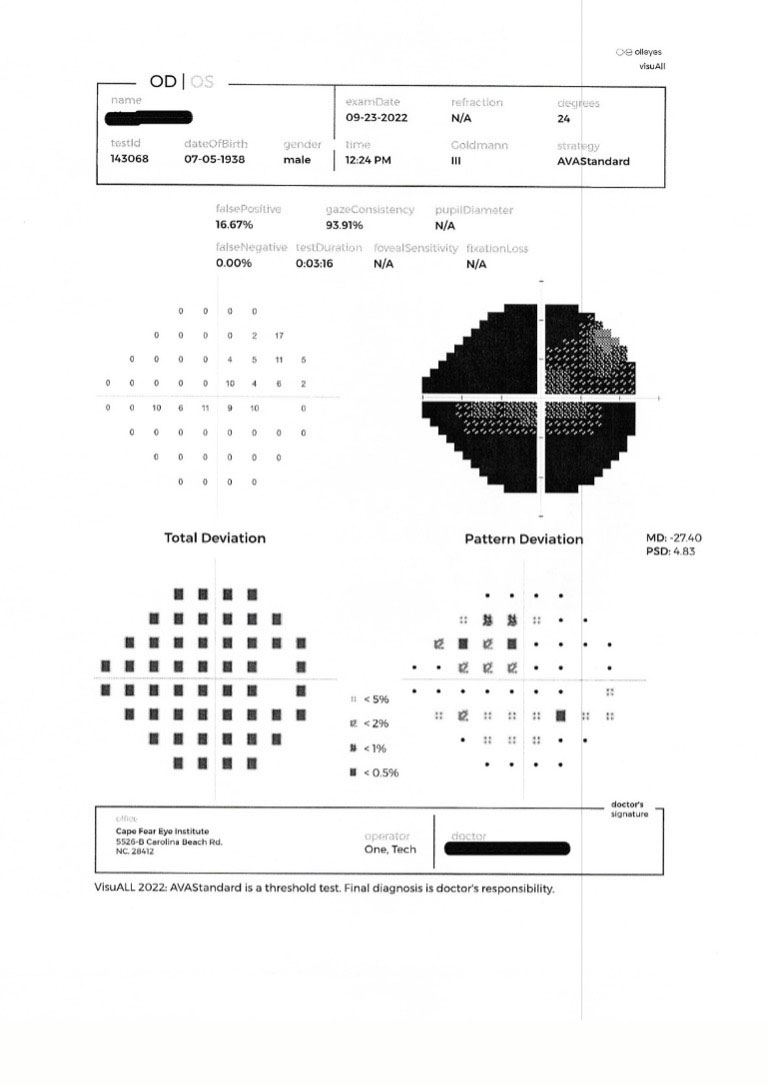 |
| A 24-2 threshold field three months later. This is the third VF since re-stabilization of the right eye. Note the stability. Click image to enlarge. |
The patient’s macular evaluations have remained stable with mild RPE granulation consistent with his age. The retinal vascular evaluation also remained stable with mild arteriolarsclerotic retinopathy consistent with the long-standing history of hypertension and elevated triglycerides. His systemic medications aiming to treat the hypertension, hyperlipidemia, gout and acid reflux were also stable throughout our time together. The peripheral retinal evaluations were essentially normal, and bilateral posterior vitreous detachments were noted.
Unsurprisingly, the patient’s Medicare Part D coverage changed, precipitating a need to find alternative IOP-lowering agents. In 2016 we settled on Xelpros HS OU and 0.5% timolol QDam. Structurally and functionally, he remained stable on this regimen.
While COVID interfered with regular follow-up care, we were able to refill his medications during the majority of 2020 and through late 2021. The patient was reluctant to come into the office because of COVID, and due to his mature age and higher risk of COVID complications, it wasn’t until early 2022 that he made it back into the office.
He reported that ever since he had taken a bad fall a few months earlier, his right eye hadn’t felt entirely normal, and his vision OD seemed to have gotten worse. Unfortunately, IOPs were 28mm Hg OD and 12mm Hg OS. His anterior chamber in the right eye was characterized by grade 1 cells and trace flare. There was mild limbal episcleral inflammation consistent with the anterior chamber reaction OD. Visual acuities were 20/50- OD and 20/30 OS. OCT showed marked neuroretinal rim loss OD. He was dilated with three drops of 5% homatropine and given an Rx of Pred Forte QID OD to use until follow-up to quiet the anterior uveitis OD.
The patient ultimately returned a week later, at which time his IOPs were 25mm Hg OD and 13mm Hg OS. The anterior chamber had no flare, and trace cells were seen; the episcleral injection was cleared.
Visual fields demonstrated significant progression OD with further involvement of fixation, and the left visual field remained stable from previous visits. Gonioscopy was essentially stable as well, with no evidence of abnormalities OU or angle recession OD.
While the anterior chamber reaction may certainly have played a role in the elevated IOP OD, it became a secondary issue once it was clear that the IOP was still elevated even though the chamber was quieter. Consider the possibility that IOP could now be elevated because of the introduction of the steroid. At this point, it became critical to lower IOP and ultimately titrate off the topical steroid as soon as possible. Accordingly, the Pred Forte was scheduled for a slow taper, and the right eye was dilated with 1% atropine given the clear angle findings. The Xelpros was stopped, and Vyzulta was substituted HS OU.
The patient followed up a week later as scheduled, and ultimately after a couple of weeks, the steroid was discontinued, and his glaucoma regimen was Vyzulta HS OU and Cosopt BID OU. IOP OD was reduced to the 10mm Hg to 13mm Hg range and OS to the 10mm Hg to 12mm Hg range.
At this point, it was clear that the patient had progressed, but the bigger question now became one of stabilization. It can be argued that he should have been sent to a glaucoma specialist at the first visit in 2022 when it was clear that he had progressed structurally and functionally and that his IOP was high. However, a good glaucoma specialist would have also realized that the inflamed anterior chamber was playing a role and that inflammation needed to be brought under control, requiring a balance between steroid inflammatory control and IOP control. A well-trained OD would come to the same conclusion.
I felt confident that we could bring the anterior chamber inflammation under control, but I initially was not certain that the glaucoma would remain stable. But once the IOP was brought under control and the chamber reaction was quieted, perhaps he would remain stable. If not, off to glaucoma surgery he’d go. But if he did remain stable moving forward, then no surgery would be warranted given the fragility of his nerves.
While the patient reported decreased visual acuity, and the visual field loss worsened during the absence of in-office care, it appeared as though he had stabilized. Overall, he did experience progression, but with consistent follow-up and appropriate management, we were able to control his glaucoma.
Advancing Glaucoma, Pt. 1In case you missed it, find Dr. Fanelli's previous column on managing cases of progressing advanced glaucoma here. |
The patient was watched closely in 2022, with the most recent field study conducted in September. Structural indices have remained stable since early 2022, and so have the visual fields. IOPs have remained under 13mm Hg OD and OS since being brought under control, which means he is stable for the time being. Is he going to remain stable? The OD in me, as well as the OD in you, will see over time if that remains the case. If not, we’ve got a plan that involves surgery. But for now, the regimen is continued care in my office.
Dr. Fanelli is in private practice in North Carolina and is the founder and director of the Cape Fear Eye Institute in Wilmington, NC. He is chairman of the EyeSki Optometric Conference and the CE in Italy/Europe Conference. He is an adjunct faculty member of PCO, Western U and UAB School of Optometry. He is on advisory boards for Heidelberg Engineering and Glaukos.

