 |
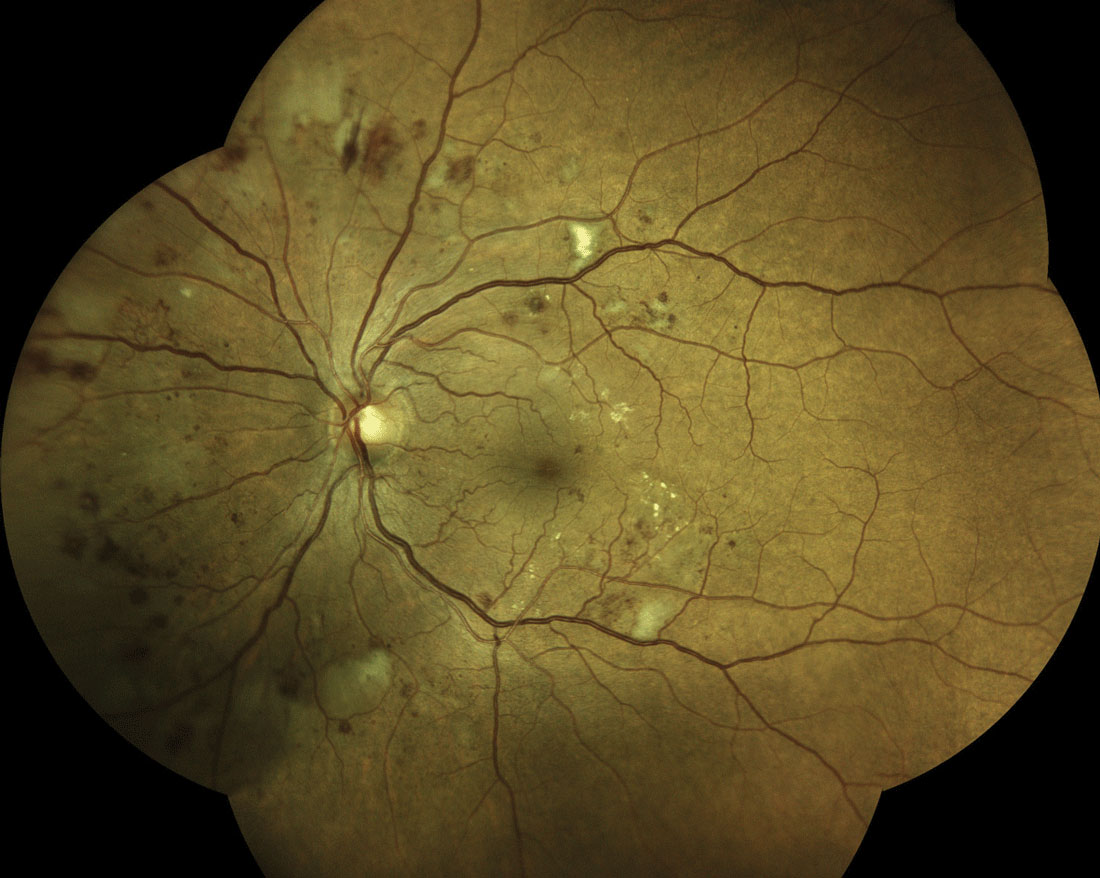
| Older age and worse DR severity were the top two risk factors for vision loss identified in this study among patients with diabetes. Photo: Steven Ferrucci, OD. Click image to enlarge. |
Many studies have researched different aspects of diabetic macular edema (DME), the most effective treatments (anti-VEGF) and why it’s one of the main contributors to vision loss among diabetic patients. But previous research has failed to assess patients in real-world settings, such as those who have inconsistent follow-ups, receive fewer injections and experience visual anatomic outcomes. A recent study aimed to identify those clinical and anatomic factors in DME patients.
Central subfield thickness (CST), intraretinal fluid, intraretinal hyperreflective foci and disorganization of retinal inner layers were some of the biomarkers that were evaluated among 48 patients with DME and visual acuity of 20/25 or better. The team suggests the clinical factors most strongly associated with vision loss are older age and diabetic retinopathy (DR) severity. This is consistent with findings from the Protocol V study, as well as the MEAD study.
Eyes with severe nonproliferative DR and non-high risk or inactive proliferative DR were three- and 7.7-times, respectively, more likely to suffer vision loss requiring anti-VEGF therapy based on Protocol V recommendations.
“Our results are consistent with the natural history findings of 350 patients with DME in the MEAD study, where older age and worse baseline DR severity scores were associated with worse best-corrected visual acuity outcomes,” the authors explained. “We also confirmed the findings from a post-hoc analysis of Protocol V, where observed eyes with worse DR severity were also more likely to require anti-VEGF treatment during the two-year study.”
This study suggests the main driving structural features may include cyst diameter and baseline CST, but the authors note further research is needed to confirm this hypothesis.
“Because most of the eyes with good visual acuity in our cohort demonstrated minimal disorganization of the retinal inner layers or external limiting membrane/ellipsoid zone/interdigitation zone disruptions, which are respective markers of inner and outer neuronal dysfunction, we hypothesize that our cohort study was also not sensitive enough to identify the predictive effects of these biomarkers,” the authors wrote. “Thus, future studies that encompass more severe DME anatomy or longitudinal analysis of OCT biomarkers at later time points may identify additional imaging predictors of visual outcomes.”
Still, older age and worse DR severity remain important risk factors when deciding on the most suitable number of follow-up visits for DME patients.
Lent-Schochet D, Lo T, Luu KY, et al. Natural history and predictors of vision loss in eyes with diabetic macular edema and good initial visual acuity. Retina. 2021;41(10):2132-9. |

