 |
|
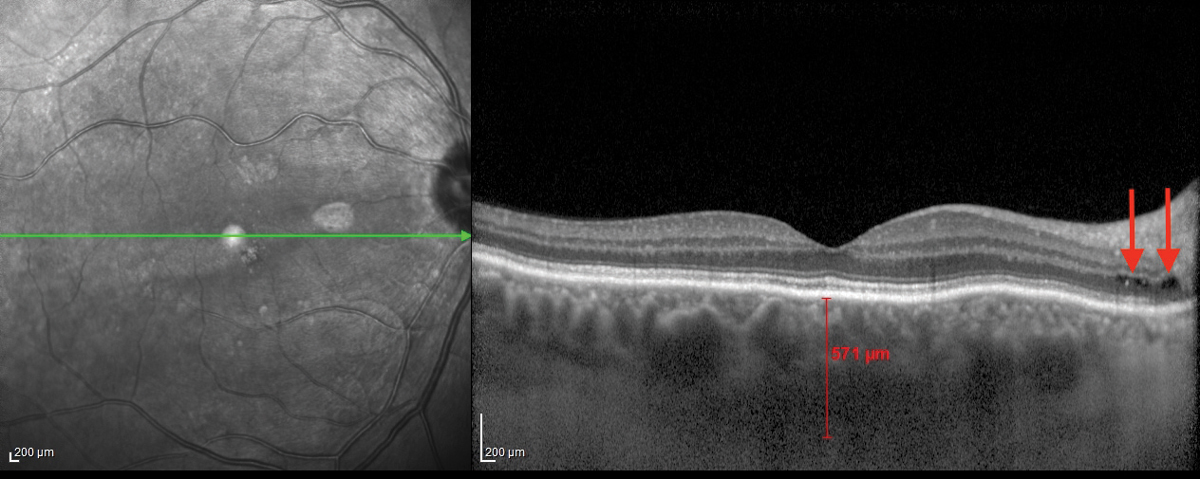
Macular choroidal thickening (shown here in an unrelated patient) may help predict myopia control efficacy over a year. Photo: Jim Williamson, OD, and Meagan Williams, OD. Click image to enlarge. |
Repeated low-level red light (RLRL) therapy is emerging as a treatment for myopia control, but the effects on macular choroidal thickness over the long term have not yet been identified. In a recent study, researchers evaluated longitudinal choroidal changes in myopic children treated for one year with RLRL therapy and the predictive value for treatment efficacy.
A total of 120 myopic children between the ages of eight and 13 with available choroidal thickness data were included in the study. RLRL therapy was delivered using a home-use desktop light device which emitted red light at 650nm. Thickness was measured by swept-source OCT at baseline and one, three, six and 12 months follow-up. Visual acuity, axial length (AL), cycloplegic spherical equivalent refraction (SER) and treatment compliance were also measured.
In the RLRL group, changes in macular choroidal thickness from baseline remained positive over one year, with a maximum increase of 14.76μm at one month and a gradual reduction from 5.29μm at three months to 1.54μm at six months, finally reaching 9.09μm at 12 months.
In the control group, changes from baseline were -1.11μm, -8.21μm, -10.19μm and -10.41μm at one, three, six and 12 months, respectively.
In their paper for the Ophthalmology journal, the researchers noted that “values at all four follow-up visits in the RLRL group were significantly greater than the ones in the control arm.” While the reasons for reduced thickening at the three- and six-month visits are unknown, they speculated that perhaps this can be explained by “a compromise on measurement accuracy secondary to poor participation at the six-month visit (28.3% lost to follow-up) due to the COVID-19 pandemic.”
Among children treated with atropine 0.01%, the team found that 25.9% of six-month AL changes could be explained by one-week choroidal thickness change, age, gender and the presence of peripapillary atrophy. Similarly, 58.0% of 13-month changes in AL following orthokeratology could be explained by one-month macular choroidal thickness changes, baseline age and one-month changes in biometric measurements, they explained.
Three-month choroidal changes alone could predict satisfactory RLRL treatment efficacy on both axial length and refraction.
The researchers noted that three-month choroidal changes performed better in predicting satisfactory RLRL treatment efficacy on axial length than on spherical equivalent progression. “This discrepancy may be in part explained by the complexity of SER, which should be attributed to the combined effect of the cornea, crystalline lens and AL,” the authors explained. They also acknowledged a potential effect from the limited sample size.
The authors added that choroidal thickening occurring as early as one month may also serve as a predictor of red-light treatment efficacy on myopia control.
“In conclusion, as early as one month after RLRL therapy, macular choroidal thickening reached its peak magnitude and was associated with 12-month myopia control efficacy,” the authors explained. “Macular choroidal thickening may be a proxy for future treatment response and serve as a reference for guiding treatment regimens. Further studies should elucidate mechanisms underlying choroidal thickening following RLRL therapy.”
Xiong RX, Zhu Z, Jiang Y, et al. Longitudinal changes and predictive value of choroidal thickness for myopia control following repeated low-level red-light therapy. Ophthalmology. October 3, 2022. [Epub ahead of print]. |

