 |
|
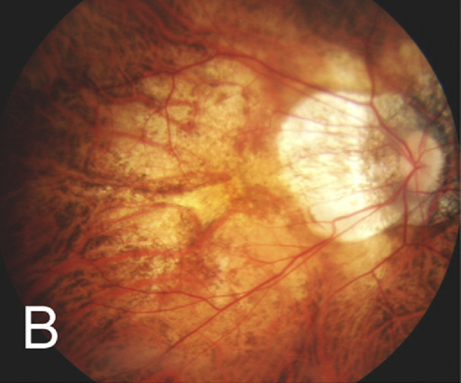
Diffuse chorioretinal atrophy seen in a 51-year-old, -21.00D myopic woman. Photo: Kengo Hayashi, MD. Click image to enlarge. |
Given the detrimental ocular changes wrought by development of myopic maculopathy (MM), researchers from Shanghai recently sought to explore potential biomarkers in hopes of giving clinicians more tools for early identification. The team looked at macular choroidal thickness and ocular biometry.
The study—totaling 1,947 total patients from a Chinese high myopia cohort—included all participants undergoing detailed ocular examinations. MM was subdivided into thin choroid, Bruch’s membrane defects, choroidal neovascularization and myopic tractional maculopathy as determined through OCT-based classification. Peripapillary atrophy area (PPA), tilt ratio, torsion and macular choroidal thickness were also measured.
Through the researchers’ model, myopic maculopathy and different types were more likely to occur with older age, longer axial length, a larger PPA area and thinner average choroidal thickness . Females were also found more likely of having MM and Bruch’s membrane defects. A lower tilt ratio, however, was found more likely associated with choroidal neovascularization and myopic tractional maculopathy.
“The proportions of MM, as well as each type of MM, might increase nonlinearly with aging, with an accelerated period of increase at 50-69 years old,” the authors of the study explained in their paper for the journal Eye. “The results also showed a distribution pattern in the thinning of choroidal thickness and large PPA area that might occur with aging and might lead to more severe myopic chorioretinopathy,” they added. From their findings, they suggest that some combination of peripapillary atrophy area and choroidal thickness could prove useful predicting MM and four types of MM.
The study researchers compared their findings to similar research for the proportion of myopic maculopathy seen in a high myopia group. This study’s 35.9% proportion was lower than hospital-based cohorts from Japan (80.4%) and China (54.4%), but fell in line with a Singaporean population-based study (28.7%) of high myopic patients 40 years or older.
Consequently, the study authors posit that case severity should represent high myopia in general clinical settings. They do continue that a German population-based study found even lower myopic maculopathy presence than this study, with patients aged 35 to 74 years old resulting in only an 8.4% presence. When considering this difference, ethnic backgrounds might play a role in MM prevalence.
In addition to the primary factors found associated with predicting MM (PPA and choroid thickness), tilt ratio and torsion were found significantly associated with axial elongation and aging. However, after analysis, this was found to be a less sensitive factor associated with MM when compared with using PPA area.
Despite this fact, the study authors still include it as important in consideration when developing guidelines. As they put it, “PPA area, tilt ratio and [macular choroidal thickness] could be used as parameter for MM and each type of MM with high accuracy. The cut-off value of a combination of peripapillary atrophy areas and choroidal thickness could be better used to predict MM and each type of MM.”
He J, Ye L, Chu C, et al. Using a combination of peripapillary atrophy area and choroidal thickness for the prediction of different types of myopic maculopathy. Eye (Lond). March 6, 2023. [Epub ahead of print]. |

