 |
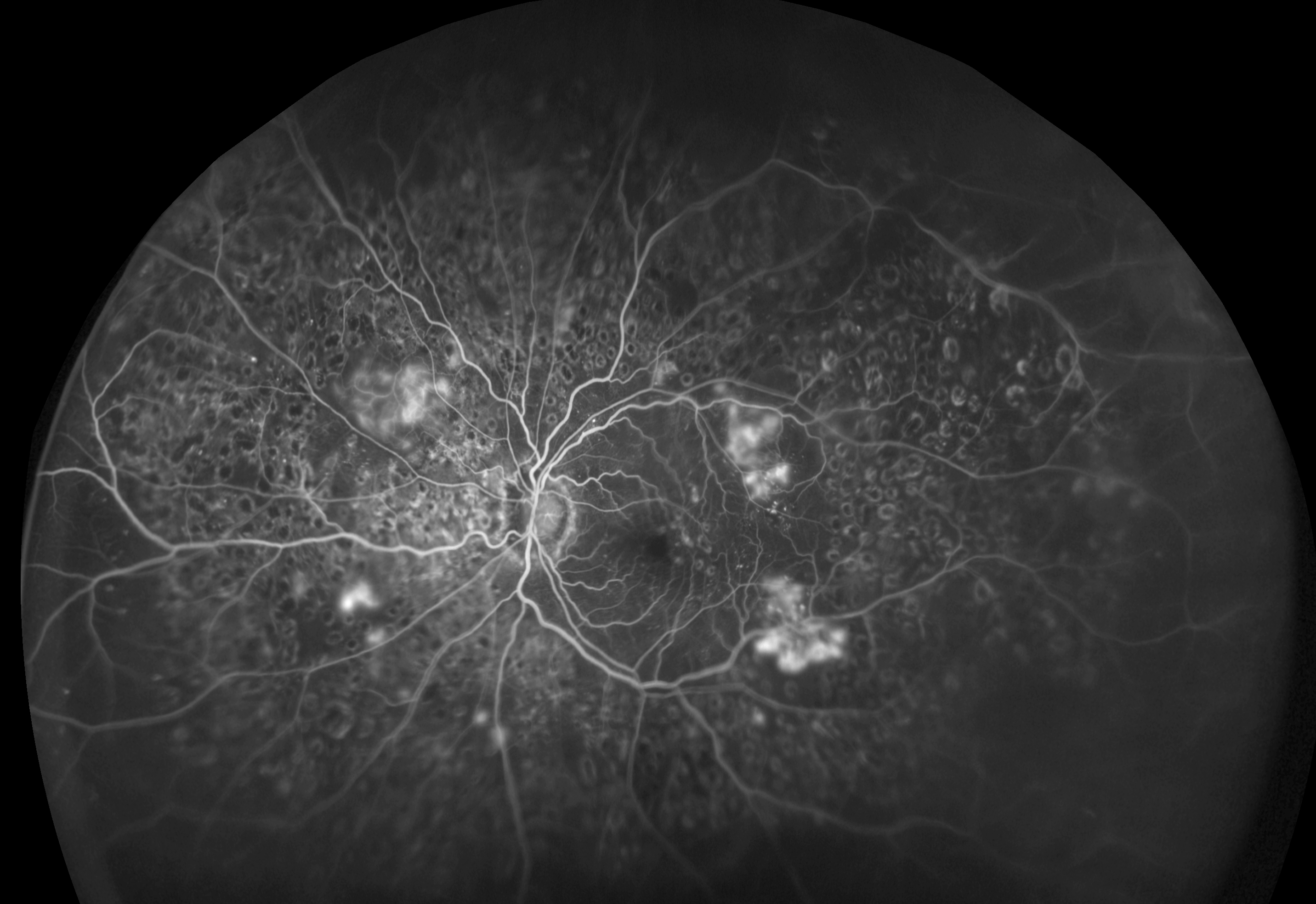
| Severe proliferative diabetic retinopathy may go undetected in patients with severe mental illness, as these patients often don’t see an eye doctor until it’s too late. Photo: Optos. Click image to enlarge. |
Evidence has emerged highlighting the link between eye health and mental health and the potential role of the eye as a window to understanding the central nervous system. As research on severe mental illness and eye health is rare, researchers recently sought to close this gap by examining the association of mental health with a range of ophthalmic outcomes and investigate whether any relationship is modified by age.
Administrative data from general practitioner hospital and ophthalmic records of nearly 800,000 individuals (798,564 to be exact) in Northern Ireland hospital population was used to examine receipt of any eye test and diagnoses of glaucoma, diabetes or blindness.
When compared with unaffected patients, those with severe mental illness—examples given included schizophrenia and bipolar disorder—were more likely to have a vision test, diabetes and blindness. After adjusting for unrelated variables, higher likelihood of an eye test and diabetes but lower likelihood of glaucoma remained. Lower glaucoma rates among severe mental illness patients may reflect their younger age profile of that population, the researchers suggested.There was also evidence that the likelihood of having an eye test was lower in the older age groups among people with severe mental illness.
This study highlights potential inequalities in provision of health care, particularly among older people with severe mental illness. “The higher rates of diabetes found in severe mental illness patients in ophthalmic healthcare settings underlines the need for more assertive and routine diabetes screening in this population, ensuring early detection and intervention,” the authors wrote in their study.
“While our analysis indicates higher levels of eye examinations among severe mental illness patients per se, interaction analysis based on age group shows that older individuals with severe mental illness were less likely to have had an eye test,” the authors explained. These findings are similar to results from recent research on severe mental illness and dental health outcomes and highlight an unmet need among older patients with severe mental illness.
“Importantly, our study also identifies key sociodemographic characteristics associated with ophthalmic service use and related health outcomes; for example, it points to gender differences, with females more likely to have had an eye test and recorded blindness but less likely to have glaucoma or diabetes recorded,” the authors explained. “Our findings also highlight urban-rural inequity, with lower levels of eye testing among rural dwellers but higher risk of adverse ophthalmic-related health outcomes. This finding, which merits further research into underdiagnosed ophthalmic health problems in rural communities, fits in a wider context of rural/urban disparities in access to healthcare services.”
The authors also found a higher prevalence of eye examinations among those who were previously married, with increased chances of glaucoma among the widowed group and diabetes in the divorced group.
“While higher rates of glaucoma among widows is likely to reflect the higher prevalence of the condition among older people, research points to the association of environmentally modifiable risk factors such as lifestyle, exercise and nutrition, which may play an important role for this sub-group,” the authors noted.
Ferry F, Rosato M, Leavey G. Severe mental illness and ophthalmic health: a linked administrative data study. PLoS ONE. May 24, 2023. [Epub ahead of print]. |

