 |
Q:
I have a new spectral-domain optical coherence tomographer (SD-OCT) that I used to perform an optic nerve evaluation on a patient. The test shows a very thin nerve fiber layer (NFL) and ganglion cell layer thinning. The patient has para-nasal visual field defects in both eyes. Her discs look normal, her IOP is 15mm HG OU and there is no family history of glaucoma. Is this low-tension glaucoma?
A:
Brian Den Beste, OD, of LP Eye Consultants in Orlando, had the same thing happen to him recently. A 47-year-old Caucasian female came to his practice. He examined the patient and confirmed the OCT and visual field findings that the referring optometrist found. The patient’s history revealed that she has been on blood pressure meds for the past eight years, and she admitted to never having perfect vision. Her glasses revealed a low hyperope prescription, with 20/25 vision OU.
Her pachymetry measurements were normal at 520mm. Her fundus exam revealed healthy optic nerves with 0.3 central cups and no visible optic nerve drusen. The average retinal NFLs showed symmetry but were both thin at 66µm. The macular ganglion cell complex (GCC) was also extremely thin with an average thickness of 60µm. The Matrix visual field was also reviewed and showed nasal loss OU.
The horizontal B-scan showed a “reverse divot” OU, without vitreal macular traction but with a “bump” instead of a depression. This correlated with the patient’s history of long standing vision less than 20/20.
Dr. Den Beste says this finding is not uncommon in patients who are referred to him as glaucoma suspects. “It’s easy to throw out GCC and NFL data when there is macular traction and the tissue is obviously distorted,” he adds. “It is more difficult when there are subtle changes that don’t seem to make sense.”
OCT Assurance
While optic nerve drusen or tilted disc syndrome can cause unusual NFL findings and nasal field loss, the patient didn’t have evidence of that. Optic nerve hypoplasia is also in the differential when the discs are less than 1.5mm. Dr. Den Beste’s patient had normal disc diameters. A prior history of optic neuritis would obviously affect both the ganglion cells and the overall nerve fiber thickness but often is accompanied by disc pallor.
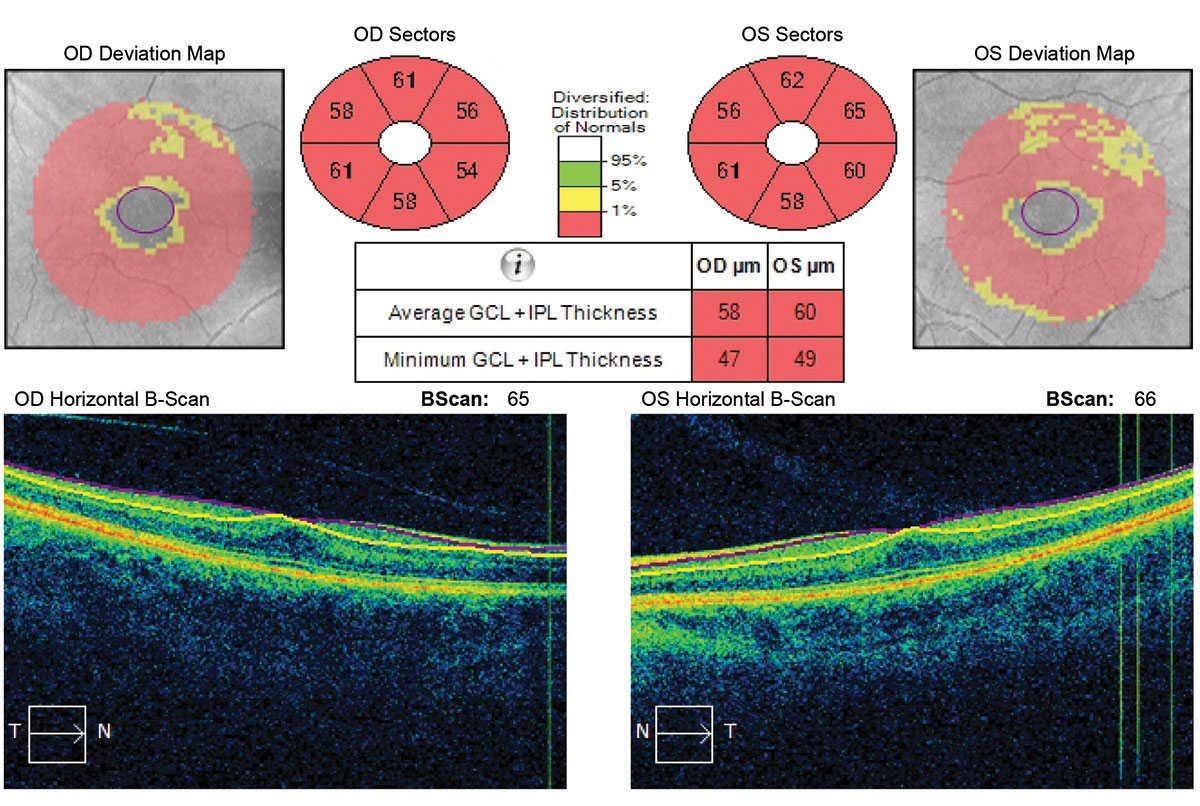 |
| Ganglion cell analysis revealed a reverse foveal pit and no vitreal macular traction. Click image to enlarge. |
Similar findings are present with compressive lesions in the visual pathway. Diabetic retinopathy can also greatly affect OCT data. None of these associated findings were pertinent in this case.
“We see a lot of patients who are referred as glaucoma suspects with asymmetric cupping or bilateral large cups, and the OCT is a great tool to rule in or out glaucoma,” Dr. Den Beste says. Many of these individuals who have asymmetric cups also have asymmetric discs, so the “disc area” is the first item he looks at when evaluating the OCT print out. “It’s easy with funduscopy to note a difference in cup size but not so easy to assess disc size,” he says.
This patient was relieved to know she didn’t have a progressive disease, like primary open-angle glaucoma, but she is due to have a repeat OCT and visual field exam in six months to make sure her findings are not progressive. The beauty of an objective test like OCT is that it is repeatable, and Dr. Den Beste is predicting that the results won’t change.
The chief lesson here: don’t just look at the color key with OCT. “Seeing red” may lead you to an incorrect diagnosis. Look at other findings to be sure that your patient really has glaucoma. “The OCT B-scan images will assist your diagnostic decisions,” says Dr. Den Beste. “They help delineate ganglion cell damage from a macular etiology as opposed to an optic nerve etiology.”

