 |
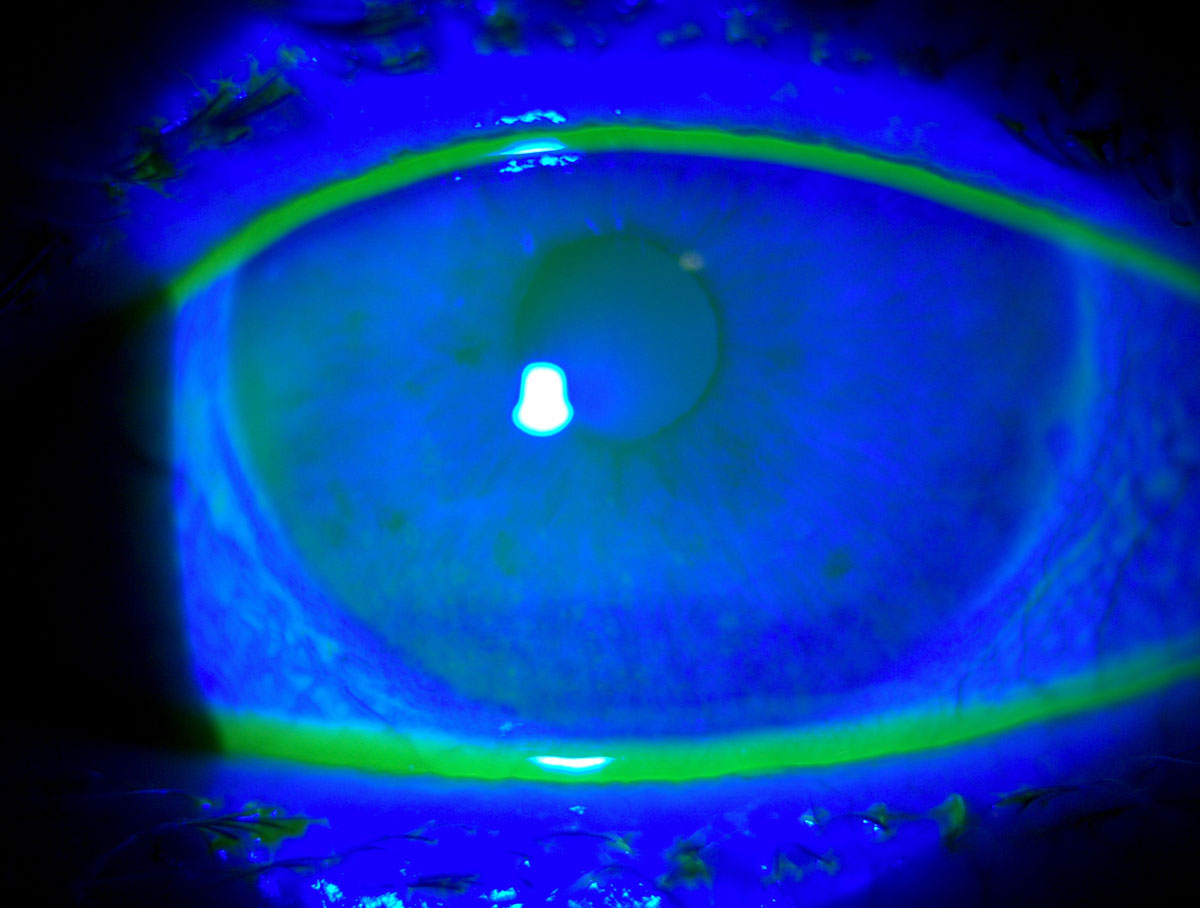
| The influence of depression may be one factor leading to a mismatch between dry eye signs and symptoms. Photo: Michelle Hessen, OD. Click image to enlarge. |
The list of potential ocular manifestations associated dry eye disease (DED) are non-specific, comprising redness, burning, stinging, foreign body sensation, photophobia and pruritis. While DED diagnosis is dependent upon reports of ocular symptoms and measurements of signs, literature has not clearly demonstrated a link between signs and symptoms. One new study assessed this need by determining correlations among symptoms and signs of dry eye in the Dry Eye Assessment and Management (DREAM) study.
Moderate to severe dry eye was assessed in a total of 535 patients, using the Ocular Surface Disease Index (OSDI) for symptoms. Four DED signs were tested in both eyes, including conjunctival lissamine green staining, corneal fluorescein staining, Schirmer’s testing and tear breakup time following standard protocol at baseline and follow-up visits at three, six and 12 months.
The researchers found OSDI scores at baseline did not correlate with signs, but OSDI subscale score of ocular symptoms was weakly associated with corneal staining score and Schirmer test score. There were correlations among the four signs. Correlations among changes in signs and symptoms were weaker, with the highest correlation being of change in conjunctival staining and corneal staining. Overall, the results yielded low correlation of DED symptoms with signs, even weaker correlation among changes in symptoms and signs, but low to moderate correlation among the four signs.
The study researchers as part of their discussion relay that the weak associations observed may be due to comorbidities that could increase the perception of ocular symptoms in dry eye patients, such as with neuropathic pain or other chronic pain conditions. They also mention that although the OSDI subscale and ocular symptoms displayed weak association with corneal staining and Schirmer’s test scores, these correlations did not differ with sex or depression status, although were stronger in patients with Sjögren’s syndrome.
Similarly, despite low correlations among the four signs of dry eye, the highest correlation was seen with corneal and conjunctival staining and was higher in the population of patients with Sjögren’s.
The authors discuss how mental health disorders can also contribute to the symptom level experienced with DED which are not consistent with the severity of DED signs. One previous study outlined that DREAM participants with depression experienced more severe dry eye symptoms than those without. Another observed depression to be more prevalent in DED patients and was associated with symptoms of dry eye but not signs. The current study found that the correlation was weaker between dry eye signs and symptoms for those with depression than those without. As such, this may play a part in some of the discordance seen between signs and symptoms, but offers no complete explanation, and is likely not the majority of causation of these findings.
These observations prompt the authors to convey that “better objective minimally invasive metrics that capture biologic changes in the eye might lead to a better assessment of the severity of ocular surface changes in DED and perhaps a better correlation with symptoms.”
Tawfik A, Pistilli M, Maguire MG, et al. Association of dry eye symptoms and signs in patients with dry eye disease. Ophthalmic Epidemiol. August 17, 2023. [Epub ahead of print]. |

