How often do you find yourself with a patient in your chair with an exhaustive list of dry eye symptoms, not knowing where to begin? It can be overwhelming for both you and the patient, which is why it’s imperative to have proper knowledge of dry eye causes and treatments in your diagnostic toolkit. After all, as eyecare professionals, it’s our job to produce happy patients.
Dry eye disease (DED) is a multifactorial condition that can complicate treatment; we must first determine the underlying causes and then marry them with treatment options that make sense for the patient’s lifestyle, budget and expectations. Do symptoms arise from too much screen time, an undiagnosed systemic disease or a medication they failed to list on their paperwork? Does this patient simply need prescription drops or do they require placement of an amniotic membrane or thermal pulsation device treatments? The list of symptoms is as long as the available treatments.
Our aim in this article is to help you incorporate dry eye treatment into your practice while graduating your management from basic to advanced, without having to purchase expensive equipment. In the end, you will have happier patients while also increasing your practice revenue.
Adding Dry Eye to Your Practice
The Tear Film and Ocular Surface Society Dry Eye Workshop II (TFOS DEWS II) report provides evidence-based rationale for diagnosis and treatment and gives those new to DED a more organized approach. The TFOS DEWS II diagnostic methodology report provides a comprehensive review of tests to be used for diagnosis, monitoring and to guide treatment. Coupled with the Management and Therapy report, the collective work ensures the most targeted therapy and monitoring plan.
Because you are treating a condition that requires more chair time and different billing practices, don’t try to fit it all into one visit; have them return for a follow-up when they need additional care. If the patient originally presented for routine care using their vision plan, they will need to return for a separate visit for the additional testing to be billed through their insurance.
 |
|
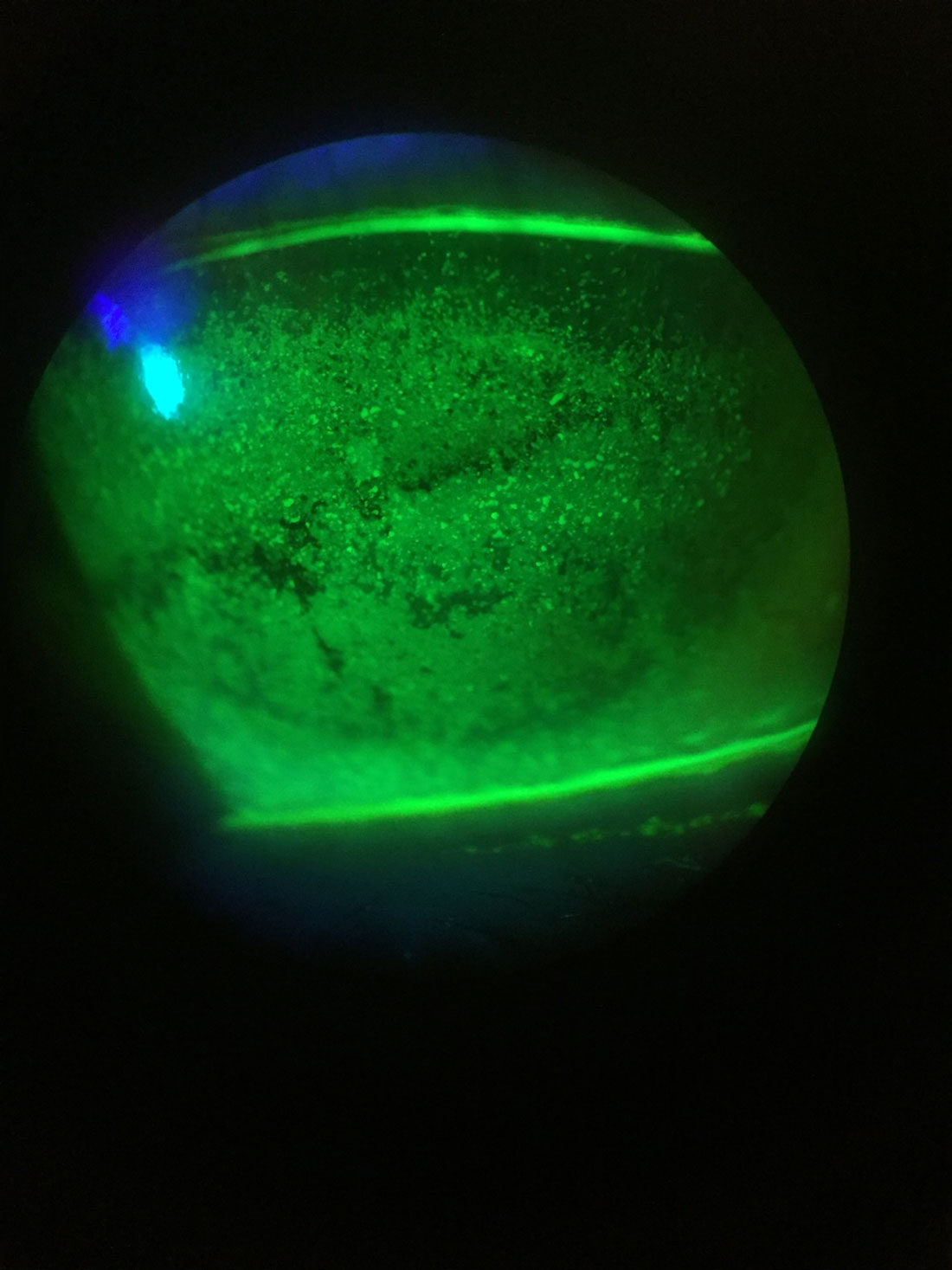
Fig. 1. Slit lamp image of diffuse punctate corneal staining. Click image to enlarge. |
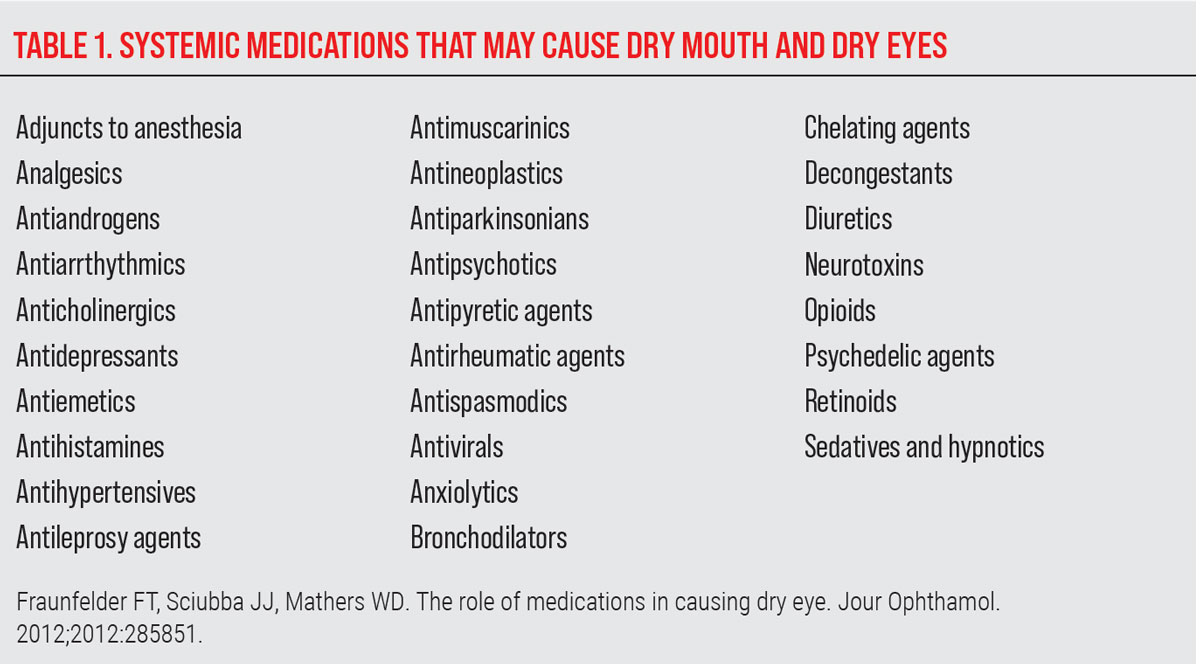
Get to Know Your Patients
Make sure you’ve gathered comprehensive information from your patient. Are their symptoms occupational, whether it’s too much computer time or working in harsh environmental conditions? Do they have other symptoms such as dry mouth or eye pain, or have they had recent bloodwork to rule out autoimmune conditions? They could also be taking certain oral medications, which may interfere with goblet cells, meibomian glands and ocular surfaces of the conjunctiva and cornea (Table 1).1 Is your patient on topical glaucoma medications? A study found these induced meibomian gland dysfunction (MGD) and were associated with a 50% incidence of dry eye.2
Thoroughly getting to know your patient helps involve them in their treatment, understand how their daily routine contributes to their discomfort and allows you to find the best regimen to improve their condition.
Education is Key
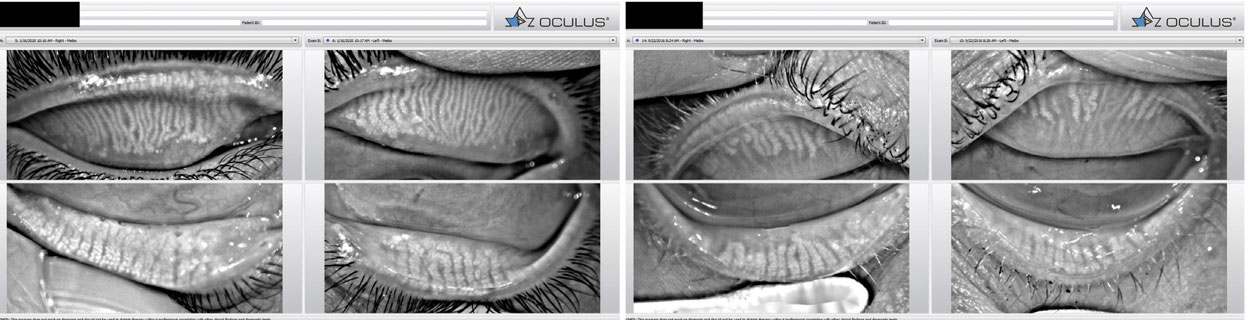
Using diagnostics helps add a greater level of understanding of these patients. Showing or explaining their results allows them to be more accepting to your treatment recommendations. This could be done with your phone at the slit lamp or you could invest in a corneal topographer with keratograph that allows you to evaluate meibography, non-invasive tear break-up time (TBUT) and tear meniscus height (Figure 1). When patients are shown these images, they typically understand what is happening on the ocular surface and it allows them to be part of their own dry eye treatment journey.
Treatment Regimen
The next step is determining what treatments are best for your patients, which range from beginner to intermediate to advanced.
TIER 1: (BEGINNER)
• Prescription eye drops. These include cyclosporine (Restasis [0.05%], Allergan), Cequa (0.9%, [Sun Pharmaceuticals]), Klarity-C (0.1%) and lifitegrast (Xiidra, Novartis).
• Ointments. These include Refresh PM, Systane Nighttime, erythromycin and GenTeal Tears.
• Warm compresses. A popular option is the Bruder Moist Heat Eye Compress.
• Lid scrubs/cleansers. These include Avenova, Ocusoft, We Love Eyes, Zocular, Optase and Cliradex.
• Tea tree eye cleansers. These include Cliradex, We Love Eyes and Eye Eco.
• Steroids. These include loteprednol (Eysuvis [0.25%], Kala Pharmaceuticals), Lotemax SM (0.38%, Bausch + Lomb) and Alrex (0.2%, Bausch + Lomb).
• Nasal spray. There’s now a treatment called Tyrvaya (varenicline, Oyster Point Pharmaceuticals).
• Eye seals/sleep masks. Options include Eye Eco and Sleep Tite.
Start basic with a slit lamp and begin assessing the lids and lashes where you first see ocular surface inflammation. Approximately 20% of patients have ocular findings before dermatologic evidence of rosacea, (which will be further discussed in Tier 3).3 Warm compresses and lid scrubs are easy treatments that patients can add to their daily routine.
A significant number have Demodex infestation, including about 45% of patients with blepharitis, 84% of patients 60 and older and 100% of patients over the age of 70.4,5 Patients with rosacea have nine times the average rate of infestation.6 Keep in mind that inflamed eyelid margins and mechanical irritation of the lids are not always present.
 |
Fig. 2. Tyrvaya is the first FDA-approved nasal spray to treat DED. Click image to enlarge. |
Another thing to look out for is nocturnal lagopthalmos, the inability to close the eyelids while sleeping. We always ask patients if their dryness worse is the morning. If so, we consider overnight therapies such as ointment or eye seals from Eye Eco.
Tyrvaya, the first FDA-approved nasal spray for the treatment of DED, activates the trigeminal parasympathetic pathway, resulting in improved basal tear film production (Figure 2). A study showed that, at week four, 47% of patients improved their Schirmer’s score by equal to or more than 10mm from baseline, compared with 14% and 28% of vehicle-treated patients, respectively.7
Inflammation plays a significant and central role in the pathogenesis of dry eye.8 Steroids can be our friend for a short-term therapy, including Eysuvis, which is the first steroid to be FDA-approved for dry eye flare-ups.
The hardest part about treating patients is setting expectations. Often they feel like we should be able to fix 50 years of dry eye with a few drops for a few weeks. However, a study showed that lifitegrast demonstrated significant improvement in patient’s signs and symptoms who suffered from inflammatory MGD.9
Prescribing cyclosporine or lifitegrast won’t create an overnight fix, though. Inform your patients that dry eye is a war, a chronic progressive disease and that these drops, most of the time, require long-term commitment.
Make it convenient for your patients by selling products like warm compresses, lid scrubs/cleansers, ointments or artificial tears in your office. Stock brands you believe in and think are the best fit for your patients; specifying specific brands and products increase patient buy-in and compliance.
 |
Fig. 2. Prokera Slim being inserted on a patient. It is a corneal bandage device that reduces inflammation, prevents scarring and helps the ocular surface heal. Click image to enlarge. |
TIER 2: (INTERMEDIATE)
• Amniotic membranes. Options include the cryopreserved Prokera (BioTissue), as well as several dehydrated membranes (e.g., BioDOptix, Integra Lifesciences; AmbioDisk, Katena; AcellFX, Akorn).
• Therapeutic meibomian gland expression. Mastrota Meibomian Gland Paddle (Medi Instruments), Collins Meibomian Expressor Forceps (Sigma Pharmaceuticals) and Meibomian Gland Evaluator (Johnson & Johnson).
• Microexfoliation devices. (BlephEx).
• Punctal plugs.
Temporary occlusion. These include Vera180 (Lacrivera) and Soft Plug Extended Duration (Oasis Medical).
Permanent occlusion. These include SmartPlug (Medennium) and FormFit (Oasis Medical).
Surgical closure. This includes cauterization, punctal plug suturing and canalicular ligation).
You can get a jump start on treating the ocular surface with amniotic membranes. In a dry eye study with 160 participants, 95% said cryopreserved amniotic membranes healed their eye and 81% said it improved their vision.10 Usually, amniotic membranes are used clinically one eye at a time since they obscure vision. Prokera Clear heals the cornea and maintains visual acuity with the inclusion of a clear central aperture. Additionally, consider that if you find the cornea to be moderately to severely dry, it may require you to use more than one membrane treatment.
To help keep tears on the surface longer, consider using punctal plugs, which block the openings to the drainage ducts to improve ocular surface tear retention.
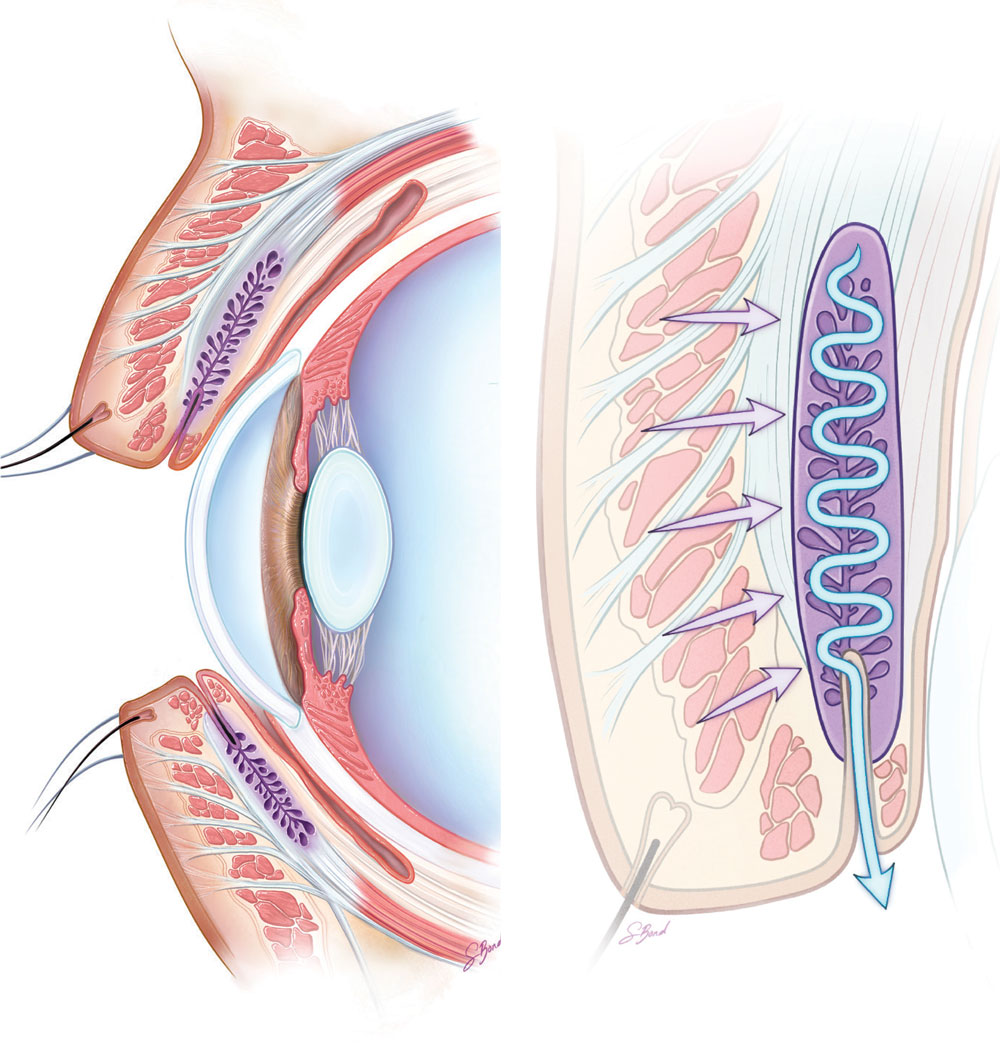
It’s been shown that hyper-keratinization of the meibomian gland duct is a primary cause of MGD; once the ducts are obstructed, the glands themselves atrophy (Figure 4).11 Historically, doctors have first tried therapeutic expression of the glands to increase quality and promote healthy meibum production. This could be attempted with a topical anesthetic and an expressor, such as the Mastrota Meibomian Gland Paddle.
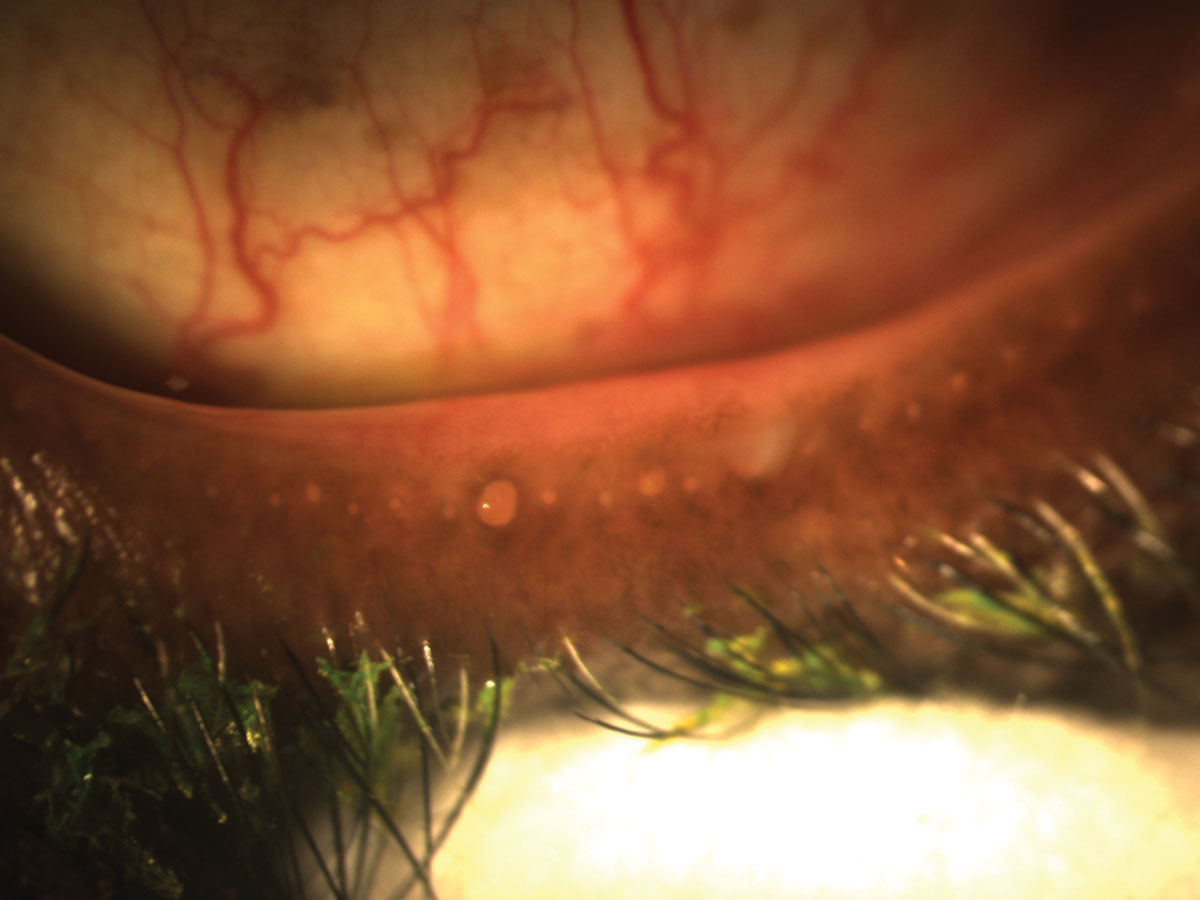 |
Fig. 3. Obstructed meibomian glands respond to digital pressure by releasing thickened, cloudy meibum. Click image to enlarge. |
Blepharoexfoliation is a painless procedure performed in-office that cleans the eyelids margins, removing bacteria and biofilm (Figure 5). BlephEx has been shown to improve eyelid health: increasing TBUT, reducing inflammation and enhancing meibomian gland function.12 It is also a reasonable clinical approach for use on noncompliant MGD patients. We could consider doing therapeutic expression and/or BlephEx with a thermal treatment, which brings us to our advanced level.
 |
| Fig. 4. The BlephEx device or in-office removal of eyelid scurf and bacterial debris, which can cause inflammatory lid disease. The rotating pad buffs away the biofilm and other lid debris to prevent blepharitis. Click image to enlarge. |
TIER 3: (ADVANCED)
• Thermal pulsation devices. These include TearCare (Sight Sciences), LipiFlow (Johnson & Johnson Vision), Systane iLux (Alcon), Thermoflo (MiBo Medical Group) and EyeXpress (Holbar Medical Products).
• Intense Pulse Light Therapy (IPL). These include Lumenis Optima IPL (Lumenis) and LacryStim IPL (Quantel Medical).
• Low-level Light Therapy (LLLT). These include Eye-Light (Espansione Group) and Equinox LLLT (Marco).
• Radio Frequency energy application. A device called TempSure (Cynosure) enables this.
• Scleral lenses. These create a temporary reservoir for medication and lubricants and include DigiForm (TruForm Optics and Contamac), Onefit (Blanchard Contact Lenses), Boston IV (Bausch + Lomb) and PROSE (BostonSight).
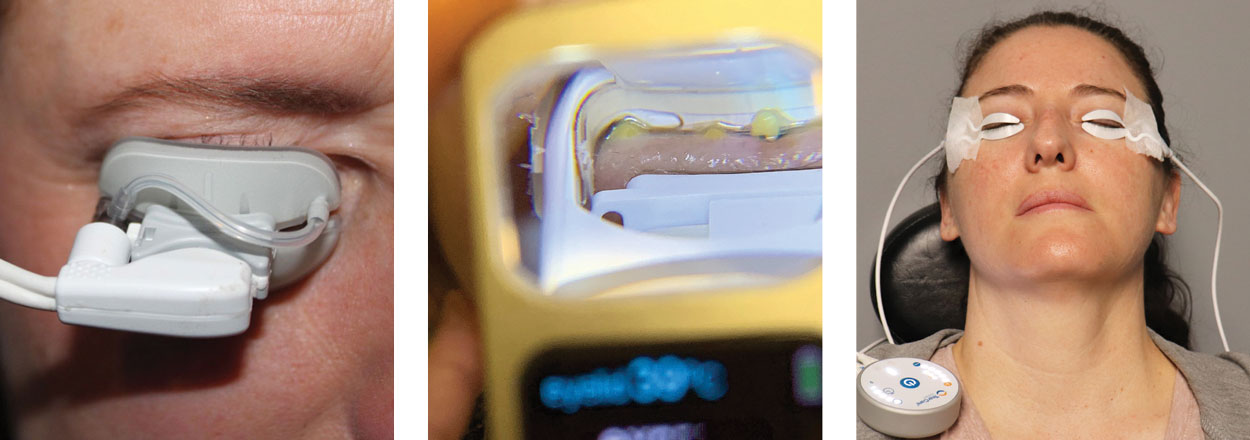 |
| Fig. 5. In-office procedures to heat and express the meibomian glands yield many benefits. From left to rightL iLux, LipiFlow and TearCare. Click image to enlarge. |
We have arrived at the point of adding equipment to your practice to truly designate ourselves as a comprehensive dry eye clinic. When advancing into Tier 3 treatment options, consider the increased financial commitment for both your practice and patients. While some treatment options can be billable with correct diagnosis, many are not. Before purchasing new equipment, it’s important to study the cost, typical reimbursement or out-of-pocket costs for the patient, as well as proper diagnosis requirements. Once you have the whole picture, it’s easier to decide whether your clinic will benefit from adding extra equipment and procedures.
Warm compress care at home can be challenging for patients to keep the glands heated up for a sufficient amount of time and at the right temperature. New technology has created the opportunity for thermal pulsation devices to make this less challenging. (Figure 6). These wearable eyelid paddles provide targeted and adjustable thermal energy and pressure to the meibomian glands. The Olympia clinical trial data for TearCare showed a statistically significant improvement in both TBUT and meibomian gland secretion score, as well as a statistically significant decrease in Ocular Surface Disease Index score.13
Another newer technology is LLLT, which uses specially designed LED light to gently apply periorbital heat to the eyelids to treat MGD, blepharitis, chalazia and Demodex. Treatment consists of four consecutive applications, which last 15 minutes; the sessions are separated by 48 to 72 hours. It’s been shown that LLLT increases the amount of tear volume and decreases neutrophils and the level of inflammatory cytokines significantly in non-human trials.14
Radio frequency energy application is a non-invasive treatment that stimulates collagen production by delivering high frequency electrical currents, which generates heat to the surface of the skin. The heat promotes not only improvement in skin tone but also reduces inflammation around the eye and improves lipid expressions into the tears. It only takes around 10 to 20 minutes to complete.
IPL has been used in dermatology for several years as a treatment for rosacea and now has been incorporated into eye doctor’s offices to treat ocular rosacea (Figure 7). The light emitted causes blood cells in the abnormal telangiectasias to absorb the light, coagulate and close the blood vessels. Rosacea is a condition where these abnormal blood vessels secrete inflammatory mediators over time that damage the meibomian glands.15 Ultrasound gel is applied to the face from tragus to tragus, including the nose. Complete two full passes across the ultrasound gel and then you can then express the patient’s upper and lower glands. The protocol calls for four visits repeated about every 30 days. After these initial treatments are completed, the patient can then return for maintenance in the future when they become more symptomatic.
 |
Fig. 6. Dr. Wiechmann demonstrates the use of IPL on a patient. Click image to enlarge. |
Let's Get Down to Business
When deciding to bring any new dry eye treatment into your office, it’s important to consider the cost of acquisition and return on investment. Another thing to consider is adding marketing and advertising to acquire dry eye patients. Questions to ask:
• Do you have a page on your website dedicated to dry eye treatments?
• Do you use email marketing to target your dry eye patients, letting them know about the latest treatments?
• What systems are you using to make sure your patients are returning for their follow-up visits?
• Do you offer financing for non-billable treatments, and do you have someone in your office who goes over pricing? It’s critical to have someone in your clinic who can explain the potential out-of-pocket expense for patients, depending on their insurance plan’s allowables and deductibles.
• Do you have a system to follow-up if they don’t sign up for anything?
All of these, if done well, can lead to a profitable dry eye practice, regardless of the treatments that you have in your office.
 |
| Fig. 7. X-rays of the eyelids of a patient with meibomian gland dysfunction. Click image to enlarge. |
Become Committed
Some may believe treating dry eye is a hassle, as it requires more chair time and think it won’t pay off in the end, but I feel this isn’t the case any more. DED is increasingly more common and the more you treat it, the easier it gets. Don’t wait until the condition becomes severe, as this makes it much more challenging and frustrating for you and your patients.
Our profession is changing and we need to increase our awareness of the treatments we are capable of providing; we can become patient’s go-to doctor for dry eye care. This is also an easy way to shift to a more medical practice model. Once you are committed and experienced in medical billing, you can expand your offerings, further growing your revenue. You’ve now graduated from being a primary care optometrist to a medical optometric practice. At this level, revenue growth can become exponential.
 |
| Fig. 8. The role and dysfunction of meibomian glands in dry eye. Click image to enlarge. |
Takeaways
Never stop learning! Technologies and treatments are always improving and keeping up with these advancements is what sets you apart from your peers. There are ample continuing education courses on DED as well as workshops conducted by leaders in the dry eye landscape.
Remind yourself and your patient that you can’t throw the kitchen sink at DED all at once. Start with a few treatment options and get your patient into a routine. Then, reassess their new daily symptoms and see what needs to be added or removed. Not every treatment works for everyone—don’t be afraid to change it up. Remind them that DED is never “cured” forever; you are managing their symptoms and preventing them from becoming more severe.
Dry eye management requires a positive attitude. Many of my patients come to me thinking they have tried everything under the sun and are about to give up and accept that pain and suffering is their only option. There are many factors that can cause their problems and trying to fix them all might not be practical, but if you take the time to treat the things within your control, it can be the most rewarding time spent with someone in your chair.
Once you bring your patients relief, they can end up being some of the most grateful people leaving your practice, eventually referring their friends and family. Become a dry eye hero—your patients will thank you!
Dr. Wiechmann is an assistant adjunct clinical professor at the University of the Incarnate Word Rosenberg School of Optometry and faculty of the Refractive Surgery Alliance Grands Rounds Collaborative Care Series. She practices at Parkhurst NuVision, an OD-MD integrated care practice that specializes in refractive surgery and is a Fellow of the American Academy of Optometry. She has no financial disclosures.
| 1. Fraunfelder FT, Sciubba JJ, Mathers WD. The role of medications in causing dry eye. Jour Ophthalmol. 2012;2012:285851. 2. Viso E, Gude F, Rodríguez-Ares MT. The association of meibomian gland dysfunction and other common ocular diseases with dry eye: a population-based study in Spain. Cornea. 2011;30(1):1-6. 3. Thiboutot D, Anderson R, Cook-Bolden F, et al. Standard management options for rosacea: the 2019 update by the National Rosacea Society Expert Committee. J Am Acad Dermatol. 2020;82(6):1501-10. 4. Zhao YE, Wu LP, Hu L, Xu JR. Association of blepharitis with Demodex: a meta-analysis. Ophthalmic Epidemiol. 2012;19(2):95-102. 5. Post CF, Juhlin E. Demodex folliculorum and blepharitis. Arch Dermatol. 1963;88:298-302. 6. Chang YS, Huang YC. Role of Demodex mite infestation in rosacea: a systematic review and meta-analysis. J Am Acad Dermatol. 2017;77(3):441-7.e6. 7. Wirta D, Vollmer P, Paauw J, et al. Efficacy and safety of OC-01 (varenicline solution) nasal spray on signs and symptoms of dry eye disease: the ONSET-2 Phase 3 randomized trial. Ophthalmology. 2022;129(4):379-87. 8. Pflugfelder SC. Antiinflammatory therapy for dry eye. Am J Ophthalmol. 2004;137(2):337-42. 9. Tauber J. A six-week, prospective, randomized, single-masked study of lifitegrast ophthalmic solution 5% versus thermal pulsation procedure for treatment of inflammatory meibomian gland dysfunction. Cornea. 2020;39(4);403-7. 10. McDonald M, Sheha H, Tighe S, Janik SB. Treatment outcomes in the Dry Eye Amniotic Membrane (DREAM) study. Clin Ophthalmol. 2018;12:677-81. 11. Knop E, Knop N, Millar T, et al. The international workshop on meibomian gland dysfunction: eeport of the subcommittee on anatomy, physiology and pathophysiology of the meibomian gland. Invest Ophthalmol Vis Sci. 2011;52(4):1938-78. 12. Connor CG, Choat C, Narayanan S, et al. Clinical effectiveness of lid debridement with BlephEx treatment. Invest Ophthalmol Vis Sci. 2015;56(7):4440. 13. Loh JM, Trattler WB, Dhamdhere KP, et al. A novel, targeted open eye thermal therapy and meibomian gland clearance in treatment of dry eye: A randomized control trial (OLYMPIA). Virtual American Society of Cataract and Refractive Surgery Annual Meeting. May 16, 2020. 14. Goo H, Kim H, Ahn JC, Cho KJ. Effects of low-level light therapy at 740 nm on dry eye disease In Vivo. Med Laser. 2019;8(2):50-8. 15. Toyos R, McGill W, Briscoe D. Intense pulsed light treatment for dry eye disease due to meibomian gland dysfunction; a three-year retrospective study. Photomed Laser Surg. 2015;33(1):41-6. |

