Earn New Surgical SkillsOptometric surgery is increasingly becoming a core responsibility of the profession. Today, 17 states (and counting) allow ODs to perform laser or other minor surgical procedures. Here to offer tips and advice on surgery implementation and technique is the December 2023 issue of Review of Optometry, the magazine's 30th annual surgery report. Inside, experts offer advice on performing SLT, equipping your office for surgery and handling complications of in-office procedures, along with a review of the newest IOLs on the market. Check out the other articles featured in the December issue: |
As scope expansion efforts continue across the country, the number of optometrists who can practice to the full extent of their expertise and ability continues to grow. Therefore, ODs must be prepared to incorporate these procedures into clinical practice.
“It is important for every doctor of optometry to consider the thousands of person hours it has taken to move optometry forward,” notes Luke Brog, OD, who practices in Wyoming. “Many are aware because they have been on the front lines. It is in the best interest of your patients and our profession to have as many doctors offering these services in their offices as possible.” Dr. Brog urges ODs, “If your state has already gained these privileges, find a procedure and start offering it. If you don’t have them yet, work with your state board and state legislators to help move the legal efforts forward.”
Once an optometrist has decided they want to perform minor surgical procedures in their practice, they must take the necessary steps to set up themselves—and their patients—for success. That begins by equipping your office with the necessary tools.
Below, we will delve into what you need for various procedures—including incisions, injections, selective laser trabeculoplasty (SLT), YAG capsulotomy and laser peripheral iridotomy (LPI)—as well as discuss the considerations behind these purchases. Seasoned ODs share their own experiences and offer insights on specific equipment needs, including non-negotiables and often overlooked resources, touch on the pros and cons of various options and discuss navigating big-ticket purchases.
Incisions and Injections
When performing minor surgical procedures, such as intralesional injections, benign lesion removal and biopsies, there are a variety of tools required for success, some of which are must-haves while others are helpful but not absolute necessities.
|
Fig.1. Example of a radiofrequency unit (Soniquence) that can be used for minor optometric procedures such as benign lesion removal as well as for aesthetic purposes like the reduction of wrinkles and fine lines. Photo: Nathan Lighthizer, OD. Click image to enlarge. |
“The biggest ticket item is the radiofrequency device (Figure 1),” notes Nathan Lighthizer, OD, associate dean at NSU Oklahoma College of Optometry. “However, while a laser is required for laser procedures, a radiofrequency device, like an Ellman or Soniquence unit, even though it is often the preferred device, is not an absolute necessity for lesion removal. There are many different ways to remove lesions, including surgical scissors and scalpels.”
While Dr. Lighthizer has found having a radiofrequency device to be very beneficial and recommends that optometrists consider it, he recognizes that cost is a factor. These devices, he notes, typically run between $10,000 and $20,000 and can get much higher in cost if the aesthetics components of the radiofrequency device are added in.
There are a number of electrosurgical devices available, according to Dr. Brog, who notes that the level of investment really depends on the doctor’s preference. “For all practical purposes, you can purchase a basic unit and it will do everything you need it to in your office,” he advises.
Dr. Brog, who opted to purchase a used Ellman unit, says, “If you get them used, make sure that you can get the electrodes for the equipment you purchase. Some companies have discontinued certain models and the electrodes are no longer available.” He cautions, “You will also need a smoke evacuator unless you want your entire office to smell from the procedure.”
Whether or not they decide to invest in a radiofrequency device, optometrists who want to perform incisions and injections should have the following tools on-hand:
- Surgical scissors (Westcott, Vannas, etc.) in varying sizes (Figure 2)
- #11 blade scalpel (either as single-use disposable sterile scalpels that cost about $0.70 a piece or a stainless steel reusable blade handle for approximately $10 with disposable #11 surgical blades at $0.05 a piece)
- #15c blade scalpel
- Featherblade scalpel
- Forceps (both toothed and non-toothed)
Other must-haves include a 2.5mm or 3.0mm trephine blade, 2.0mm-5.0mm punch biopsies, needle drivers and eyelid speculums, according to Dr. Lighthizer. If an optometrist plans to offer chalazion removals, they will need chalazion clamps (small- and medium-sized; Figure 3) and chalazion curettes (serrated and non-serrated).
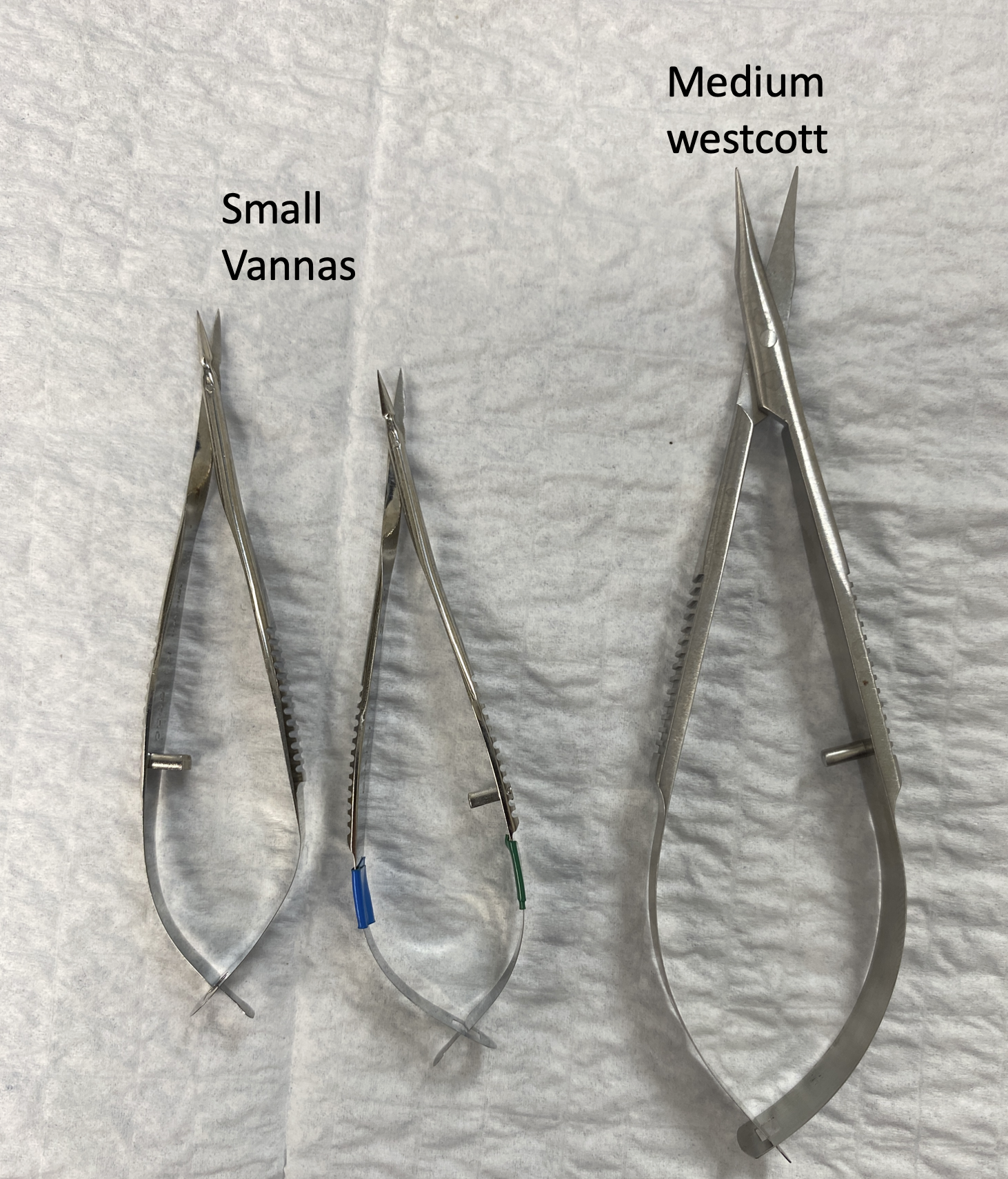 |
| Fig. 2. Different varieties and sizes of surgical scissors that can be used to perform in-office eyelid procedures. Photo: Nathan Lighthizer, OD. Click image to enlarge. |
Chris Wroten, OD, who practices in Louisiana, recommends small, curved-tip Vannas scissors. “They are great for cutting the stalks of small lid lesions, trimming lashes and cutting sutures prior to removal,” he says. Dr. Wroten adds that while single-toothed tissue forceps are sometimes overlooked, they can be very useful when performing a lesion removal, as tissue often gets wet and regular forceps will not adequately grasp.
 |
| Fig. 3. Clamps are necessary for chalazion/lesion removal to prevent the mass from moving during the procedure. Photo: Jackie Burress, OD, and Rodney Bendure, OD. Click image to enlarge. |
When considering where to get the various instruments needed for in-office incisions and injections, keep in mind that there are surgical sets available that have all the recommended instruments for in-office procedures, including forceps, scissors, scalpels, needle drivers and more (Figure 4).
For incisions and injections, Dr. Brog repurposes job trays as surgical trays and prepares them ahead of time. “The trays include povidone-iodine swab sticks or alcohol swabs for preparing the lesion, cotton swabs, gauze pads to clean off the electrode during procedure, electrodes of various types (loop, diamond, ball and broad needle), triple antibiotic ointment, biohazard specimen bags and small bandages,” he says. “We also have a number of things for infiltration anesthesia, including needles and syringes, prepared on the trays.”
Another important component is personal protective equipment, including gloves and masks. Staff should be trained on how to properly handle needles and biohazard material, says Dr. Brog. “It has been proven that as you remove lesions with electrosurgery, there are particles in the smoke. Some that have been isolated are HPV and HIV. You need to protect yourself and your staff,” he cautions.
Biopsies are another type of procedure optometrists must be equipped to handle. While not every lesion requires a biopsy, if there are concerns around malignancy, ODs must be prepared for when these cases arise. “You should contact your local pathology lab and get the necessary biopsy kits,” says Dr. Lighthizer. “If you are removing eyelid lesions, you have to have the ability to biopsy.”
Other inexpensive—yet important—items are needles and syringes, both which have a wide selection to choose from. In addition to product availability, deciding which to purchase will depend on your personal preferences and the specific needs of your patients. The most common needles are 18-, 25- and 30-gauge, according to Dr. Lighthizer, who notes that while some optometrists may opt for different sizes, these three will serve the majority of your needs.
 |
Fig. 4. Example of an in-office surgical instrument set that has all the recommended tools needed to successfully perform simple procedures (scissors, scalpels, forceps). This may be a wise investment for ODs who are just beginning the process of equipping their practice for these services. Photo: Nathan Lighthizer, OD. Click image to enlarge. |
“The eyelid tissue is very thin, so it is important to use small-gauge needles,” says Dr. Brog, adding that he would opt for the 30-gauge needle to start. “The length is also important; I prefer one-half inch,” he says. “You could easily use longer ones if you would like.” To ensure the needle is sharp and has an easier time penetrating the tissue, Dr. Brog says he likes “to draw the material up with a 25-gauge needle and then change it before I infiltrate.” He notes that you can certainly use a larger needle than a 25-gauge to draw faster; Dr. Brog’s rationale for choosing this size is that it’s the same as he uses to inject chalazia, so it’s already in his cupboard. Regarding the syringe size, he says that he uses a 1mL because “it is small and easy to use around the eyes.”
Magnification is another equipment consideration to keep in mind. As with most equipment, optometrists have a selection of high-cost and more economical options, including surgical microscopes, surgical loupes and headset magnifiers. “While not a requirement, magnification tools are very important and they don’t have to come with a high price tag,” says Dr. Lighthizer, pointing out that there are options available for as little as $30.
There are several other miscellaneous items optometrists should have available when performing incisions and injections at their practice. Some of these include Mayo stands with sterile drapes, a sharps container for used needles and other sharp objects, a camera to take photos pre- and post-procedure, biohazard service, small steam autoclave or chemical disinfection/sterilization unit for reusable surgical instruments, gauze, cotton tip applicators, alcohol wipes, sterile saline, Wek-Cel sponges, antibiotic ointment and a scrub pad to clean electrodes (optional).
Agents to have on-hand include lidocaine with and without epinephrine, betadine, sodium bicarbonate as a buffering agent and Kenalog-40 (triamcinolone acetonide, Bristol-Myers Squibb) for injecting chalazia (see table below for a full list of items required for these procedures).
What You Need to Perform Eyelid Incisions and Injections
|
Laser Procedures
The price tag of offering laser procedures in your practice certainly exceeds that of incisions and injections. There are a variety of tools optometrists need to have in their clinical practice to successfully perform laser procedures. This starts with a significant investment: the laser itself. Depending on the type (YAG, SLT or YAG/SLT combination laser) and brand, the price can range from $20,000 to $55,000, according to Dr. Lighthizer.
While Dr. Brog acknowledges that lasers are an investment, he believes it is worth the high price tag given the impact for not only patients, but also optometric practice as a whole. “This increased scope of practice has been hard fought for and the more optometrists who are doing these procedures, the better it is for our patients and our profession,” he says.
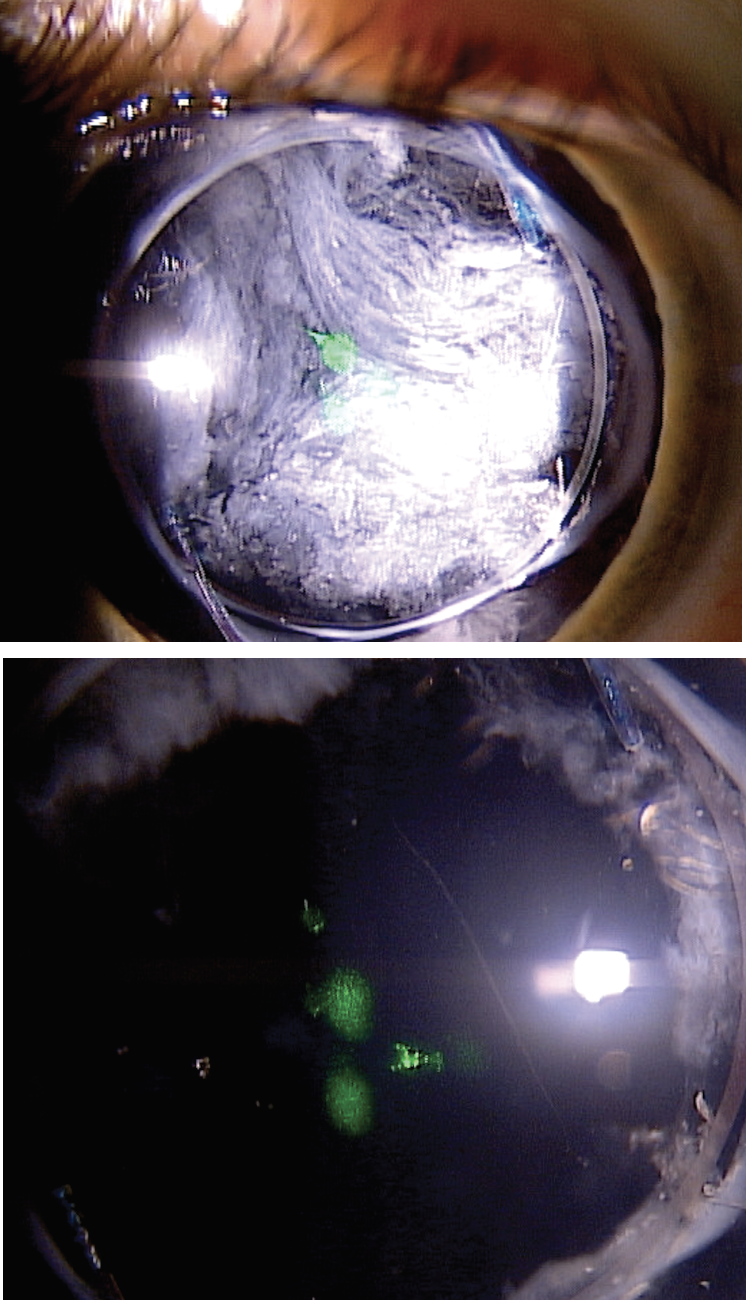
|
Fig. 5. Patient before (top) and after (bottom) YAG posterior capsulotomy. Photo: Nathan Lighthizer, OD. Click image to enlarge. |
“Most of the referring ophthalmologists I work with are very busy and it is hard to get patients an appointment with them in a timely manner. By offering these services, my patients can have their eye problems resolved much sooner.” Another plus is that patients may feel more comfortable if they already know and trust the person performing the procedure (you).
There are ways to mitigate the cost, including opting for refurbished/used models or sharing the financial burden with another optometrist. However, Corri Collins, OD, who practices in Lexington, KY, cautions that it is important to look closely at the warranty options, especially when purchasing a used device.
Beyond cost, optometrists should also consider the patient populations they typically treat and which types of procedures they plan to perform. “Making sure you have the volume of patients to pay for this investment is important,” says Dr. Collins, while noting that ODs who plan to offer SLT, YAG capsulotomy and LPI would benefit from a combination laser. “The simple YAG laser will allow you to perform YAG and LPI, but not SLT.”
A combination laser may also be more cost-efficient depending on the needs of the individual practice. It could also be a good option if space is an issue. Dr. Lighthizer opted for a combination device for these reasons as well as its ability to perform multiple procedures. “Doctors should also remember that when you turn the laser off, it functions like a slit lamp as well,” he notes. “Therefore, when you aren’t using the laser, you can use the room for patient examinations.”
Making this investment can feel daunting, but it should be approached the same way as any other large equipment purchase, recommends Dr. Brog. “You need hands-on experience. Also, it is important to talk to colleagues about what they have and what they like. Equipment representatives can also add insight.”
Shop around, advises Dr. Lighthizer. “Every brand has its own bells and whistles,” he notes. “Explore the interfaces and get a feel for the individual lasers. Ultimately, it comes down to your preference and specific needs. I always say, your favorite laser will likely be the one you have in your office.”
Dr. Wroten recommends getting quotes from the major laser manufacturers to compare prices and features. “Demo their lasers in-office or at a national or regional conference or CE workshop seminar to get a feel for how they work with your arm length, the optics of the slit lamp, what the focusing beams look like, how it’s adjusted and so on.”
In addition to the laser, optometrists will also need the appropriate laser lenses. Some popular options on the market include the Latina SLT lens or Rapid SLT lens for SLT, the Abraham YAG iridotomy lens for LPI and the Abraham YAG capsulotomy lens for YAG capsulotomy. Like purchasing a laser, Dr. Brog based his choices—Abraham YAG laser capsulotomy lens, the Abraham YAG laser iridectomy lens and Volk’s rapid four-mirror SLT lens—on colleague recommendations and hands-on practice.
Some ODs may opt to perform capsulotomies without a lens; however, Dr. Collins finds that, while not always a necessity, the Abraham lens can make the procedure run much smoother with fewer complications. “In some scenarios, doctors will not use a lens during a YAG capsulotomy procedure, but there are certain cases where the lens is crucial,” she notes. “If the patient’s cornea has certain abnormalities, a lens with a cushioning solution will help to smooth out the appearance of the cornea and make the procedure much easier.
“The lens also helps with the clarity of the posterior capsule as well as minimizing the possibility of pitting the IOL,” Dr. Collins continues. “The Abraham iridectomy lens is also useful in an LPI because it can be used for pressure if there is an iris bleed.”
When considering SLT lenses, Dr. Brog initially bought a one-mirror Latina lens, and while he was able to perform the procedure, he reports that it took longer. “The lens has to be turned on the patient’s eye many times to treat 360°,” he explains. “I found that the patients were more and more uncomfortable as the procedure went on. The rapid four-mirror is much faster and improves patient comfort. The lens only has to be rotated once to treat 360° (Figure 6). You can find these lenses anywhere you buy your 20D, 90D or other lenses you already use in your office.”
|
Fig. 6. The Rapid SLT lens from Volk is what Dr. Brog uses (notice the four mirrors). Compared with a one-mirror lens, he has found that this one helps to expedite procedures and is more comfortable for patients since it does not have to be moved around to treat 360° of the eye. Photo: Nathan Lighthizer, OD. Click image to enlarge. |
While the laser and laser lenses are the key pieces needed for these procedures, there are a number of other items required. “Every office should have a blood pressure cuff to check BP before and after the procedure,” says Dr. Brog. “You should also have topical proparacaine for pre-procedure anesthesia as well as topical brimonidine for use pre- and post-procedures.” Check out the table below for other items that you should have on-hand in your clinical practice.
What You Need to Perform Laser Procedures (YAG, SLT, LPI)
|
When choosing between different brands, it ultimately comes down to personal preference. For example, there are a variety of cushioning solutions for use with laser lenses (e.g., Genteal Gel, Celluvisc, Goniosol, Goniovisc). Dr. Brog prefers the Genteal Gel since it stays on the lens well as you insert it into the eye, and it is not toxic to the cornea.
On the other hand, Dr. Wroten opts for Celluvisc because he finds it to be gentler on the cornea and has a good viscosity. As discussed above, optometrists must do their own legwork. Test out the different options and get feedback from colleagues who have experience with these items.
There are some tools that, while not necessary, can be helpful additions when performing these procedures. For instance, Dr. Brog recommends having a strap attached to the laser that goes around the patient’s head. He notes that while he has tried different ways to control patient movement during the procedure, including having a staff member or himself hold the patient’s head against the rest, a strap has proven most effective.
“Other doctors might prefer other methods and I have seen them used successfully,” says Dr. Brog. He adds, “Another thing is to have a good arm rest when performing laser procedures. It helps steady your hand.”
While this doesn’t necessarily fall under equipment, it is important not to overlook consent forms, urges Dr. Collins. “Make sure you have a good patient consent form that is easy to read and comprehend. It is crucial to have this documentation when performing these procedures.”
Conclusion
Fully equipping your practice to perform these surgical procedures takes time; however, with the right tools and support, optometrists are perfectly positioned to provide these important services to their patients.
Exactly what you need depends on what level you want to practice, notes Dr. Brog. “You can always start with a few basic procedures and move up from there,” he says. When selecting specific tools and equipment, he recommends finding a starting point with trusted information from colleagues.
“As you practice, fine-tune those things with personal preferences. The key is to get started,” Dr. Brog says. “It is the same as with your slit lamp, gonio lens, retinoscope or BIO. The more you use them, the more you will determine what works best for you,” he explains.
“The most important point in performing these procedures is to do what we always do with any procedure in optometry, and that is to follow the standard of care,” he concludes. “Always think about your patients and which tools will best fit their needs. If you do that, you will be successful. It will also make a big difference in the lives of your patients.”