
A 73-year-old Hispanic female presented complaining of blurred vision in her left eye and difficulty reading newsprint for the past three months. She underwent uncomplicated cataract surgery in her right eye approximately three years earlier. After the surgery, best-corrected visual acuity measured 20/20 O.D. and 20/25 O.S.
At this visit, her best-corrected visual acuity measured 20/25 in the right eye and 20/30 in the left. Motility testing was normal. Confrontation visual fields were full to careful finger counting in both eyes, and her pupils were equally round and reactive, with no afferent pupillary defect. Anterior segment exam was significant for a well-positioned posterior chamber intraocular lens (IOL) in the right eye and a 2+ nuclear sclerotic cataract in the left.
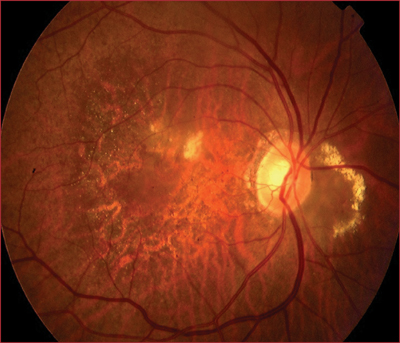
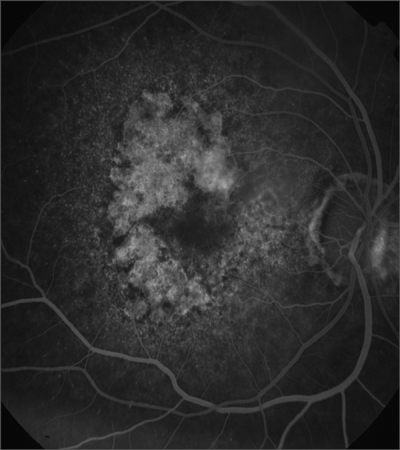
Dilated fundus exam revealed a moderate-sized cup with good rim coloration and perfusion O.U. There were localized areas of circinate exudate on the nasal side of both optic nerves (figures 1 and 2) and obvious macular changes in both eyes. A fluorescein angiogram was performed concentrating on the right eye (figures 3 and 4).
 |
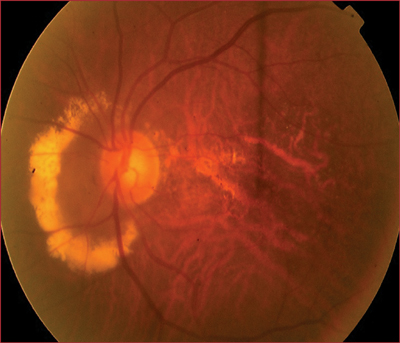 |
| 1, 2. Dilated fundus exam (O.D. left, O.S. right) showed localized areas of circinate exudate on the nasal side of each optic nerve. .Also, note the macular changes in each eye. | |
 |
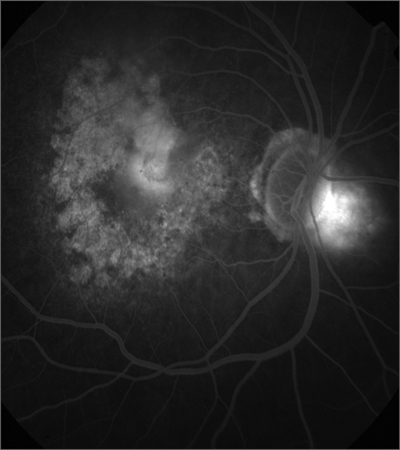 |
| 3, 4. An early (left) and late (right) frame from the fluorescein angiogram of the right eye shows some interesting staining and leaking patterns. What do these represent? | |
Take the Retina Quiz
1. What caused the changes around each optic nerve?
a. Optic nerve dystrophy.
b. Juxtapapillary choroidal neovascular membrane.
c. Polypoidal choroidal vasculopathy (PCV).
d. Chronic papilledema.
2. What does the fluorescein angiogram of the right eye reveal?
a. Geographic atrophy.
b. Choroidal neovascular membrane.
c. Disciform scar.
d. Both a and b.
3. What do the changes in each macula represent?
a. Geographic atrophy.
b. Exudative age-related macular degeneration.
c. Stargardts disease.
d. Both a and b.
4. What is the correct diagnosis?
a. PCV.
b. Exudative AMD.
c. Geographic atrophy.
d. All of the above.
5. What treatment is appropriate for the optic nerve changes?
a. Observation.
b. Laser photocoagulation.
c. Photodynamic therapy.
d. Lucentis (ranibizumab, Genentech).
6. What treatment is appropriate for the macular changes?
a. Observation.
b. Laser photocoagulation.
c. Photodynamic therapy.
d. Lucentis.
For answers to this months quiz, please see below.
Discussion
Our patient presented several years earlier with a visually significant cataract in her right eye. At that initial exam, we discovered the circinate exudate nasally around the left optic nerve but not around the right optic nerve. However, the same changes developed in the right eye two years later.
Fluorescein and indocyanine green angiography revealed that these changes represented polypoidal choroidal vasculopathy (PCV). Because these changes were located nasally, they did not represent a threat to her vision, so we chose to observe her. Since the discovery, the changes around her optic nerves have not progressed.
We were more concerned about the changes in each macula. Clinically, it was evident that she had widespread geographic atrophy of the retinal pigment epithelium (RPE) in both eyes. Of even greater concern: a small area of subretinal fluid located superiorly in her right macula.
Because of the problems in her right eye, she did not undergo cataract surgery in the left, nor would she have benefited from doing so. And, she subsequently developed loss of vision due to the geographic atrophy.
Fluorescein angiography confirmed the presence of a typical choroidal neovascular membrane. Given the close proximity to her fovea, we referred her to a retinal specialist, who treated her with Macugen (pegaptanib sodium, Eyetech/Pfizer). Had Lucentis been FDA approved at the time, that would have likely been the treatment of choice. (Lucentis received FDA approval on June 30.)
The patient subsequently required a second Macugen injection, which stabilized the choroidal neovascularization (CNV). On her most recent exam, visual acuity in the right eye measured 20/40, due to the geographic atrophy.
The left eye did not have as good of an outcome. The geographic atrophy progressed to involve the entire macula, leaving her with 20/200 acuity in that eye.
This case was interesting in that our patient had several disease processespolypoidal choroidal vasculopathy, geographic atrophy of the RPE and exudative AMDgoing on at the same time
Lawrence Yannuzzi, M.D., initially identified PCV in 1982.1 The hallmark of the disease is a vascular network of vessels in the inner choroid that develop peculiar aneurysmal bulges. They appear as reddish-orange, spheroidal, polyp-like structures. Clinicians initially thought these structures involved only the peripapillary choroidal circulation but now realize that they can occur around the macula as well.
Patients who have PCV often present with multiple, recurrent, serosanguineous detachments of the RPE and neurosensory retina. These occur secondary to leakage and bleeding from the aneurysmal choroidal vascular lesions. We were concerned that the area of fluid in the macula also represented an area of PCV, but ancillary studies showed this was not the case.
Our patient had typical CNV due to exudative AMD in her right eye and severe geographic atrophy of the RPE in both eyes. Although we could do nothing for the geographic atrophy, treatment of the CNV in the right eye preserved some level of vision.
Use of anti-VEGF drugs, namely Macugen and Lucentis, to treat CNV represents a paradigm shift from traditional treatments, such as thermal laser photocoagulation, which sometimes destroyed the CNV at the expense of normal retinal tissue. By inhibiting VEGF, which stands for vascular endothelial growth factor, these drugs target the root cause of CNV.
Macugen was the first FDA-approved drug for the treatment of CNV. Despite improved visual function compared with conventional treatment, patients continue to show a decline in visual function over time.2
Patients who receive Lucentis, however, show stabilization and even improvement in visual function.3 This may prove to be the most successful treatment for CNV thus far.
Although Lucentis was not yet available for our patient, she still achieved a very good outcome from Macugen, with complete resolution of her CNV. We continue to watch her very closely, and visual acuity in her right eye has remained 20/40.
We addressed her difficulty reading with a change in her Rx, including an increase in reading add.
Retina Quiz Answers: 1) c; 2) d; 3) d; 4) d; 5) a; 6) d.
1. Yannuzzi LA, Ciardella A, Spaide RF, et al. The expanding clinical spectrum of idiopathic polypoidal choroidal vasculopathy. Arch Ophthalmol 1997 Apr;115(4):478-85.
2. Gragoudas ES, Adamis AP, Cunningham ET Jr, et al. Pegaptanib for neovascular age-related macular degeneration. N Engl J Med 2004 Dec 30;351(27):2805-16.
3. Rosenfeld PJ, Heier JS, Hantsbarger G, Shams N. Tolerability and efficacy of multiple escalating doses of ranibizumab (Lucentis) for neovascular age-related macular degeneration. Ophthalmology 2006 Apr;113(4):632.e1.

