 |
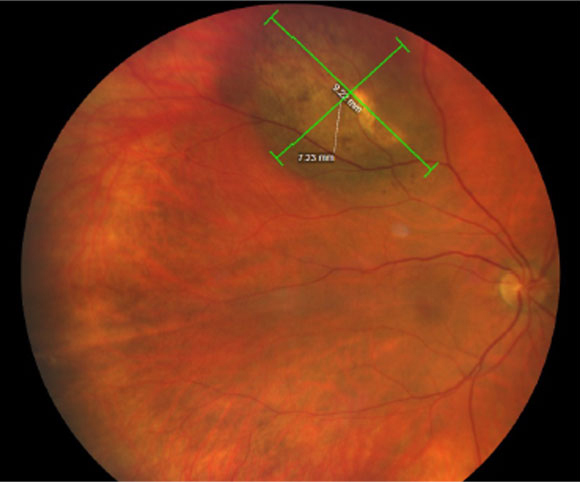
| Regular eye exams can also act as cancer screenings. Making this service available to the public regardless of income or insurance status would enable earlier ocular tumor detection and treatment. Photo: Amy Bade, OD. Click image to enlarge. |
The US Department of Health and Human Services defines social determinants of health as “the conditions in the environments where people are born, live, learn, work, play, worship and age that affect a wide range of health, functioning and quality-of-life outcomes and risks.” These determinants can be grouped into five categories: economic stability; education access and quality; healthcare access and quality; neighborhood and built environment; social and community context. Evaluating all these factors together can help determine patient health outcomes, which was the aim of a recent study that looked specifically at ocular cancer patients.
Its researchers obtained records of individuals in the National Cancer Database who were diagnosed with uveal melanoma (n=3,968), conjunctival melanoma (n=352) or retinoblastoma (n=480) between 2006 and 2017. SDH-related characteristics and clinical metrics (including tumor presentation, 30-day post-surgery readmission and overall survival) were then compared between the three cohorts.
The data revealed a host of differences between the cancer types, including race, income group, population density, history of prior malignancy, clinical tumor classification at presentation, surgical treatment, radiotherapy, chemotherapy, 30-day readmission and overall survival, to name a few.
No insurance (odds ratio=1.74) and Medicaid primary payer status (OR=1.88) showed an increased likelihood of advanced clinical tumor classification. Conversely, two characteristics associated with a decreased likelihood of advanced clinical tumor classification at presentation were female sex (OR=0.82) and top income quartile (OR=0.69).
Other pertinent findings from the study were that ocular cancer patients in rural areas were more likely to be readmitted within 30 days following initial treatment (OR=7.16), and increased age was associated with decreased five-year ocular survival (hazard ratio=1.04).
“Our findings suggest that SDH plays a critical role in predicting the probability of advanced clinical tumor classification in eye cancer patients,” the researchers wrote in their paper, published recently in the American Journal of Ophthalmology. “Specifically, patients with Medicaid and uninsured primary payer status relative to privately insured individuals were significantly more likely to present with advanced tumor presentation. Likewise, relative to individuals in the bottom income quartile, patients in all higher income quartiles exhibited significantly decreased probability of advanced tumor staging. These findings suggest that financial disparities, in particular, play a role in worsening the odds of early detection of eye cancers,” they concluded.
Due to the rarity of ocular cancers in comparison to other types, such as cervical cancer, it’s unlikely that legislation will be adopted to secure solutions to financial barriers, such as community screenings, the researchers suggested. However, public health efforts to promote equal access to regular eye care—which can also serve as cancer screening—may help to mitigate this issue of access.
This research highlights the need for eyecare providers to be confident in identifying and diagnosing ocular tumors early—at least for the individuals who are able to visit their clinic—to initiate sooner treatment and encourage better outcomes.
Choudhry HS, Patel AM, Nguyen HN, Kaleem MA, Handa JT. Significance of social determinants of health in tumor presentation, hospital readmission, and overall survival in ocular oncology. Am J Ophthalmol. November 11, 2023. [Epub ahead of print]. |

