 |
Q:
An eight-year-old girl presents as a weekend emergency after a fishing line with weights on the end sprung into her eye. What’s the appropriate management of this patient?
“First, obtain a good case history,” says Jessica Schiffbauer, OD, of The Eye Centers of Racine and Kenosha, WI. Ask the child and her family questions that include time of injury, time the vision loss occurred, any systemic medications with anticoagulants (aspirin, NSAIDs, warfarin or clopidogrel), personal or family history of sickle cell disease and history of any nose bleeds, bleeding gums or easy bruising.
Examine Closely
Check the patient’s vision and pinhole acuity. “For patients with recent injury or trauma, advise staff to avoid touching the eye until further instructed, which includes deferring fluorescein instillation and IOP measurement until the doctor sees the patient,” Dr. Schiffbauer says.
To rule out a ruptured globe or penetrating ocular injury, perform a slit lamp examination prior to the insertion of drops. This is often difficult due to pain and photophobia. “Anesthetic will probably be required, so I put in a drop or two of proparacaine to perform the slit lamp exam and then use a fluorescein strip to check Seidel,” Dr. Schiffbauer notes.
 |
|
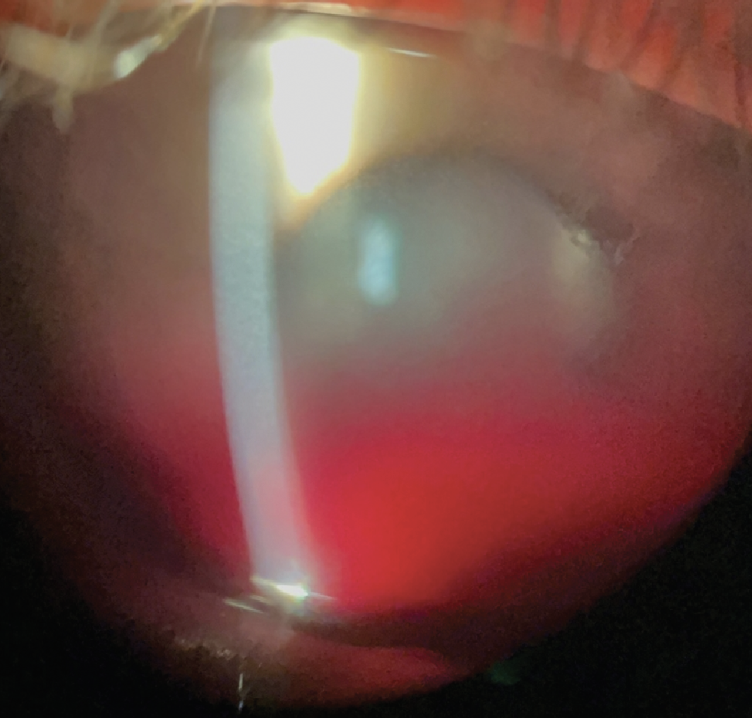
Fig. 1. Slit lamp image of hyphema. Click image to enlarge. |
Once a laceration or penetrating injury has been ruled out, assess the anterior chamber for circulating red blood cells and/or inflammatory cell and flare, each graded separately. Dr. Schiffbauer measures the height of the hyphema and notes the location of any clot or blood. If possible, she will try to document the hyphema with a slit lamp photo, as she did here on initial presentation (Figure 1). Capturing these pictures is great so you will have them on file as you follow these patients through the healing process.
Now it’s time to check the IOP, and using iCare for a child this age is probably a good choice. Dilated fundus exam is mandatory. “Unfortunately, in this case, the view of the posterior segment was limited due to the hyphema,” Dr. Schiffbauer observes. “If ultrasound is available, I would perform a B-scan with light pressure to assess the status of the retina.”
The Five-Day Period
The greatest risk for new bleeding or rebleeding occurs within the first five days. Advise the patient—and their parents—to keep their head continuously elevated, sleep with the head propped up at a 45º angle, avoid physical activity, bending or lifting, and also wear an eye shield while sleeping. It may be best for the child to stay home from school to avoid further injury to the eye and reduce the risk of a rebleed.
Start the patient on a topical cycloplegic such as Cyclogyl (cyclopentolate 1%, Alcon) or atropine TID OD and a topical steroid such as prednisolone every two hours.
“If the IOP is in the upper twenties or higher, start a combination ocular hypotensive medication such as brimonidine-timolol, dorzolamide-timolol or brinzolamide-brimonidine BID,” Dr. Schiffbauer advises. “Avoid prostaglandins and miotics to avoid more inflammation and confirm that the child has no asthma or breathing issues prior to starting a beta-blocker.”
Depending on the response from topical treatment, oral treatment for IOP may be indicated. If this patient does have sickle cell disease or trait, avoid carbonic anhydrase inhibitors, alpha agonists and prostaglandins. Monitor this patient daily to check visual acuity, IOP and slit lamp for improvement.
 |
|
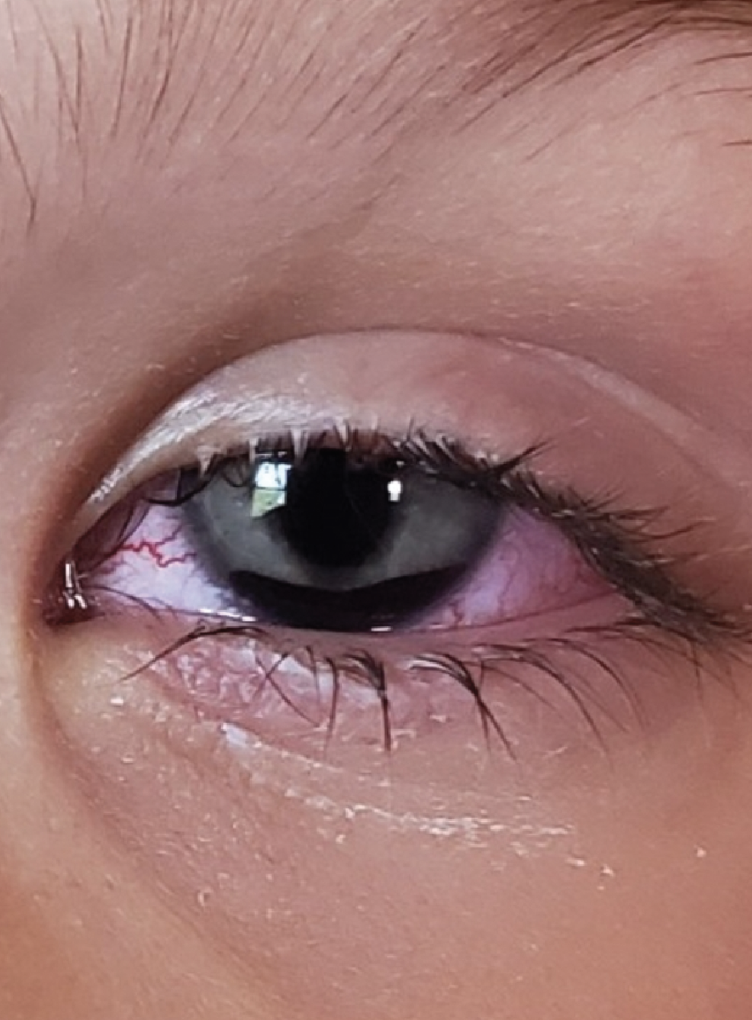
Fig. 2. Significant improvement at 28-hour follow-up. Click table to enlarge. |
At the 28-hour follow-up, our patient’s condition improved significantly (Figure 2). The blood had settled, and the vision was clearing dramatically. This was encouraging, but Dr. Schiffbauer would still be worried about the risk of a rebleed, given the patient’s age.
“Continue with the drops and slowly taper off the cycloplegic and anti-inflammatory as the blood, fibrin and white blood cells start to resolve,” she suggests. “At this visit, I would also attempt to evaluate the posterior segment.”
Once the patient has made it past the critical period, Dr. Schiffbauer would perform gonioscopy to check for signs of peripheral anterior synechiae or angle recession.
“If continual improvement is noted, start spacing out the visits and tapering off the drops,” she says. “Due to the patient’s age, I would recommend keeping all the restrictions in place until the hyphema has resolved.”
Educate this child’s parents about the risk of complications following a traumatic injury, such as cataracts, elevated IOP and glaucoma. If no complications arise, examine this patient annually with gonioscopy. Also, stress the need for eyewear protection for future fishing trips.
“This case and ones like it are easily managed by the doctor of optometry. Consider a second opinion if there is corneal blood staining, no significant improvement (<50%) of the hyphema after one week, or extremely elevated pressure that does not respond to topical therapy,” Dr. Schiffbauer recommends.
Dr. Ajamian is board certified by the American Board of Optometry and serves as Center Director of Omni Eye Services of Atlanta. He is vice president of the Georgia State Board of Optometry and general CE chairman of SECO International. He has no financial interests to disclose.

