 |
Q:
I have a 12-year-old patient who presented with a “growth” on the conjunctiva. What is it, and what can I do about it?
A:
Pyogenic granuloma (PG) is a benign, acquired, vascular lesion that is part of an aberrant wound healing process. After an insult to tissue, such as trauma or inflammation, an exaggerated fibrovascular response occurs. Histologically, PG is composed of chronic inflammatory cells and capillaries. “The term pyogenic granuloma is a misnomer, as the lesion is neither pyogenic (pus-producing) nor a true granuloma,” says Stephanie Jian, OD, of the Vanderbilt Eye Institute in Nashville.
Clinically, PG appears as a fleshy, elevated, red-pink mass. Its shape is variable: round, ovoid or lobular. The shape is categorized as either pedunculated (attached via a stalk/peduncle) or sessile (flat and without a stalk/peduncle). PG can grow on cutaneous or mucosal surfaces. “They often grow rapidly, which can help differentiate pyogenic granuloma from more malignant lesions,” Dr. Jian notes.
Ocular PGs are most commonly seen on the palpebral and bulbar conjunctiva. They can also grow on the external eyelid surface. Rare cases of corneal PG have been reported in the literature.
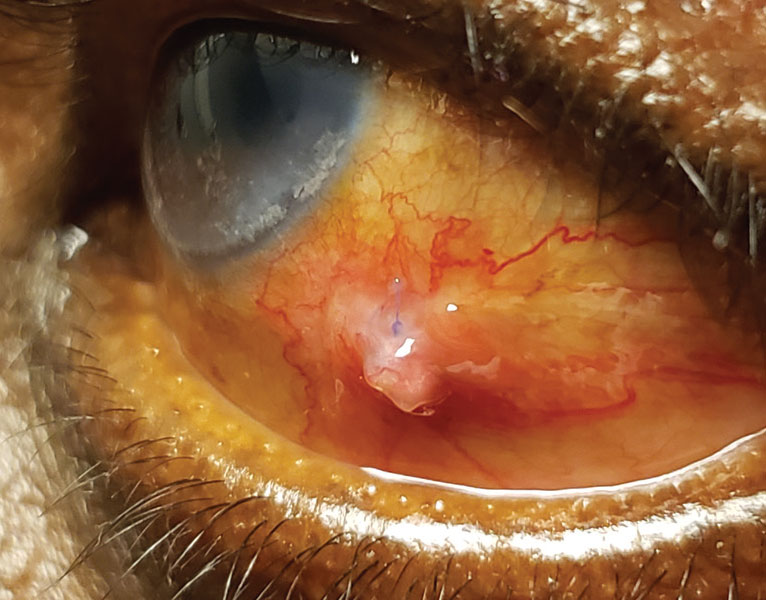 |
| PG can be treated by the primary care OD without a referral. Click image to enlarge. |
PG and Children
Pyogenic granuloma are common in children. There is a definite relationship between chalazion and the development of pyogenic granuloma, with a chalazion preceding 42% of PG cases.1 There is also a strong relationship between ocular surgery and the development of PG, as 40% are preceded by ocular or adnexal surgery.1 Dr. Jian states that PG is not uncommon after strabismus surgery. Approximately 2% of patients who have strabismus surgery develop PG.2 “They typically develop a few weeks after eye muscle surgery near the area of sutured conjunctiva,” she observes.
According to Dr. Jian, topical steroids and/or surgical excision are the traditional treatment option for PG. Smaller PG are more likely to respond to topical treatment. One study found a 90% success rate when treating pyogenic granuloma with topical steroids.2
Topical timolol has been recently used to successfully treat ocular PG. Timolol solution or gel was dosed twice a day in adult and pediatric patients with ocular PG, with high resolution rates ranging from 88% to 100%.3,4,5 In these studies, timolol was dosed twice a day for two to six weeks. “Many cases in the dermatological literature have demonstrated successful treatment of cutaneous PG using topical timolol, often in children,” Dr. Jian says.
Beta-blockers have been used, topically and systemically, to treat capillary hemangiomas. It is hypothesized that beta blockers cause vasoconstriction within the hemangioma, subsequently inhibiting VEGF and promoting apoptosis. Beta blockers’ mechanism of action in treating PG, another vascular lesion, is likely similar.
“There are many advantages to considering timolol treatment for PG, especially in pediatric patients,” Dr. Jian says. Timolol has a lower side effect profile than topical steroids. Both topical steroid eye drops and timolol are noninvasive and avoid local/general anesthesia.” Timolol is also less expensive than topical steroids. Lastly, timolol is instilled less frequently than a topical steroid.
“Bottom line, PG are common in children as well as adults and can be treated by the primary care optometrist effectively and without a referral,” she says.
Dr. Ajamian is the center director of Omni Eye Services of Atlanta. He currently serves as general chairman of the education committee for SECO International. He has no financial interests to disclose.
1. Ferry, AP. Pyogenic granulomas of the eye and ocular adnexa: a study of 100 cases. Trans Am Ophthalmol Soc. 1989;87:327-47. 2. Espinoza GM, Lueder GT. Conjunctival pyogenic granulomas after strabismus surgery. Ophthalmology. 2005;112(7):1283-6. 3. Oke I, Alkharashi R, et al. Treatment of ocular pyogenic granuloma with topical timolol. JAMA Ophthalmol. 2017;135(4):383-5. 4. Demaria LN, Silverman NK, Shinder R. Ophthalmic pyogenic granulomas treated with topical timolol–clinical features of 17 cases. Ophthalmic Plast Reconstr Surg. 2018;34(6):579-82. 5. Nair AG, George RJ, Natarajan S, Jain V. Topical timolol for the treatment of conjunctival pyogenic granulomas: outcomes and effect on intraocular pressure. Indian J Ophthlamol. 2020;17(1):2170-4. |

