 |
A 74-year-old man presented to the office with a chief complaint of blurry vision in both eyes of four months’ duration. He said the issue had gradually become worse. He also commented that he “had to look at people to make his vision right over the last three months.” He did not report any pain and denied trauma. He was properly medicated for hypertension and diabetes and denied allergies of any kind.
Clinical Findings
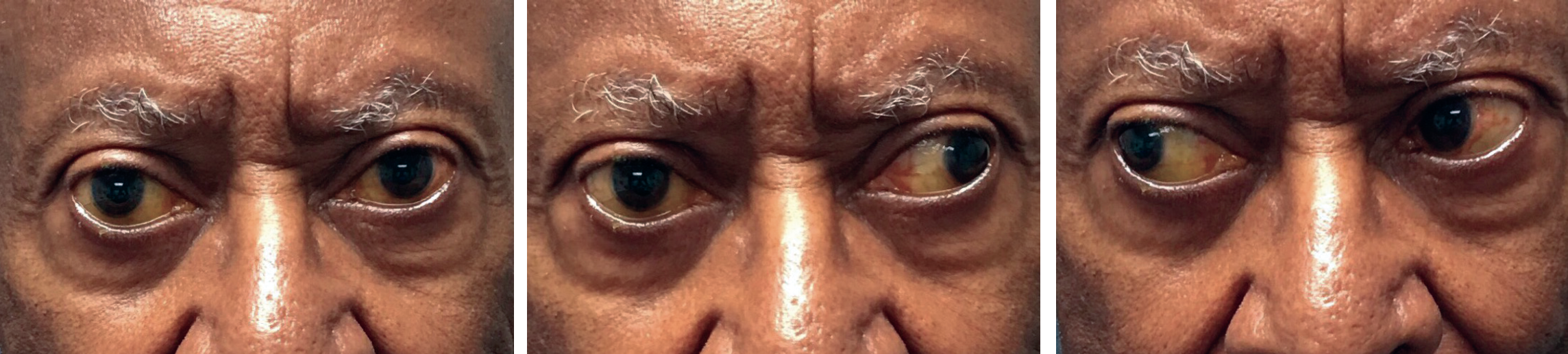
His best-corrected entering visual acuities were 20/30 OD and 20/30 OS. His external examination was remarkable for the extraocular muscle motility findings demonstrated in the photographs below. (He initially reported no double vision).
 |
|
Gaze assessment yielded the findings seen above. What could be causing this presentation? Would you rate the level of care needed to address his status as routine, urgent or emergent? Click image to enlarge. |
There was no evidence of afferent pupillary defect and his confrontation visual fields were full. His anterior segment findings were normal. Goldmann applanation tonometry measured 17mm Hg OU. Dilated fundus examination found no posterior pole or peripheral pathologies, with cup-to-disc ratios measuring 0.3/0.3 round and sharp and pink discs noted.
For Additional Information
Additional studies used to further investigate this case included measuring the deviation in five positions of gaze (primary, up, down, left, right). Gaze left was scrutinized for an abduction nystagmus, which was found.
After further discussion, “horizontal diplopia” was present on gaze left. Health history questions were also asked in an attempt to identify other neurological signs or symptoms (e.g., dizziness, loss of balance, disequilibrium, difficulty speaking, limb drift, face droop, headache, tinnitus, numbness, tingling).
What would be your diagnosis in this case? What is the patient’s likely prognosis?
Connecting the Eye and the Brain
The diagnosis in this issue is right internuclear ophthalmoplegia (INO). This condition is created when a brainstem lesion involves the medial longitudinal fasciculus (MLF). The injury produces a conjugate horizontal gaze (horizontal “yoked” eye movement) defect that classically manifests as an impaired ipsilateral adduction deficit (the right eye cannot turn in; INO is named for side in which the MLF pathway is damaged—a right MLF lesion produces a right adduction deficit) along with an abducting nystagmus seen when the unaffected contralateral eye looks left.1-14
Horizontal conjugate gaze movements can be voluntary (“I wish to look left or right”) or involuntary (“I am falling to the left and my eyes, in a reflex-like movement, dart left”).
In a voluntary lateral gaze scenario, the signal for “looking left” starts in the right pre- and primary motor cortex (Brodmann areas 4 & 6) and travels down the ipsilateral corticobulbar spinal tract.7 The impulse travels along the internal capsule and the cerebral peduncle, then decussates to the opposite side at the level of the midbrain to innervate the left paramedian pontine reticular formation (PPRF).7 This structure also receives afferent impulses from the frontal eye field and from the parietal eye field.7 This plays a role in involuntary lateral conjugate gaze. The PPRF contains excitatory “burst” neurons that produce a pulse that is transmitted to the abducens nucleus on the same side.7 Involuntary conjugate eye movements also use other mechanisms to generate signals that are delivered to the corresponding PPRF.
Once the PPRF discharges a signal into the left CN VI nucleus, it is relayed into right MLF. The left and right tracts of the MLF move superiorly through the spinal cord, connecting each CN VI nucleus to the contralateral CN III (oculomotor) nucleus. This design permits the right eye to adduct (tracks in) when the left eye abducts (moves out).1-7 The result is a simultaneous and coordinated contracture of the left lateral rectus (an abduction movement) and contracture of the right medial rectus (an adduction movement), producing conjugate gaze left.1-7
The MLF facilitates actions that coordinate the oculomotor and the abducens nuclei, generating conjugate horizontal eye movements.1-7 It is the final common pathway for different types of conjugate eye movements that include saccades, smooth pursuits and the vestibulocochlear reflex.14
Differential Diagnosis
When any neurologic disease or lesion is discovered, one should consider four areas of origin: (1) the muscle, (2) the nerve, (3) the neuromuscular junction and (4) the brain. The disorders of horizontal eye movement that are caused by brainstem lesions include lateral gaze palsy, internuclear ophthalmoplegia and one-and-a-half syndrome.7
Lateral gaze palsy is caused by a lesion involving the paramedian pontine reticular formation (PPRF) or the abducens nucleus.7 In this pathology, the signal to move the eye is blocked from stimulating the lateral rectus on the same side or the MLF on the opposite side. When a person wants to gaze in a particular direction, the lateral rectus fails to abduct on that side and the medial rectus fails to adduct on the opposite side.7 The result is that the individual cannot look in that direction.7
INO occurs as a result of a lesion involving the MLF after successfully reaching the abducens nucleus.1-7 The ipsilateral lateral rectus receives a signal and the eye abducts (moves out) but the crossing or contralateral MLF is blocked so the fellow eye never receives a signal in the CN III nucleus to activate the medial rectus and adduct (move in).7 The abducting nystagmus seen in the eye that is moving out is secondary to compensatory signaling brought about by the inability to complete the adduction movement in the fellow eye; this is parcel to Herring’s law of equal innervation.14
One-and-a-half syndrome is a combination of lateral gaze palsy and internuclear ophthalmoplegia; it is caused by a lesion involving both the ipsilateral PPRF or the ipsilateral CN VI nucleus and the ipsilateral MLF.7 The lesion in the brain is so large that it clips the PPRF and CN VI nucleus while extending far enough to hit the crossing MLF coming from the other CN VI nucleus. The result is an eye that cannot look left or right while the other eye can only abduct.7
The most common causes of INO are multiple sclerosis (demyelinating disease) and brainstem infarction.3,4 Other causes include head trauma (tentorial herniation), brainstem and fourth ventricular tumors (medulloblastoma, glioma, lymphoma, metastases), the Arnold-Chiari malformation, infection (e.g., zoster, syphilis), hydrocephalus, lupus erythematosus and Sjögren’s syndrome.1-14 The incidence of internuclear ophthalmoplegia in males and females is virtually equal.14 The condition is extremely rare in the pediatric population.14
INO does not affect convergence.8 This is called dissociation of convergence. This is an important sign that helps distinguish internuclear ophthalmoplegia from pseudo-INO seen in cases of myasthenia gravis, third nerve palsy and Guillain-Barre syndrome (the presence of constant or variable ptosis is also diagnostic as this is not a sign of INO).14 Recent studies have recognized that retained convergence reflects the innate ability to converge to near targets.14
Bilateral INO is possible. Here, there is paresis of adduction in both eyes, bilateral abduction nystagmus and, when the eyes are in up gaze, there is impaired gaze-holding, impaired vestibular responses and impaired smooth tracking.8 When vertical diplopia is observed in the primary position, it is due to skew deviation where the weak adducting eye exhibits hypertropia.14 Skew deviation is a vertical misalignment of eyes caused by asymmetrical disruption of supranuclear input from the otolithic organs of the inner ear; it is an associated sign of INO.14
Demyelination secondary to multiple sclerosis (MS) can produce lesions to the MLF.3-5,9,10 In these cases, the condition can be aggravated by increasing the body’s temperature through exposure to a warm environment or exercise.5,10 This is known as Uhthoff's phenomenon, where functioning axons have their behavior altered, producing differing conduction velocities.3,4,10 Rapid (saccadic) horizontal eye movements will become impaired and patients report transient diplopia, visual confusion, the illusion of environmental movements during a saccade (Pulfrich phenomenon), vertigo and transient blur especially noted while reading.3 The saccadic eye movement abnormalities can be easily quantified by infrared oculography (eye tracking).5 The prevalence of clinically evident INO in cases of MS ranges from 24% to 55%. In most of these cases, the condition presents bilaterally.3
Prognosis
There is no treatment for INO; it may variably improve or not as the issue that produced it resolves or fails to resolve.1-14 One literature citation documents that nearly half of all cases of internuclear ophthalmoplegia resolve within one year.14 The key is prompt diagnosis so that discovery and treatment of the underlying cause may begin so as to prevent further signs or symptoms.1-14
In cases such as Sjögren’s syndrome, where there is cellular central nervous system infiltration, or cases that are the result of infection or compression, improvement may be seen after therapy removes the offending issue. Ischemic or hemorrhagic damage may never resolve, resulting in a chronic condition. In cases of demyelinating disease, exacerbations and remissions are common. Medications are being evaluated for their ability to stimulate re-myelination in both cases of optic neuritis and INO.5 Fampridine (dalfampridine) has had a positive effect on saccadic eye movements in patients with MS who suffer from an INO.5
This patient was referred to the emergency department for immediate neuroimaging to uncover the cause of their INO and to determine if hospital admission was required for a new medical condition requiring intervention.
Dr. Gurwood thanks Nick Karbach, OD, for his contributions to this case.
Dr. Gurwood is a professor of clinical sciences at The Eye Institute of the Pennsylvania College of Optometry at Salus University. He is a co-chief of Primary Care Suite 3. He is attending medical staff in the department of ophthalmology at Albert Einstein Medical Center, Philadelphia. He has no financial interests to disclose.
1. Virgo JD, Plant GT. Internuclear ophthalmoplegia. Pract Neurol. 2017;17(2):149-153. 2. Nij Bijvank JA, van Rijn LJ, Balk LJ, et al. Diagnosing and quantifying a common deficit in multiple sclerosis: Internuclear ophthalmoplegia. Neurology. 201914;92(20):e2299-e2308. 3. Obuchowska I, Mariak Z. Internuclear ophthalmoplegia--causes, symptoms and management. Klin Oczna. 2009;111(4-6):165-7. 4. Keane JR. Internuclear ophthalmoplegia: unusual causes in 114 of 410 patients. Arch Neurol. 2005;62(5):714-7. 5. Kanhai KMS, Nij Bijvank JA, Wagenaar YL, et al. Treatment of internuclear ophthalmoparesis in multiple sclerosis with fampridine: A randomized double-blind, placebo-controlled cross-over trial. CNS Neurosci Ther. 2019;25(6):697-703. 6. Kochar PS, Kumar Y, Sharma P, et al. Isolated medial longitudinal fasciculus syndrome: Review of imaging, anatomy, pathophysiology and differential diagnosis. Neuroradiol J. 2018;31(1):95-99. 7. Bae YJ, Kim JH, Choi BS, et al. Brainstem pathways for horizontal eye movement: pathologic correlation with MR imaging. Radiographics. 2013;33(1):47-59. 8. Zee DS. Internuclear ophthalmoplegia: pathophysiology and diagnosis. Baillieres Clin Neurol. 1992;1(2):455-70. 9. Serra A, Chisari CG, Matta M. Eye movement abnormalities in multiple sclerosis: pathogenesis, modeling, and treatment. Front Neurol. 2018 5(9):9:31. 10. Frohman TC, Davis SL, Frohman EM. Modeling the mechanisms of Uhthoff's phenomenon in MS patients with internuclearophthalmoparesis. Ann N Y Acad Sci. 2011;1233:313-9. 11. Niestroy A, Rucker JC, Leigh RJ. Neuro-ophthalmologic aspects of multiple sclerosis: Using eye movements as a clinical and experimental tool. Clin Ophthalmol. 2007;1(3):267-72. 12. Natsis KS, Boura E, Kyriazis O, et al. Bilateral internuclear ophthalmoplegia as a presenting manifestation of primary Sjögren’s syndrome. Neuroophthalmology. 2016;40(5):247-250. 13. Liu DT, Li CL, Lee VY. Internuclear ophthalmoplegia. Arch Neurol. 2006;63(4):626;626-7. 14. Feroze KB, Wang J. Internuclear Ophthalmoplegia. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019. |

