Spotlighting OSDMedication, infection, genetics, poor hygiene—these are only a few factors that contribute to ocular surface disease. This month in Review of Optometry, experts weigh in on the risk factors, diagnosis, treatment and management of numerous types of OSD. Check out the other articles featured in the November issue:
|
With a rising incidence of over 20 million affected people in the United States alone, dry eye disease (DED) is now considered a major ocular condition.1 DED affects patients of all ages and has been shown to negatively impact a patient’s quality of life both physically and psychologically.2 Increased awareness has led to significant worldwide progress in research, but dry eye management can be frustrating for both patients and clinicians alike. Significant strides have been made in not only defining and classifying DED, but also understanding the association between the condition, systemic comorbidities and systemic medications. The focus of this article will be iatrogenic DED; specifically, dry eye induced by systemic medications.
The definition of DED was carefully rewritten during publication of the 2017 report by the Tear Film & Ocular Surface Society’s Dry Eye Workshop II (DEWS II). The ultimate result: “Dry eye is a multifactorial disease of the ocular surface characterized by a loss of homeostasis of the tear film, and accompanied by ocular symptoms, in which tear film instability and hyperosmolarity, ocular surface inflammation and damage, and neurosensory abnormalities play etiological roles.”3 This loss of homeostasis is the common denominator of all dry eye subtypes.1
According to the latest Physician’s Desk Reference, 22 out of the top 100 best-selling systemic drugs in the US were shown to possibly cause dry eye.4 Additionally, eight out of the nine systemic drugs that are secreted into the tear film are associated with induced dry eye, including common over-the-counter (OTC) meds aspirin and ibuprofen.4 Systemic medications may cause DED through decreased tear production, inflammatory effects on secretory glands, altered nerve input and reflex secretion or direct irritation through secretion into the tears.5
Numerous classes of pharmaceuticals can trigger DED, so the list of medications associated with dry eye is quite extensive. A thorough patient history and medication review is crucial because myriad drugs, ranging from OTC medications to complex oncology and neurological agents, may affect the ocular surface. The DEWS II Iatrogenic Report provides a table of 171 systemic medications that are known or suspected to cause, contribute to or aggravate dry eye.5 However, bear in mind that much of the research is inconclusive and only 48 of the 171 medications are actually proven to be causative of DED.5
This article will review and give common examples of many of the medications from this list by class, discuss the mechanism of causation and offer approaches to management and treatment.
Anticholinergics
This is the largest category of systemic medications associated with dry eye, and the anticholinergics discussed in this article include antihistamines/decongestants, antidepressants, anti-Parkinson’s, antipsychotics and antispasmodic medications.5
Most anticholinergic medications are antimuscarinic, as they competitively inhibit the binding of acetylcholine at post-synaptic muscarinic receptors.6 In terms of DED, this action decreases both aqueous and mucus tear secretions from lacrimal gland and conjunctival goblet cell receptors. With decreased tear volume and quality, the stability of the tear film is lost.5,6
• Antihistamines and Decongestants. Commonly used and self-prescribed in many cases, antihistamines decrease tear production through reduction of aqueous outflow. From a DED perspective, it is better to prescribe or recommend second-generation antihistamines (e.g., Clarin, Zyrtec, Allegra) rather than first generation. Second-gen antihistamines have less anticholinergic side effects because they more selectively bind to muscarinic receptors.6 Commonly prescribed H1-antihistamines for allergies include diphenhydramine (first generation), loratadine (second generation) and cetirizine (second generation).7
Those H1-antihistamine agents may be found in combination with decongestant medications. Decongestants cause local vasoconstriction, which alters the blood flow to the lacrimal system, ultimately leading to reduced tear production.6,8 Pseudoephedrine (e.g., Sudafed) is the most commonly used decongestant.7
H2-antihistamines are prescribed for stomach, esophageal and intestinal issues. Since these drugs also affect the muscarinic receptors, DED can be induced. Common examples are cimetidine (Tagamet) and famotidine (Pepcid AC).6
• Antidepressants.Tricyclic antidepressants (TCAs), selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) all have been found to cause DED; they affect amine neurotransmitters. TCAs are well known to have anticholinergic effects, whereas SSRIs and SNRIs do not typically act as antimuscarinic agents despite showing increases in DED.
Both TCAs and SNRIs block serotonin and norepinephrine reuptake at the pre-synaptic neuron, ultimately leading to an increase in synaptic neurotransmission of serotonin and norepinephrine. SSRIs exclusively block serotonin reabsorption, increasing the level of serotonin concentrations binding to the post-synaptic receptors.5,6,9
No clinical studies to date have specified which antidepressant would be best prescribed for patients suffering from DED; however, based on conclusions drawn from studies on antidepressants and dry mouth, it is suggested that SSRIs affect tear film homeostasis less than TCAs.6,10 Better still are SNRIs, which have less dry eye associations than their SSRI counterparts.10
The most popular TCA prescribed is amitriptyline. Common SSRIs are sertraline (Zoloft), fluoxetine (Prozac), citalopram (Celexa) and escitalopram (Lexapro). Frequently prescribed SNRI antidepressants are duloxetine (Cymbalta) and venlafaxine (Effexor).7
 |
|
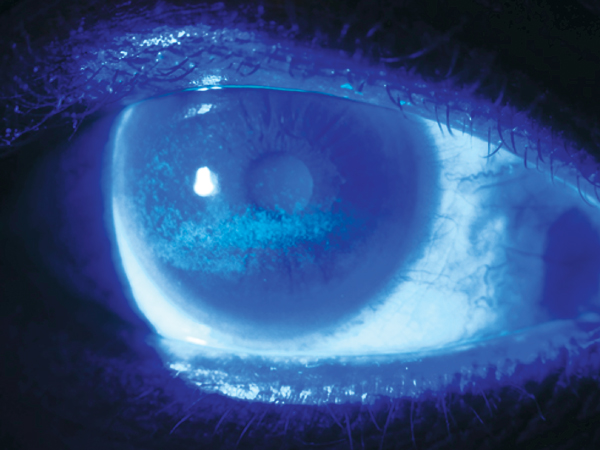
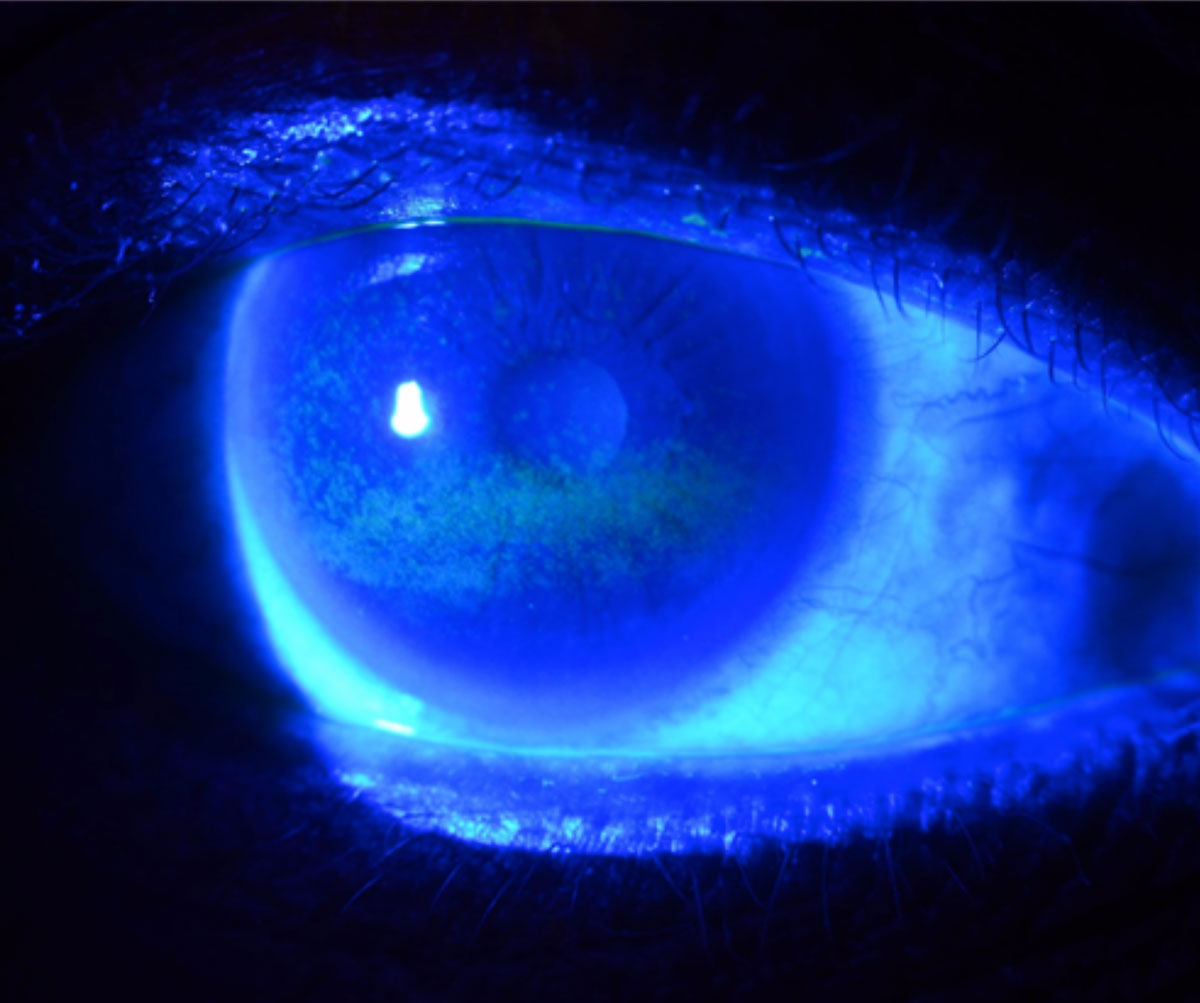
A photo demonstrating a classic presentation of dry eye with superficial punctate keratitis, greatest inferiorly. Photo: Brian Dornbos, OD. Click image to enlarge. |
• Anti-Parkinson’s drugs. Initially, the movement disorder Parkinson’s disease was treated with anticholinergics like benztropine and benzhexol. These drugs are now often used in conjunction with the favored anti-Parkinson medication levodopa, which may cause similar side effects to anticholinergic agents.6 Both in monotherapy and combination therapy, anti-Parkinson’s medications act comparably to their antidepressant and antipsychotic counterparts regarding their impact on DED.11
• Antipsychotics. These powerful drugs are classically divided into two groups: typical, which primarily affects dopamine receptors, and atypical, which primarily affects serotoninergic receptors. Meds in both groups have anticholinergic effects, but there are no studies to determine which specific drugs are better or worse for DED. Investigative studies regarding antipsychotics and dry mouth did not favor the typical or atypical group as a whole, but rather suggested that there are certain drugs in each category that seemed to have less anticholinergic peripheral side effects.
Of note, anticholinergic levels that affect the central nervous system do not correlate with anticholinergic levels in the serum.6 Current commonly used antipsychotic medications are haloperidol (typical), perphenazine (typical), quetiapine fumarate (atypical) and aripiprazole (atypical).5,7
• Antispasmodics. These drugs are used to treat overactive bladder by acting on muscarinic receptors. Inadvertently, their antimuscarinic properties lead to DED. Antispasmodics shown to cause DED symptoms are oxybutynin, tolterodine and fesoterodine.5,6
Antihypertensives
Of the four major classes of antihypertensive drugs, beta blockers and diuretics are known to induce dry eye. Beta blockers, which are adrenergic blocking, reduce aqueous production by lowering immunoglobulin A and lysozyme levels.11,12 Thiazide diuretics increase elimination of water and electrolytes, while loop diuretics reabsorb sodium. Both act on the kidney and reduce fluid availability throughout the body.8 With less overall fluid available to form tears, tear production is decreased.8,12
Popularly prescribed systemic beta blockers include metoprolol, atenolol, carvedilol and propranolol. Common diuretics include hydrochlorothiazide and furosemide.7
 |
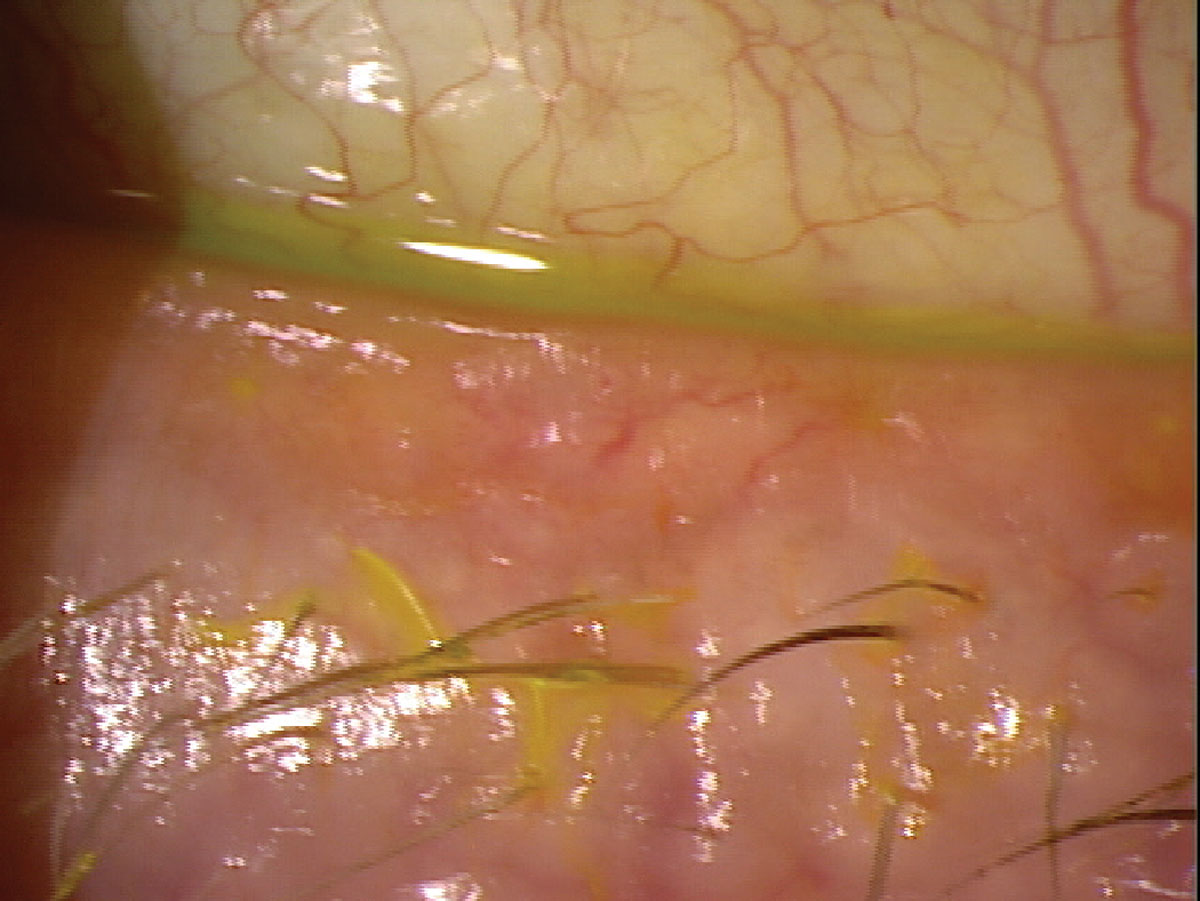
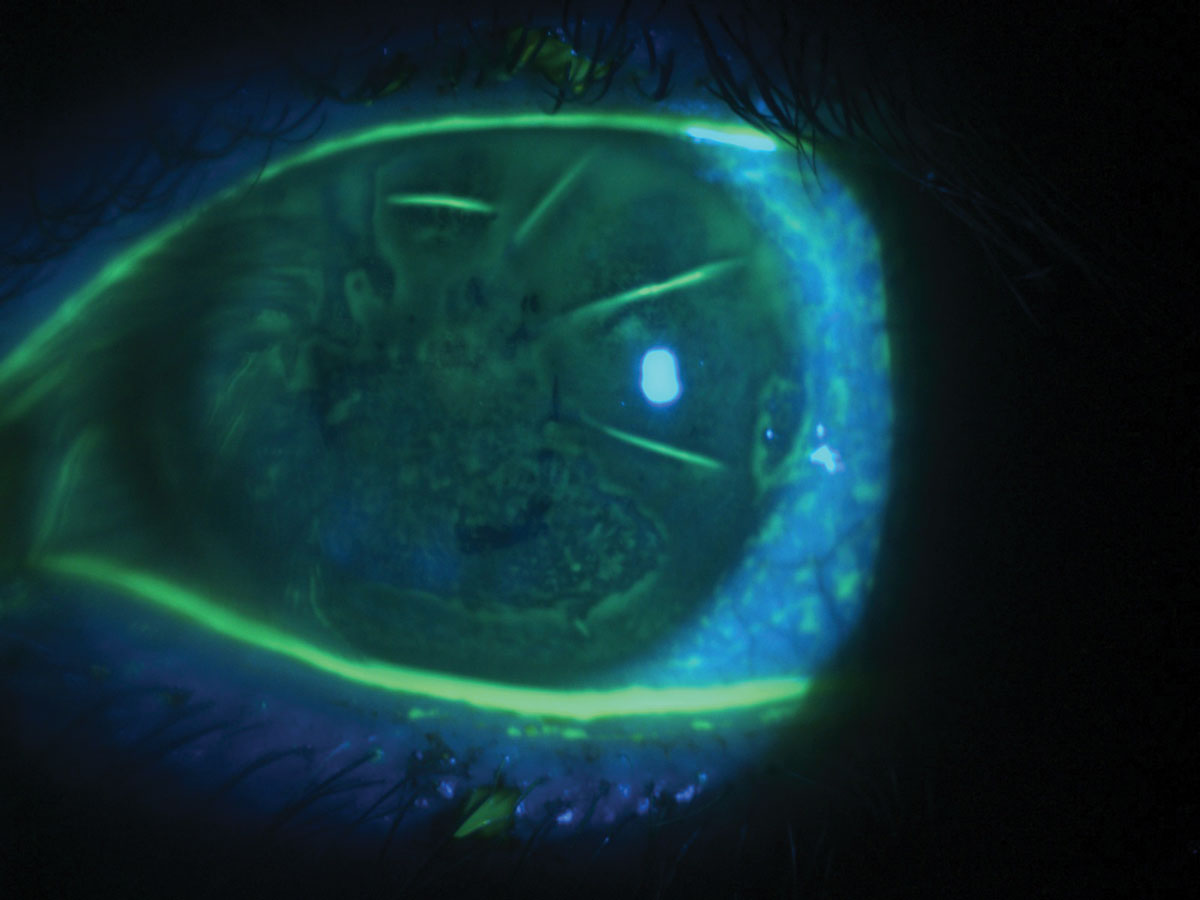
| Dry eye in a patient with melanoma taking chemotherapeutic medications. Photo: Juan Ding, OD. Click image to enlarge. |
A survey of eyecare providers at a national meeting found that only 10% of the 340 attendees reported use of this point-of-care test. This highlights the current lack of a widely accepted, inexpensive, in-office test that can accurately determine the presence of Ad-Cs.37
Hormonal Therapies
Investigative research regarding the role sex hormones play in DED is inconclusive, as some studies show benefits with hormone replacement therapy and others find worsening of dry eye signs and symptoms with these drugs. Combination estrogen and progesterone therapy during menopause can cause level imbalances that affect lacrimal function, but the effect of this combination therapy on DED is likely indirect.
Estrogen and progesterone are androgen-blocking agents, leading to decreased androgen levels and increased inflammation of the ocular surface. Oral contraceptives, which typically contain both estrogen and progesterone, have been specifically linked to meibomian gland dysfunction (MGD) associated dry eye.13 Two other popular hormonal medications that are associated with DED include tamsulosin and terazosin.5
 |
|
A polypharmacy patient with dryness associated with meibomian gland dysfunction. Photo: Brian Dornbos, OD. Click image to enlarge. |
Anticancer Drugs
Chemotherapeutic agents cannot differentiate between cancer cells and healthy cells. Consequently, the lacrimal glands are often affected, leading to the development of dry eye.8 Many anticancer medications also decrease stability of the ocular surface by disrupting the homeostasis of the cornea, conjunctiva and lacrimal system.14 Examples of these chemotherapeutic agents are methotrexate, mitomycin C, busulfan and cetuximab.5
Antiulcer Drugs
Recently, proton pump inhibitors (PPIs) have been linked to DED. The exact mechanism is unknown, but it is believed that long-term use of PPIs affects the absorption of vitamin B12, increasing risk of B12 deficiency and associated dry eye. Furthermore, PPIs affect the gut microbiome, which also maintains mucosal immune function outside the gut, and may ultimately impact the conjunctival microbiome.15
Omeprazole (Prilosec), one of the top 10 prescribed drugs in the US—available both OTC and with a prescription—is part of this medication class. Pantoprazole (Protonix) and esomeprazole (Nexium) are also commonly used PPIs.7
Anti-Acne Drugs
Most retinoids, a class of compounds derived from vitamin A, are topical. Isotretinoin, however, is a well-known oral retinoid used to treat acne; unfortunately, it is also causative for DED. Its mechanism of action causes unintended programmed cell death of sebaceous glands, which ultimately leads to disruption of the ocular surface through MGD and loss.6,16-17
Analgesics
Aspirin and ibuprofen continue to be linked to dry eye. Both of these drugs are secreted into the tears, after which they can increase tear evaporation and affect tear film stability. It is important to note that these common OTC medications typically only cause dry eye issues when they are taken in excess of recommended doses.18
Narcotics, including hydrocodone and oxycodone, can also lead to DED due to their anticholinergic properties.8
Cannabis is becoming more widely prescribed, as well as used recreationally; it also should be an etiological consideration for the development of dry eye. It is believed that THC found in cannabis activates the cannabinoid CB1 receptors in the lacrimal gland, which may reduce tear secretion, leading to DED.18
Alcohol, too, is secreted into the tears, where it can cause disrupted tear concentration and shortened tear breakup time.5
Vitamins and Supplements
Most vitamins, including multivitamin supplements, are not associated with DED.19 However, some herbal products and other natural supplements are recognized to contribute to DED. The mechanisms of action are inconclusive, but are likely similar to the sicca effect in dry mouth. Niacin (vitamin B3), echinacea and kava are the three most common herbal products that contribute to DED.11
 |
|
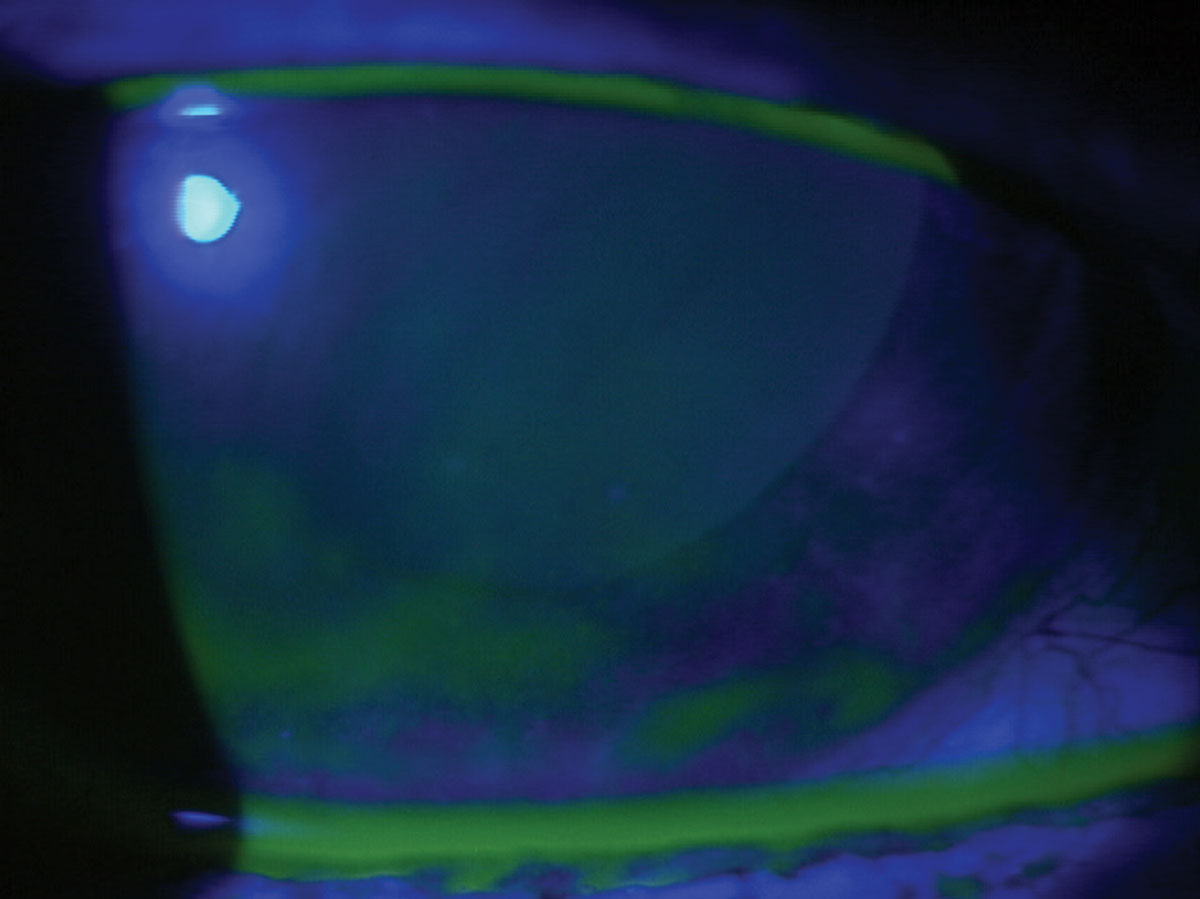
Punctate epithelial erosions in a dry eye patient as revealed by fluorescein dye. Photo: W.R. Buie, OD. Click image to enlarge. |
Topical Medications
Although the focus of this article is systemic medication effects on the ocular surface, we would be remiss not to briefly touch on topical drugs as well.The investigation of DED induced by topical drugs is highly complicated, as patients prone to ocular surface disease (OSD) are typically excluded in clinical trials. Still, many topical medications and excipients have been considered to cause or aggravate DED. These classes of drugs include anti-glaucoma agents, antiviral agents, agents used to treat allergies, decongestants, miotics, mydriatics and cycloplegics, preservatives, anesthetics and NSAIDs. These drugs work at the ocular surface through various mechanisms, ultimately causing toxic, allergic and/or immuno-inflammatory effects. As these medications are delivered directly to the ocular surface, they may also generate a chemical interaction with the lacrimal film, ultimately reducing aqueous secretion, disrupting the lipid layer or causing damage to goblet cells, corneal and conjunctival epithelium, corneal nerves or the eyelids.5
Clinically, it remains difficult to differentiate between iatrogenic effects and spontaneous changes in OSD. Most studied is the prevalence of OSD among patients treated long-term for glaucoma or ocular hypertension. Risk factors for developing DED in these patients are treatment duration, severity of glaucoma, higher intraocular pressure and the use of BAK-containing eye drops. Interestingly, the results of a recent survey showed that nearly 38% of glaucoma patients were using tear substitutes, more than half of which were preserved.5
In diseases like glaucoma where the treatment is mandatory for a sight-threatening condition, discontinuation of therapy is not an option. It is recommended to reduce the number of preserved eye drops. Switching a patient from a preserved to nonpreserved formulation or a different nonpreserved class of medication may significantly improve the appearance of the ocular surface and reduce patient symptoms. Additionally, implanted medication like Durysta or a multitude of surgical options can be considered to spare the ocular surface.5
Interdisciplinary Management and Treatment
Further complicating the assessment of iatrogenic dry eye is the issue of polypharmacy, which is defined as the use of five or more prescription drugs.4 This problem mainly affects older individuals and increases with age. Medication side effects have generally been reported to be three times greater in the older population, which suffers from DED the most.4 As age increases, drug clearance rates decrease, which may increase dry eye–related side effects.19 Furthermore, the interactions that many medications have with each other are difficult to predict and this becomes significantly more complex with the addition of each new medication.4
The underlying disease process should also be a consideration for dry eye symptoms. It is often difficult to conclude whether DED is drug-induced or disease-induced. Despite the complexity and incomplete data, sufficient information is available to show that medication-induced DED is likely underestimated. A population-based study of 2,481 individuals between the ages of 64 and 84 estimated that 62% of dry eye cases in the elderly were caused by systemic medications, rather than the comorbid conditions themselves.21
 |
|
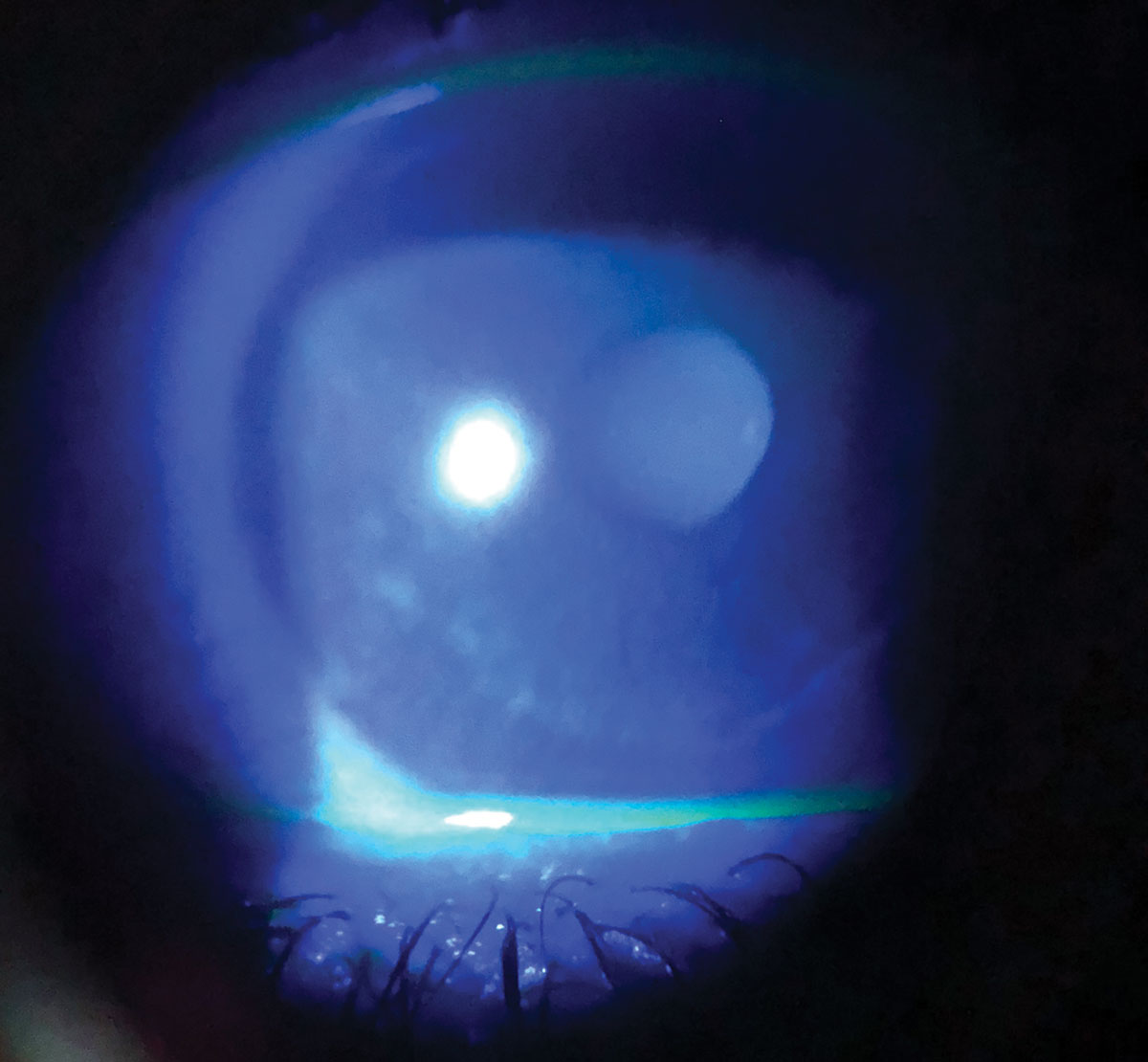
Diffuse corneal staining with fluorescein in a patient with severe dry eye and a history of radial keratotomy. Photo: Irene Frantzis, OD. Click image to enlarge. |
When it is suspected that systemic medications are a factor in a patient’s DED, patient education is the first step. Depending on symptom severity and the medication class that is the suspected aggravator, it may be indicated to suggest an alternative medication that is known to have less side effects of DED. A more localized drug administration method can also be recommended when possible.7 For example, an oral antihistamine regimen can be switched to an antihistamine nasal spray. In these cases, an interdisciplinary and collaborative approach is essential. A patient’s primary care provider and/or prescribing specialist should be contacted if a modification to systemic medication is suggested. While optometrists are encouraged to consider a medication change, that is not always feasible. In scenarios when an alternative medication dose or discontinuation is not recommended, optometrists should treat the DED complications independently.
The DED treatment protocol will be similar no matter which systemic medication is the known or suspected culprit of a patient’s dryness symptoms. Often in DED, combination therapy is required. The TFOS DEWS II Management and Therapy Report provides a step-wise approach to DED management.22 First-line treatment typically involves topical lubricants, including varying viscosity artificial tears, gels and ointments. Tears with less potent or no preservatives are preferred. Drugs with anti-inflammatory properties (e.g., topical steroids, cyclosporine, lifitegrast) and oral doxycycline or azithromycin are other options. Additional treatment choices in more severe cases of DED include punctal plugs, scleral contact lenses and/or serum tears.23
Ultimately, a person cannot choose their comorbidities, but it may be possible to reduce or alter medication therapy to reduce sicca symptoms. A detailed drug review is imperative as providers continue to improve their approach to treatment of DED. The role systemic drugs play in DED is significantly underappreciated, but supporting data is still missing because of the difficulty in separating drug-induced from disease-induced DED.4
Dr. Gilbertson Kuiken is an attending optometrist at the Battle Creek Veterans Affairs Medical Center where she completed her ocular disease residency in 2012. She is a fellow of the American Academy of Optometry and maintains ABCMO certification.
Dr. Vanderpool is a fellow of the American Academy of Optometry. She completed her residency in ocular disease at the Battle Creek Veterans Affairs Medical Center, where she has been an attending optometrist for the past five years. They have no financial disclosures.
1. Weiner G. Dry Eye Disease. American Academy of Ophthalmology EyeNet Magazine. 2018:43-8. 2. Paulsen AJ, Cruickshanks KJ, Fischer ME, et al. Dry eye in the beaver dam offspring study: prevalence, risk factors, and health-related quality of life. Am J Ophthalmol. 2014;157(4):799-806. 3. Craig JP, Nichols KK, Akpek EK, et al. TFOS DEWS II Definition and Classification Report. Ocul Surf. 2017;15(3):276-83. 4. Fraunfelder FT, Sciubba JJ, Mathers WD. The role of medications in causing dry eye. J Ophthalmol. 2012;2012:285851. 5. Gomes JAP, Azar DT, Baudouin C, et al. TFOS DEWS II iatrogenic report. Ocul Surf. 2017;15(3):511-38. 6. Wong J, Lan W, Ong LM, Tong L. Non-hormonal systemic medications and dry eye. Ocul Surf. 2011;9(4):212-26. 7. Fuentes AV, Pineda MD, Venkata KCN. Comprehension of top 200 prescribed drugs in the US as a resource for pharmacy teaching, training and practice. Pharmacy (Basel). 2018;6(2):43. 8. Townsend W. Are Medications the Culprit?. Optometric Management. Accessed September 15, 2022. 9. Weatherby TJM, Raman VRV, Agius M. Depression and dry eye disease: a need for an interdisciplinary approach? Psychiatr Danub. 2019;31(Suppl 3):619-21. 10. Koçer E, Koçer A, Özsütçü M, et al. Dry eye related to commonly used new antidepressants. J Clin Psychopharmacol. 2015;35(4):411-3. 11. Askeroglu U, Alleyne B, Guyuron B. Pharmaceutical and herbal products that may contribute to dry eyes. Plast Reconstr Surg. 2013;131(1):159-67. 12. Bowling E. Which oral meds cause dry eye? Rev Cornea & Cont Lens. June 15, 2011. Accessed September 15, 2022. 13. Maurya RP, Gupta A, Verma S, et al. Sex hormones and dry eye disease: Current update. IP International Journal of Ocular Oncology and Oculoplasy. 2021;7(2):139-50. 14. Chiang JCB, Zahari I, Markoulli M, et al. The impact of anticancer drugs on the ocular surface. Ocul Surf. 2020;18(3):403-17. 15. Wolpert LE, Snieder H, Jansonius NM, et al. Medication use and dry eye symptoms: A large, hypothesis-free, population-based study in the Netherlands. Ocul Surf. 2021;22:1-12. 16. Ruiz-Lozano RE, Hernández-Camarena JC, Garza-Garza LA, et al. Isotretinoin and the eye: a review for the dermatologist. Dermatol Ther. 2020;33(6):e14029. 17. Clayton J. Review Article Dry Eye. N Engl J Med. 2018;372:221-2223. 18. Thayer A, Murataeva N, Delcroix V, Wager-Miller J, et al. THC regulates tearing via cannabinoid CB1 receptors. Invest Ophthalmol Vis Sci. 2020;61(10):48. 19. Aljeaidi M, Keen C, Bell JS, et al. Dry eyes, ocular lubricants and use of systemic medications known or suspected to cause dry eyes in residents of aged care services. Int J Environ Res Public Health. 2020;17(15):5349. 20. Barabino S. Is dry eye disease the same in young and old patients? A narrative review of the literature. BMC Ophthalmol. 2022;22(1):85. 21. Schein OD, Hochberg MC, Muñoz B, et al. Dry eye and dry mouth in the elderly: a population-based assessment. Arch Intern Med. 1999;159(12):1359-63. 22. Jones L, Downie LE, Korb D, et al. TFOS DEWS II Management and Therapy Report. Ocul Surf. 2017;15(3):575-628. 23. Hakim FE, Farooq AV. Dry eye disease: an update in 2022. JAMA. 2022;327(5):478-9. |