Spotlighting OSDMedication, infection, genetics, poor hygiene—these are only a few factors that contribute to ocular surface disease. This month in Review of Optometry, experts weigh in on the risk factors, diagnosis, treatment and management of numerous types of OSD. Check out the other articles featured in the November issue:
|
Demodex mites are the most common ectoparasites on humans and, because of their ubiquity, this species has largely been ignored as human pathogens. Mites are typically harmless and exist in various environments on the body, but when there is an overpopulation, as evidenced by collarettes on the eyelashes, they may go from being benign to causing inflammation and a variety of diseases. They have been associated with acne vulgaris, folliculitis, rosacea, seborrheic dermatitis and hair loss among other conditions.1 Specific to the eye, they have been implicated in diseases of the eyelid and lid margin, including blepharitis and meibomian gland dysfunction (MGD).1
Prevalence
A study published in 2022 involving over 1,000 consecutive eyecare patients found that 57.7% had Demodex blepharitis.2 Other studies have indicated that there is an increase in Demodex blepharitis with age, with the highest rate occurring between ages 20 and 30. This is suspected to be because sebum secretion is at its highest during this period.3 Another spike in occurrence is experienced by patients over the age of 60, likely related to dermatochalasis and skin pH changes.
It also believed that the increase in Demodex blepharitis found in children under the age of five is related to their constant touching of the face, which introduces bacteria to the skin.3 Initial exposure to Demodex occurs at birth or shortly thereafter by skin-to-skin contact between parent and newborn.3 Sebum secretion in 20- to 30-year-olds, dermatochalasis in those over 60 and increased facial touching of young children are all instances of which Demodex overpopulation becomes an increased risk, thus concern broadly spans all age groups. Increased mite population is also more common in patients with rosacea.3
Anatomy of the Enemy
There are two known species of Demodex that affect the eye: Demodex folliculorum and Demodex brevis. Demodex folliculorum organisms are typically 0.30mm to 0.40mm in length and are typically found in clusters around the lash root and lash follicle, feeding on sebum and follicular epithelial cells.1, 3-5 Demodex brevis is slightly smaller at 0.15mm to 0.20mm in length and typically travels alone, preferring to infest the meibomian glands.1,3-5 Both species have semi-translucent, elongated bodies with two segments. They have eight short-clawed legs, allowing them to move at a rate of 8mm to 16mm an hour; they are most often active at night.1,3-5 They can anchor into the hair follicle with the help of their scales, and their pin-like mouths aid in eating skin cells, oils and bacteria.1, 4-5
 |
|
A close-up microscopy photo of a Demodex mite enjoying a meal of paracilia debris. Photo: Patrick Vollmer, OD. Click image to enlarge. |
Demodex typically mate within the hair follicle opening and lay their eggs within the follicle or sebaceous gland. The larvae hatch three to four days later and develop into adults within seven days. They have an approximate lifecycle of 14 days. Their total lifespan is two to three weeks and the dead mites are left to decompose inside the follicle or sebaceous gland.1,4-5
Demodex Causes Trouble
Infestation of these creatures causes both ocular surface disease and meibomian gland dysfunction to worsen. The related mechanisms are believed to be mechanical, bacterial and inflammatory. While Demodex mites consume epithelial cells at the hair follicle, they can cause follicular distention. Microabrasions caused by the mites’ claws further induce epithelial hyperplasia and reactive hyperkeratinization.
D. brevis, preferring the meibomian glands, can cause blocking of the orifices. Their chitinous exoskeleton acts as a foreign body, causing a granulomatous reaction. In theory, this is a potential cause of chalazia and MGD. Demodex carry bacteria within their gut that is released with excrement and in death, as well as harboring bacteria on their surface. Bacteria from either of these sources leads to infection. A delayed hypersensitivity to these proteins carried within the mites’ debris and waste causes an inflammatory response.
Infestation Manifestation
These infestations most commonly lead to patient complaints of itching, burning, tearing, redness, crusting or stickiness of eyelids, although patients often remain asymptomatic. Relying solely on patient complaints to diagnose Demodex infestation can lead to significant misdiagnosis and lack of appropriate treatment.
 |
|
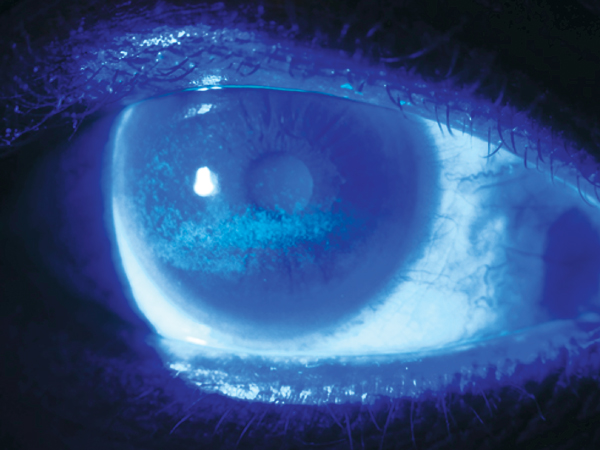
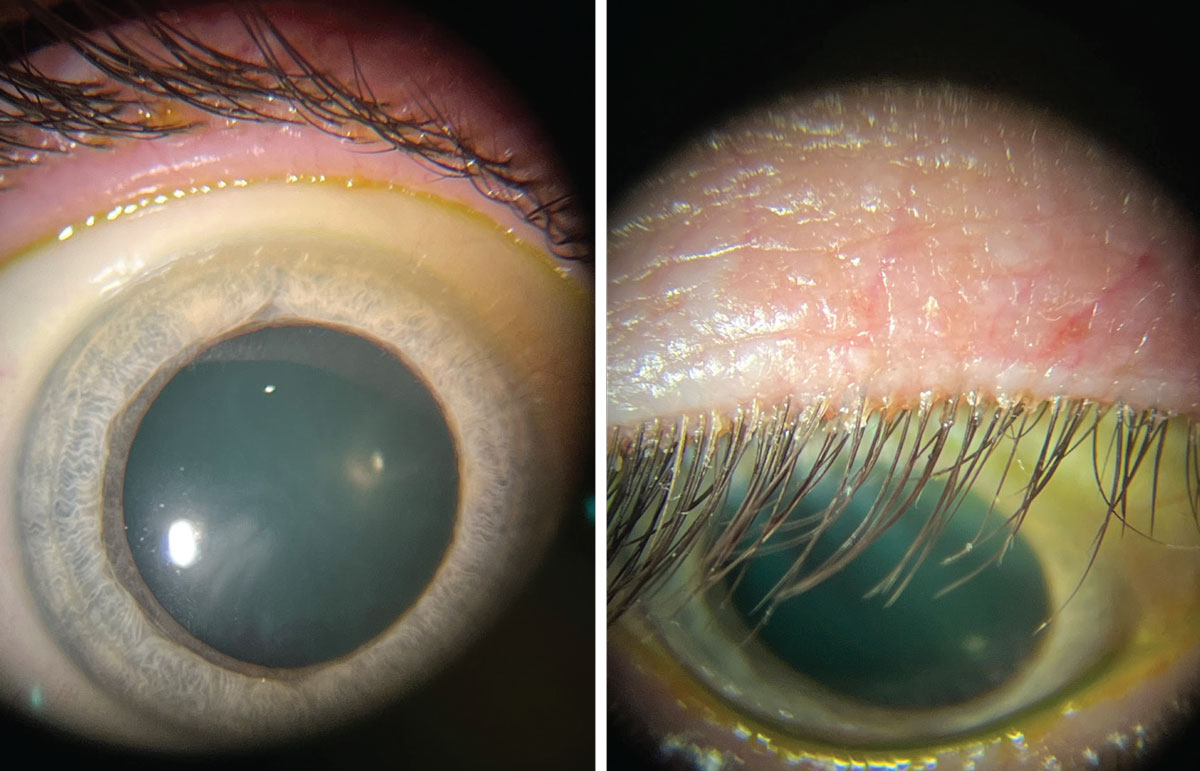
These photos are of the same patient during slit lamp exam. The left photo is of the patient looking straight ahead with minimal identifiable blepharitis. The right photo is the patient looking down with obvious collarettes, indicating a Demodex infestation. Click image to enlarge. |
Collarettes, which are translucent waxy plugs at the base of the lashes, are the pathognomonic sign of an overpopulation of Demodex.6-8 One clinical study showed that Demodex mites were found on 100% of lashes with collarettes.1 They are composed of regurgitated and undigested material, epithelial cells, keratin, mite eggs and digestive enzymes.7,8
The best way to identify collarettes is on slit lamp exam. When examining the lids, remember to look, lift, push and pull. Asking your patient to look down when examining the lid margin can reveal diffuse collarettes and misdirected or missing lashes that otherwise would have gone unseen. Take the time to then look at the lid margin, inspecting for saponification, lid margin debris or biofilm, telangiectasia and lid margin thickening. Next, push on the meibomian glands to grade both expressibility and meibum quality. Studies have shown that MGD is significantly more prevalent in conjunction with Demodex infestations.4
It is worth mentioning that an overpopulation of Demodex and blepharitis can also lead to a higher rate of contact lens intolerance and subsequent dropout in patients. A 2015 study found that 90% of contact lens wearers were positive for Demodex in comparison with only 65% of non-wearers.9 Furthermore, a separate study found that approximately 93% of patients with contact lens intolerance were also positive for Demodex.10
Patient Discussion TipsIt can be difficult for many of us to have the conversation about Demodex without feeling like we are “bugging” out our patients or even ourselves. Unfortunately, there is no way around the truth, but how you deliver the message can make all the difference to help stick a better landing. Here is an example of how to discuss this issue: “Mr. Smith, overall your eyes are looking very healthy on today’s exam. However, I am noticing an overgrowth of bacteria and mites on the eyelashes today. Both mites and bacteria are normally found on the eyelashes, just like bacteria is on our faces and in our mouths. We do things like brushing our teeth and washing our faces to keep them under control. Similarly with the eyes, when these two get out of balance, they can start to cause problems like inflammation or itchiness. I’m going to start you on at-home treatment to help restore that balance.” |
Disease Management
Demodex blepharitis management techniques currently revolve around improving eyelid hygiene. The idea is to control bacterial overgrowth, which can be a food source for the mites. Good lid hygiene using lid sprays or wipes containing hypochlorous acid can help to keep bacterial, fungal and viral pathogens of the eyelids under control.1 Oral doxycycline and azithromycin are effective in use for treatment of MGD.11
Focus has been on tea tree oil for several years as a management option for active Demodex infestations. The mites are resistant to many antiseptic agents, such as alcohol, povidone-iodine and erythromycin.1 Tea tree oil, while not always effective or well-tolerated, is commonly used due to lack of FDA approved treatments and is subsequently the go-to option.1 The oil helps remove the collarettes from the eyelash roots, kill some of the mites and stimulates the buried mites to migrate up to the skin surface.4 Unfortunately, studies have not been able to show full eradication of Demodex after four weeks of tea tree oil–derived therapy, even when blepharoexfoliation was used to debulk the infestation.1,4
Another promising management option is okra extract. It has antioxidative and anti-inflammatory effects on the Akt-mediated NF-kB pathway involved in dry eye and blepharitis.12 One study compared the use of okra eyelid patches and tea tree oil eyelid patches, finding similar survival time of the Demodex in both groups at 115.3 minutes and 106.7 minutes, respectively.12 However, tolerance in the okra group was considerably better than that of the tea tree oil subjects.12 Thus, okra extract seems a management technique that may be better suited for sensitive patients.
Manuka honey is known for its anti-inflammatory and antimicrobial properties because of its low pH, high osmolarity and high methylglyoxal (MGO) content.13 MGO is found in other honey varietals but is higher in concentration in New Zealand Manuka honey.13 A 2020 study used Manuka eye cream overnight for three months in patients with blepharitis, finding significant improvements in ocular surface symptomology, tear film stability, bacterial load and signs of ocular Demodex infestation.13
On the Horizon
Data from two double masked, randomized Phase III pivotal studies, comprising 833 patients, was released earlier this year on studies of the use of lotilaner ophthalmic solution 0.25% (TP-03, Tarsus) for this condition. The researchers regarded the intervention as an effective and safe treatment for Demodex blepharitis.14 Patients were given one drop of TP-03 twice a day for six weeks and were required to have at least 10 collarettes per lid at the time of enrollment.14
In the most recent study, Saturn-2, the primary endpoint of complete collarette cure (zero to two collarettes per lid at day 43) was achieved in 56% of patients, and an astounding 89% of patients had 10 or fewer collarettes.14 The secondary endpoint of mite eradication (zero mites per lash) was met in 52% of patients, while lid erythema cure was found in 31.1% of patients.14 The treatment was well tolerated by patients, as 91% reported that drop comfort was neutral to very comfortable.14
This is very promising data, and soon we may have a better treatment option for our patients with Demodex blepharitis that will have proven safety, tolerability and effectiveness in collarette reduction and mite eradication. Until then, encouraging better lid hygiene and recommending blepharoexfoliation can provide some measure of relief.
Dr. Koetting practices at MD/OD practice Hines Sight in Denver, CO. Her primary focus is in anterior segment and ocular surface disease, neuro-optometry and perioperative care. Dr. Koetting is fellow in the American Academy of Optometry, a diplomate of the American Board of Optometry, active member of AOA and has served as both local and state officers in AOA. She was named young optometrist of the year in 2019 by the state of Virginia, receiving the Vanguard of the Year Award. Dr. Koetting lectures locally, nationally and internationally at conferences and has written for multiple publications.
1. Fromstein SR, Harthan JS, Patel J, Opitz DL. Demodex blepharitis: clinical perspectives. Clin Optom (Auckl). 2018;10:57-63. 2. Trattler W, Karpecki P, Rapoport Y, et al. The prevalence of Demodex blepharitis in US eye care clinic patients as determined by collarettes: a pathognomonic sign. Clin Ophthalmol. 2022;16:1153-64. 3. Rather PA, Hassan I. Human Demodex mite: the versatile mite of dermatological importance. Indian J Dermatol. 2014;59(1):60-6. 4. Luo X, Li J, Chen C, Tseng S, Liang L. Ocular demodicosis as a potential cause of ocular surface inflammation. Cornea. 2017;36(Suppl 1):S9. 5. Jalbert I, Rejab S. Increased numbers of Demodex in contact lens wearers. Optom and Vis Sci. 2015;92(6):671-8. 6. Gao YY, Di Pascuale MA, Li W, et al. High prevalence of Demodex in eyelashes with cylindrical dandruff. Invest Ophthalmol Vis Sci. 2005;46(9):3089-94. 7. Zhang AC, Muntz A, Wang MTM, Craig JP, Downie LE. Ocular Demodex: a systematic review of the clinical literature. Ophthalmic Physiol Opt. 2020;40:389-431. 8. Nicholls S, Oakley CL, Tan A, Vote BJ. Demodex species in human ocular disease: new clinicopathological aspects. Int Ophthalmol. 2017;37(1):303-12. 9. Jalbert I, Rejab S. Increased numbers of Demodex in contact lens wearers. Optom Vis Sci. 2015;92(6):671-8. 10. Tarkowski W, Moneta-Wielgoś J, Młocicki D. Demodex sp. as a potential cause of the abandonment of soft contact lenses by their existing users. Biomed Res Int. 2015;2015. 11. De Benedetti G, Vaiano AS. Oral azithromycin and oral doxycycline for the treatment of meibomian gland dysfunction: a 9-month comparative case series. Indian J Ophthalmol. 2019;67(4):464-71. 12. Liu W, Gong L. Anti-demodectic effects of okra eyelid patch in Demodex blepharitis compared with tea tree oil. Exp Ther Med. 2021;21(4):338. 13. Craig JP, Cruzat A, Cheung IMY, Watters GA, Wang MTM. Randomized masked trial of the clinical efficacy of MGO Manuka Honey microemulsion eye cream for the treatment of blepharitis. Ocul Surf. 2020;18(1):170-7. 14. Tarsus Pharmaceuticals https://ir.tarsusrx.com/news-releases/news-release-details/tarsus-announces-positive-topline-data-saturn-2-phase-3-second. May 2, 2022. Accessed September 27, 2022. |