 |
An 81-year-old woman presented with a three-day history of vision loss and mild ocular irritation in her right eye.
Her medical history included moderate primary open-angle glaucoma OU that was medically uncontrolled in her right eye. Her left eye had undergone trabeculectomy several years earlier and was stable. She had received an aqueous shunting procedure with conjunctival grafting OD several months earlier, which required two surgical revisions, and subsequently developed persistent inflammation and cystoid macular edema unresponsive to topical therapy.
She then underwent four surgical vitreal placements of Ozurdex implants (dexamethasone, Allergan), the most recent of which was one month prior to her emergency visit. She was still using timolol 0.5% BID in her right eye.
Her entering visual acuity in her right eye was hand motion at two feet (previously 20/40). Biomicroscopic evaluation revealed the cause of her reduced vision. She had a large central corneal abrasion and underlying corneal edema encompassing the central 50% of the cornea. While a simple corneal abrasion would normally be easily treated or even self-resolving, her history of multiple invasive procedures combined with surgically induced chronic inflammation, along with very minimal ocular discomfort, was cause for concern.
Corneal sensitivity testing revealed virtually no sensation. This suggested that she didn’t have a simple corneal abrasion but rather a more complicated neurotrophic keratitis.
A Lack of Feeling
Neurotrophic keratitis is a degenerative corneal condition due to reduced neural innervation.1-11 Neurotrophic keratitis is classified into three overlapping stages: stage 1 involves general epithelial alterations; stage 2 involves persistent epithelial defects; and stage 3 involves frank corneal ulceration.
A characteristic of all stages is decreased corneal sensation. Because of this, patients rarely complain of discomfort, and there is a significant discrepancy between clinical findings and subjective symptoms. Disease progression is often unnoticed by the patient but results in severe vision loss due to scarring and corneal perforation.
Trauma, tumors, inflammatory lesions, herpetic infections, chronic corneal exposure, amyloidosis and surgical procedures have all been capable of initiating the cascade.8 Abuse of topical ophthalmic anesthetics is also a strong cause, as well as exposure to smoke from crack cocaine.
One should also consider the effect of iatrogenic disease on persistent epithelial defects. Sometimes the corneal epithelium cannot heal when exposed to multiple medications and their preservatives in high doses. Damage to the trigeminal nerve anywhere between its origin in the midbrain and the branches within the cornea can cause neurotrophic keratitis.1-6
The corneal epithelium may demonstrate breakdown even in the absence of desiccation, active microbial infection or direct traumatic insult.5 There is no gender predilection. Since neurotrophic keratitis is a result from injury, infection or inflammation, its course depends on the identification and treatment of the underlying cause, along with anti-infective, anti-inflammatory and immunologic support for the cornea itself.9-13
The corneal epithelium responds to injury by synthesizing several cytokines, growth factors and tissue-remodeling molecules.14 Proinflammatory cytokines have been implicated in the inflammation that follows corneal epithelial injury. Any poorly regulated corneal reactions that occur after insult can retard healing. In turn, persistent corneal epithelial defects and inflammation may lead to ocular morbidity and permanent visual loss.14
Physical discomfort that is disparately low compared with the clinical findings should raise suspicion for neurotrophic keratitis.
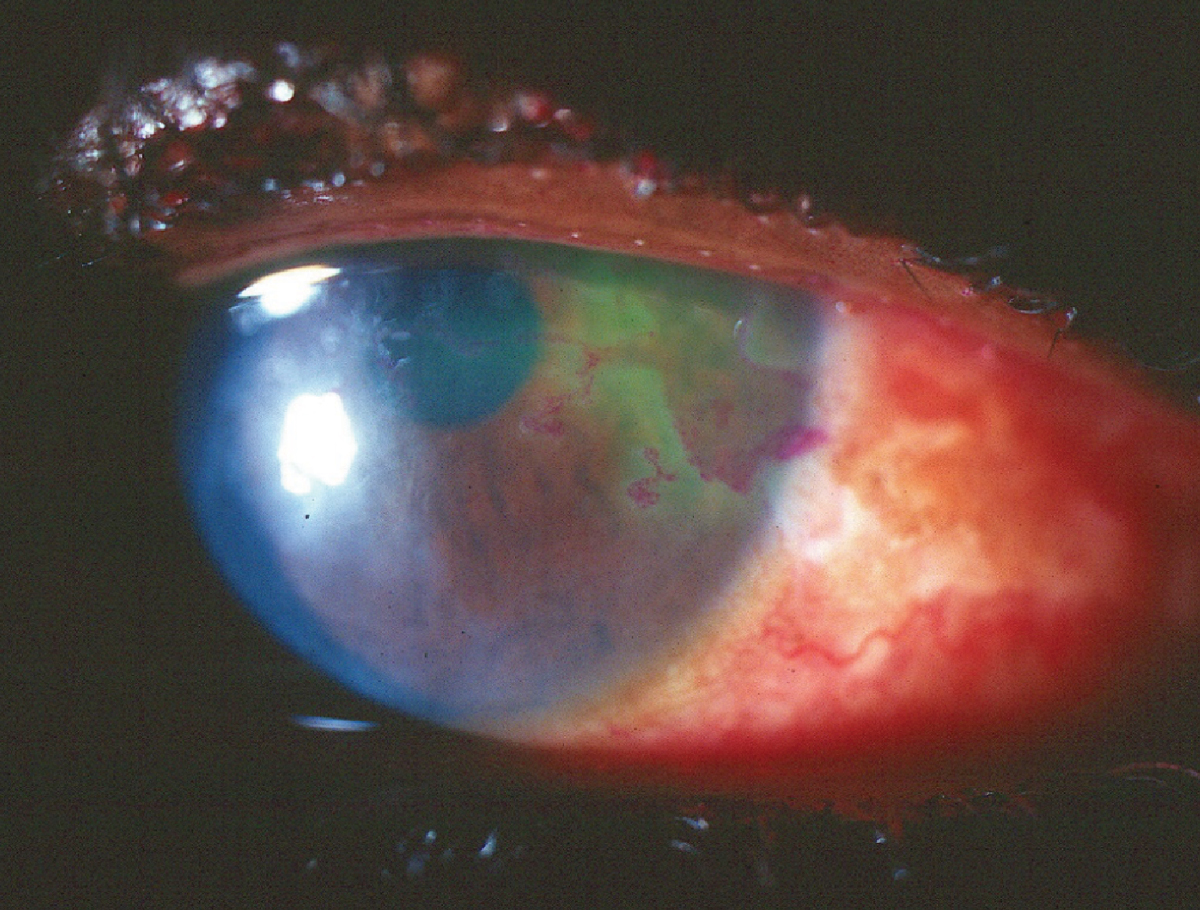 |
|
Neurotrophic corneal ulcer from herpes simplex. Click image to enlarge. |
Treatments
Evaluation of corneal sensitivity and tear film function is important diagnostic data.2 Initial management includes appropriate topical cycloplegia, depending upon the severity of the accompanying inflammation. If there is significant epitheliopathy, use a topical antibiotic such as moxifloxacin QID to Q2H to prevent secondary infection of the compromised cornea. Prescribe copious non-preserved artificial tears as well as a bandage soft contact lens to support epithelial healing.
Punctal plugs can also be used to help ensure the cornea receives adequate lubrication. Eyelid patching and tarsorrhaphy can also be used to promote corneal healing. Neurotrophic corneas that are not treated aggressively can progress through stromal lysis to perforation.5
An alternate therapy that has been successful in the management of neurotrophic keratitis involves the placement of an amniotic membrane.15-17 Additionally, autologous serum can also be beneficial in promoting corneal healing.18,19 Autologous serum eye drops are useful in corneal re-epithelialization when a patient’s serum is diluted by 20% or 50% and used every three to four hours daily.20
Recently, there has been a step forward with the development of Oxervate (cenegermin-bkbj 0.002%, Dompé), the first therapy approved for the treatment of neurotrophic keratitis.
Cenegermin is a recombinant human nerve growth factor that promotes healing in neurotrophic keratitis. Nerve growth factors act directly on corneal epithelial cells and have been shown to support corneal re-innervation.21 These mechanisms are essential to overcome the degenerative cycle of neurotrophic keratitis.
Cenegermin is typically used as a first-line treatment for patients with stage 2 or 3 neurotrophic keratitis who have not responded to other conventional nonsurgical treatments for two weeks. One drop in the affected eye(s), six times per day at two-hour intervals, for eight weeks is recommended.22-24
Clinical results from cenegermin have been impressive. At eight weeks, complete healing has been seen in 75% of patients compared with 43% in the vehicle placebo group.24
Patient Follow-Up
The patient presented here was educated about the likelihood of a protracted course of therapy. An amniotic membrane was avoided due to the aqueous shunt with grafting previously performed in that eye. She was prescribed copious non-preserved artificial tears and a topical antibiotic (moxifloxacin QID), and a soft bandage contact lens was placed on her eye. When she returned the next day, she had a diffuse epitheliopathy, but the central abrasion had decreased to involve now only 10% of the central cornea (down from 50%). She again manifested virtually no corneal sensation to cotton wisp testing.
The patient was continued on copious tears and a hypertonic saline solution, but a bandage contact lens was not used. Over several days, her epithelial defect did close, but she had persistent epitheliopathy, minimal corneal sensation and an irregular area of negative staining in the shape of the original abrasion, indicating a very fragile cornea.
Due to the severity of the corneal hypoesthesia, autologous serum tears were deferred in favor of the more condition-specific treatment, cenergermin. She was maintained on preservative-free artificial tears until she was able to move through the process of obtaining the medication, which involved insurance determination, prior authorization and patient assistance grant submission (due to the high cost of cenergermin). She returned two weeks after obtaining cenergermin and using it at the recommended dosing of six times per day. She reported that instillation of her glaucoma medication in that eye now caused mild stinging. Commensurate with this history was an increase in sensation upon corneal sensitivity testing. Her acuity had improved to 20/60, and her cornea, while manifesting a grade 2 diffuse epitheliopathy, showed no evidence of a focal corneal defect. She is currently completing her course of cenergermin.
Dr. Sowka is an attending optometric physician at Center for Sight in Sarasota, FL, where he focuses on glaucoma management and neuro-ophthalmic disease. He is a consultant and advisory board member for Carl Zeiss Meditec and Bausch Health.
1. Cursiefen C, Seitz B, Kruse FE. Neurotrophic keratitis. Ophthalmologe. 2005;102(1):7-14. 2. Bonini S, Rama P, Olzi D, et al. Neurotrophic keratitis. Eye (Lond). 2003;17(8):989-95. 3. Nishida T. The cornea: stasis and dynamics. Nippon Ganka Gakkai Zasshi. 2008;112(3):179-212. 4. Nguyen VT, Hwang TN, Shamie N, et al. Amyloidosis-associated neurotrophic keratopathy precipitated by overcorrected blepharoptosis. Cornea. 2009;28(5):575-6. 5. Pushker N, Dada T, Vajpayee RB, et al. Neurotrophic keratopathy. CLAO J. 2001;27(2):100-7. 6. Reynolds SA, Kabat AG. Therapeutic options for the management of early neurotrophic keratopathy: a case report and review. Optometry. 2006;77(10):503-7. 7. John D, Thomas M, Jacob P. Neurotrophic keratitis and congenital insensitivity to pain with anhidrosis-a case report with 10-year follow-up. Cornea. 2011;30(1):100-2. 8. Jarade EF, El-Sheikh HF, Tabbara KF. Indolent corneal ulcers in a patient with congenital insensitivity to pain with anhidrosis: a case report and literature review. Eur J Ophthalmol. 2002;12(1):60-5. 9. Yagev R, Levy J, Shorer Z, et al. Congenital insensitivity to pain with anhidrosis: ocular and systemic manifestations. Am J Ophthalmol. 1999;127(3):322-6. 10. Okada Y, Reinach PS, Kitano A, et al. Neurotrophic keratopathy; its pathophysiology and treatment. Histol Histopathol. 2010;25(6):771-80. 11. Nishida T, Yanai R. Advances in treatment for neurotrophic keratopathy. Curr Opin Ophthalmol. 2009;20(4):276-81. 12. Kaufman SC. Anterior segment complications of herpes zoster ophthalmicus. Ophthalmology. 2008;115(2 Suppl):S24-32. 13. Holland EJ, Schwartz GS. Classification of herpes simplex virus keratitis. Cornea. 1999;18(2):144-54. 14. Sosne G, Qiu P, Kurpakus-Wheater M. Thymosin beta-4 and the eye: I can see clearly now the pain is gone. Ann NY Acad Sci. 2007;112(9):114-22. 15. Kruse FE, Cursiefen C. Surgery of the cornea: corneal, limbal stem cell and amniotic membrane transplantation. Dev Ophthalmol. 2008;41(1):159-70. 16. Ting DSJ, Henein C, Said DG, Dua HS. Amniotic membrane transplantation for infectious keratitis: a systematic review and meta-analysis. Sci Rep. 2021;11(1):13007. 17. Kalogeropoulos D, Geka A, Malamos K, et al. New therapeutic perceptions in a patient with complicated herpes simplex virus 1 keratitis: a case report and review of the literature. Am J Case Rep. 2017;18:1382-9. 18. Ripa M, Jabbehdari S, Yazdanpanah G, et al. The Role of Multisystem Disease in Composition of Autologous Serum tears and ocular surface symptom improvement. Ocul Surf. 2020;18(3):499-504. 19. Semeraro F, Forbice E, Braga O, Bova A, et al. Evaluation of the efficacy of 50% autologous serum eye drops in different ocular surface pathologies. Biomed Res Int. 2014;2014:826970. 20. Vaidyanathan U, Hopping GC, Liu HY, et al. Persistent corneal epithelial defects: a review article. Med Hypothesis Discov Innov Ophthalmol. 2019;8(3):163-76. 21. Sheha H, Tighe S, Hashem O, Hayashida Y. Update On Cenegermin Eye Drops In The Treatment Of Neurotrophic Keratitis. Clin Ophthalmol. 2019;13:1973-80. 22. Ahuja AS, Bowden FW 3rd, Robben JL. A novel treatment for neurotrophic corneal ulcer using topical cenegermin (Oxervate) containing recombinant human nerve growth factor. Cureus. 2020;12(11):e11724. 23. Dana R, Farid M, Gupta PK, et al. Expert consensus on the identification, diagnosis and treatment of neurotrophic keratopathy. BMC Ophthalmol. 2021;21(1):327. 24. Pflugfelder SC, Massaro-Giordano M, Perez VL, et al. Topical recombinant human nerve growth factor (cenegermin) for neurotrophic keratopathy: a multicenter randomized vehicle-controlled pivotal trial. Ophthalmology. 2020;127(1):14-26. |

